* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Direct Comparison between T Cell Control of Hepatitis B Virus +CD8
Survey
Document related concepts
Transcript
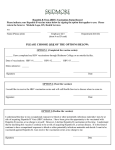
CD8+ T Cell Control of Hepatitis B Virus Replication: Direct Comparison between Cytolytic and Noncytolytic Functions This information is current as of August 12, 2017. Sandra Phillips, Shilpa Chokshi, Antonio Riva, Alexander Evans, Roger Williams and Nikolai V. Naoumov J Immunol 2010; 184:287-295; Prepublished online 30 November 2009; doi: 10.4049/jimmunol.0902761 http://www.jimmunol.org/content/184/1/287 References Subscription Permissions Email Alerts http://www.jimmunol.org/content/suppl/2009/12/08/jimmunol.090276 1.DC1 This article cites 46 articles, 19 of which you can access for free at: http://www.jimmunol.org/content/184/1/287.full#ref-list-1 Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2010 by The American Association of Immunologists, Inc. All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. Downloaded from http://www.jimmunol.org/ by guest on August 12, 2017 Supplementary Material The Journal of Immunology CD8+ T Cell Control of Hepatitis B Virus Replication: Direct Comparison between Cytolytic and Noncytolytic Functions Sandra Phillips, Shilpa Chokshi, Antonio Riva, Alexander Evans, Roger Williams, and Nikolai V. Naoumov1 H epatitis B virus (HBV) is a hepatotropic, noncytopathic virus that can cause hepatitis, cirrhosis, and hepatocellular carcinoma. Approximately 350 million people worldwide are chronically infected with HBV with various levels of viral replication (1–3). It is now established that the host immune response plays a major role in the outcome of HBV infection (4– 7). During acute HBV infection, the development of a strong cellular immune response, directed to multiple viral Ags, is associated with the resolution of HBV infection and life-long antiviral immunity. In contrast, the presence of a weak and narrowly focused cellular immune response is unable to control HBV replication, leading to viral persistence and progressive liver injury. HBV-specific CD8+ T cells are believed to play a critical role in the control of HBV replication but are also implicated in the pathogenesis of the disease by destruction of infected liver cells (1, 3, 8, 9). This Ag- specific killing of infected hepatocytes was initially believed to be the main mechanism by which CD8+ T cells control HBV infection. However, this concept was challenged by a series of studies in HBV transgenic mice (10, 11) and HBV-infected chimpanzees (12, 13), which revealed the mechanism of noncytolytic inhibition of HBV replication, i.e., that HBVInstitute of Hepatology, University College London, London, U.K. 1 Current address: Immunology and Infectious Diseases, Novartis Pharma AG, Basel, Switzerland. Received for publication August 20, 2009. Accepted for publication November 1, 2009. Address correspondence and reprint requests to Sandra Phillips, Institute of Hepatology, University College London, 69-75 Chenies Mews, London WC1E 6HX, U.K. Email address: [email protected] The online version of this article contains supplemental material. Abbreviations used in this paper: HBV, hepatitis B virus; HBc18–27, HBcore18–27 epitope; ICS, intracellular cytokine staining; LDH, lactate dehydrogenase; PD-1, programmed death-1. Copyright Ó 2010 by The American Association of Immunologists, Inc. 0022-1767//$16.00 www.jimmunol.org/cgi/doi/10.4049/jimmunol.0902761 specific CD8+ T cells could inhibit HBV replication without lysis of infected hepatocytes. Upon activation, these immune cells were shown to produce cytokines, such as IFN-g and TNF-a, which suppressed HBV gene expression and replication without destroying the infected hepatocytes. This key antiviral mechanism of noncytolytic HBV control, mediated by CD8+ T cells, has not been fully examined using human effector and target cells; in particular, the relative involvement of the two processes, a direct killing of HBV-infected cells and the intracellular HBV inactivation without cell lysis, is not well understood. In this study, we established an in vitro coculture model to determine the relative contribution and balance between the cytolytic and noncytolytic effector functions that HBV-specific CD8+ T cells use to control HBV replication. Materials and Methods Culture of 2.2.15 cells The human hepatoma cell line 2.2.15, derived from HepG2 cells, is stably transfected with HBV DNA and supports full HBV replication with production and secretion of viral Ags and infectious virions (14). In a preliminary experiment, we confirmed that 2.2.15 cells are HLA-A2 positive and, therefore, can express A2-restricted HBV peptides within MHC class I. For this purpose, 2.2.15 cells were stained with FITC-labeled Ab to A2 (Serotec, Oxford, U.K.) and analyzed by FACSort using Cell Quest software (BD Biosciences, Oxford, U.K.). For cell culture, 2.2.15 cells were seeded in 24-well tissue culture plates and grown for 3 d to reach confluency under positive selection with 0.4 mg/ml Geneticin (Invitrogen, Paisley, U.K.) in DMEM (Invitrogen) containing 10% FCS (Invitrogen), 500 U/ml penicillin, 500 mg/ml streptomycin (Invitrogen), and 2 mM Lglutamine (Invitrogen). Generation of HBV-specific CD81 T cell line and clone PBMCs were isolated by standard density centrifugation from patients who were positive for HLA-A2 and who spontaneously cleared hepatitis B surface Ag after acute hepatitis B. The HLA-A2–restricted epitope between amino acids 18–27 of the HBV nucleocapsid has been established as the key immunodominant epitope associated with control of HBV replication Downloaded from http://www.jimmunol.org/ by guest on August 12, 2017 Resolution of hepatitis B virus (HBV) infection was believed to be attributed to the cytotoxic T cell–mediated killing of infected hepatocytes. However, studies in HBV transgenic mice and HBV-infected chimpanzees revealed that T cell control of HBV replication also involves cytokine-mediated noncytolytic mechanisms. The relative role of cytolytic and noncytolytic functions of virus-specific CD8+ T cells during interaction with HBV-producing hepatocytes is not well understood. By using HLA-A2 matched effector cells (CD8+ T cell line or clone) and target cells supporting full HBV replication, we demonstrate that virusspecific CD8+ T cells can inhibit HBV replication in HBV-producing hepatocytes with minimal cell lysis. Although CD8+ T cells kill a fraction of infected cells, this effect is minimal, and most of the viral inhibition is mediated by noncytolytic mechanisms. CD8+ T cells produce an array of cytokines, among which IFN-g and TNF-a are responsible for HBV inactivation in the target cells. Blockade of IFN-g and TNF-a abrogated the noncytolytic inhibition of HBV, indicating that these two cytokines mediate the control of HBV by noncytolytic mechanisms. Furthermore, treatment of the HBV-producing hepatocytes with rIFN-g and rTNFa resulted in an efficient suppression of viral replication without cytotoxicity. In contrast, coculture of the same target cells with activated HLA-mismatched mitogen-activated lymphomononuclear cells caused a marked cytolytic effect and was less effective in HBV control. These results provide direct evidence that virus-specific CD8+ T cells efficiently control HBV replication by noncytolytic mechanisms, and this effect is mediated by IFN-g and TNF-a. The Journal of Immunology, 2010, 184: 287–295. 288 CYTOLYTIC VERSUS NONCYTOLYTIC HBV INHIBITION Flow cytometry For ICS, 1 3 106 CD8+ T cells were incubated with HBc18–27 peptide or mixed with 2.2.15 cells for 6 h at 37˚C with 10 mg/ml brefeldin A (SigmaAldrich). The cells were stained with Cy-chrome–conjugated anti-CD8 Ab (BD Biosciences) for 20 min at 4˚C. Subsequently, the cells were permeabilized and fixed with Cytofix/Cytoperm (BD Biosciences) for 20 min at 4˚C, stained with FITC–anti-human IFN-g (BD Biosciences), and then analyzed by flow cytometry. The frequency of CD8+ T cells specific for HBc18–27 peptide was also determined. The CD8+ T cell line was stained with core18–27 HLA class I tetramer (Proimmune) and PerCP-conjugated anti-CD8 Ab (BD Biosciences). CD8+ T cell clone was stained with APCcore18–27 HLA class I pentamer (Proimmune) and APC–Cy7-conjugated anti-CD8 Ab (BD Biosciences). For the degranulation, CD8+ T cell clone was cultured for 5 h with PMA/ionomycin and HBc18–27 peptide in the presence of CD107a PECy5 (BD Biosciences). Following incubation, the cells were washed and stained with PerCP-conjugated anti-CD8 Ab (BD Biosciences). + Coculture of HBV-specific CD8 T cells and 2.2.15 cells + The CD8 T cell line or the T cell clone (effectors cells) were added to the confluent 2.2.15 cells (target cells). Two different systems of cell-to-cell interactions were investigated in parallel: direct effector/target contact, whereby the CD8+ T cells were stimulated by recognizing the viral peptides expressed on the surface of 2.2.15 cells, and indirect effector/target contact, whereby the effector and target cells were separated by a 0.4-mm membrane (Marathon, London, U.K.), which allowed the passage of soluble factors only. In this second system, CD8+ T cells were stimulated by coculture with the corresponding HBc18–27 peptide at 1 mM (Fig. 1). EBV–transformed B cells were used as APCs in the insert and were added to the CD8+ T cells at a 1:1 ratio. The CD8+ T cells and 2.2.15 cells were cocultured for 3, 24, or 48 h using E:T ratios of 1:300, 1:60, and 1:6. As controls, 2.2.15 cells were cultured alone, and CD8+ T cells were cultured in the insert but without HBV peptide. At the end of the experiments, the target cells and the corresponding culture supernatants were harvested for measurement of the cytokine levels, cytotoxicity, and HBV DNA quantitation. Neutralization of IFN-g or TNF-a Anti–IFN-g and anti–TNF-a neutralizing mAbs (R&D Systems) were added individually or in combination to the direct or indirect cocultures at a 1:6 ratio. A neutralization dose of 36 or 0.9 mg/ml was used, respectively, according to the manufacturer’s guidelines. After 24 or 48 h, the cells and the supernatants were collected for HBV DNA quantitation. The complete neutralization of the cytokines in the supernatants after adding the respective Abs was confirmed by cytokine bead arrays (BD Biosciences). Cytokine production The levels of IFN-g, TNF-a, IL-10, -6, -8, -2, and -5, and FasL in the coculture supernatants of effector and target cells were assessed by commercially available ELISA assays (R&D Systems) and cytokine bead array. Cytotoxicity of target cells The cytotoxicity of the target 2.2.15 cells was assessed by measuring the lactate dehydrogenase (LDH) release in the supernatants at the end of each incubation period using a commercially available enzyme immunoassay (Roche Diagnostics, Bell Lane, U.K.). The results were expressed as a percentage of cytotoxicity, according to the manufacturer’s instructions. In summary, the percentage of cytotoxicity was measured by including several controls in the assay: a low-level LDH control, represented by the 2.2.15 cells cultured alone; a high-level LDH control, represented by 2.2.15 cells treated with Triton X-100 to lyse the cells and induce maximum LDH release; and culture medium alone used as a background control, which was subtracted from all test samples to provide the experimental value. The resulting values were substituted in the following equation: (experimental value 2 low control)/(high control 2 low control) 3 100. In addition, we assessed the proportion of apoptotic target cells using the TACS Annexin V–FITC Apoptosis detection kit (R&D Systems). HBV DNA quantitation HBV replication was assessed by quantitation of viral nucleocapsid– associated HBV DNA (cytoplasmic) and HBV DNA from secreted viral particles (supernatant). Nucleocapsid-associated HBV DNA was extracted and quantified by TaqMan real-time PCR (ABI Prism 7700, Applera, Warrington, U.K.), as previously described (17). Secreted HBV DNA was extracted using QIAamp DNA minikit (Qiagen, Sussex, U.K.) and also quantified by TaqMan. The sensitivity of the assay was verified in each run using a set of positive controls: serial dilutions of HBV DNA plasmid, as well as the EuroHep HBV DNA standard (18). The range of detection was from 1010 to 101 HBV DNA copies/ml with the plasmid and 108 to 102 copies/ml with the EuroHep standard. Coculture of HLA-mismatched effector cells and 2.2.15 cells We also evaluated the effect of HLA-mismatched, mitogen-activated lymphomononuclear cells on HBV DNA levels and target cell death. For this purpose, PBMCs from patients negative for HLA-A2 and with chronic hepatitis B were stimulated with 10 mg/ml PHA (Sigma-Aldrich). PHAstimulated PBMCs at two concentrations (2 3 105 and 1 3 106) were cocultured in direct contact and in parallel in indirect contact with target 2.2.15 cells for 48 h. The supernatant and the target cells were harvested at the end of the coculture period. The IFN-g level and target cell lysis were measured, and HBV DNA was quantitated. Statistical methods The differences among groups were evaluated using one-way ANOVA. Subsequently, the difference between two groups was calculated with the Tukey post hoc test only if ANOVA was statistically significant (p , 0.05). The Tukey post hoc test was also considered significant at p , 0.05. The correlation analysis between target cell death (i.e., cytotoxicity level) and HBV DNA levels in the supernatants was evaluated by the Pearson correlation coefficient. Results Characterization of HBc18–27-specific CD8+ T cells The HBc18-27-specific CD8+ T cells cocultured with the 2.2.15 cells in the in vitro model were first characterized (Fig. 1). The frequency of HBc18–27 pentamer–positive and IFN-g–producing CD8+ T cells was investigated. After stimulation with 2.2.15 cells or HBc18–27 peptide, 65% and 30% of the CD8+ T cell line, respectively, produced IFN-g (Supplemental Fig. 1A). Pentamer staining of the CD8+ T cell clone showed that 99% of the lymphocytes were HBc18–27 positive (Supplemental Fig. 1B), and .70% of the cells degranulated when activated with PMA/ionomycin and HBc18–27 peptide (Supplemental Fig. 1C). Cytokine production The CD8+ T cell line produced high levels of IFN-g in a time- and E: T ratio–dependent manner following the direct (p # 0.001) and indirect (p # 0.001, p # 0.05, and p # 0.005) coculture with 2.2.15 cells (Fig. 2A). TNF-a was detectable in the culture supernatants from the direct system at an E:T ratio of 1:6 (p # 0.001), but was below the limit of detection (4.4 pg/ml) at E:T ratios of 1:300 or 1:60 Downloaded from http://www.jimmunol.org/ by guest on August 12, 2017 (15). Therefore, CD8+ T cell line and a clone specific for HBV core 18–27 epitope (HBc18–27) were generated and used in the current study. PBMCs cultured at 3 3 105/well in supplemented RPMI 1640/10% human AB serum, were stimulated with 10 mg/ml synthetic HBc18–27 (FLPSDFFPSV) (Cambridge Research Biochemicals, Cleveland, U.K). rIL-2 (R&D Systems, Abingdon, U.K.) was added at 30 U/ml on days 3 and 6 of culture. After 10 d of stimulation, the specificity of the lines was ascertained by using a specific 18–27 tetramer that allowed enumeration of the number of epitope-specific CD8+ T cells. The cells were stained with core18–27 HLA class I pentamer (Proimmune, Oxford, U.K.) and PerCP-conjugated antiCD8 Ab (BD Biosciences). The ability of these T cells to produce IFN-g in response to the core 18–27 peptide and when cultured with 2.2.15 cells was determined by IFN-g intracellular cytokine staining (ICS), as described below. Then CD8+ T cells were subjected to a second round of peptide stimulation and cultured as described above for an additional 10 d. Then the cells were seeded in 96-well plates at 1, 10, 50, and 100 cells/well and stimulated every 2 wk with 1 mg/ml PHA (Sigma-Aldrich, Dorset, U. K.), 30 U/ml IL-2, 10 ng/ml IL-15, and 1 3 105/ml allogenic-irradiated PBMCs used as feeder cells. Each well was tested every 2 wk for expansion by ICS, and a cell line with 65% specificity was developed. An HBc18–27-specific CD8+ T cell clone that also recognized core 18–27 epitope was also used in this study (16). The cloned CD8+ T cells were maintained by weekly stimulation with irradiated PBMCs plus PHA (Sigma-Aldrich) in the presence of IL-2, -7, and -15. The clone was also tested for degranulation, as described below. The Journal of Immunology 289 FIGURE 1. Diagram of the two in vitro coculture systems. Direct system: CD8+ T cells and 2.2.15 cells are in direct contact. Indirect system: CD8+ T cells stimulated with HBc18–27 peptide and EBV-transformed B cells (EBV B) were placed in an insert above the 2.2.15 cells. The cytokines produced by the activated CD8+ T cells can pass through the membrane of the insert. were identified in the indirect system (Supplemental Fig. 2). IL-8 was produced constitutively by 2.2.15 cells, and increased with the number of CD8+ T cell clones in direct as well as indirect contact (Supplemental Fig. 2). IL-2 was undetectable, and the levels of IL10, -5, and -6 were ,20 pg/ml (Supplemental Fig. 2). FIGURE 2. Cytokines production. A, IFN-g and TNF-a produced by the HBc18–27-specific CD8+ T cell line cocultured with 2.2.15 cells in the direct and indirect systems for 3, 24, or 48 h. CD8+ T cell line (E) and 2.2.15 cells (T) were cultured at E:T ratios of 1:300, 1:60, and 1:6. The data are expressed as mean 6 SD from three independent experiments. The statistical significance was calculated versus the nonstimulated CD8+ T cells. pp # 0.05; ppp # 0.005; pppp # 0.001. B, IFN-g and TNF-a produced by CD8+ T cell clone cocultured with 2.2.15 cells in the direct and indirect systems for 24 or 48 h with E:T ratios of 0, 1:60, and 1:6. The data are expressed as mean 6 SD from two independent experiments. Downloaded from http://www.jimmunol.org/ by guest on August 12, 2017 as well as in the indirect system (Fig. 2A). The CD8+ T cell clone produced high levels of IFN-g and TNF-a in the direct and indirect systems; overall, the cytokine levels increased with the E:T ratio (Fig. 2B). High levels of secreted FasL were detected in the direct system following contact with 2.2.15 cells, whereas lower levels 290 Cytotoxicity of target 2.2.15 cells HBV replication levels during cocultures experiments The effect on HBV replication was assessed by the quantification of nucleocapsid-associated HBV DNA (cytoplasmic HBV DNA) and HBV DNA levels in the culture supernatants (secreted HBV DNA). The changes in HBV DNA were expressed as the percentage of increase (positive values) or decrease (negative values) in cytoplasmic and secreted HBV DNA. Initially, the production of cytoplasmic HBV DNA by confluent 2.2.15 cells was monitored in the absence of T cells and showed a 3fold increase over 48 h (Supplemental Fig. 3). Then the effect of the FIGURE 3. Cytotoxic effect of CD8+ T cells on 2.2.15 cells in the direct and indirect coculture systems. A, Percentage of cell death was measured by LDH release. The data are expressed as mean 6 SD from three independent experiments. The statistical significance was calculated versus the percentage of cytotoxicity at 3 h. pp # 0.05; ppp # 0.005; pppp # 0.001. Percentage of apoptotic and necrotic 2.2.15 cells after 24 h of culture with CD8+ T cell line (B) and CD8+ T cell clone (C). The percentages in the lower right corner (AnnexinV positive) and the top of the plot (Propidium Iodide and AnnexinV positive) represent the proportion of early apoptosis and the late stage of apoptosis/necrosis, respectively. Dot plots are representative of three separate experiments. coculture between the CD8+ T cell line and 2.2.15 cells on HBV replication was studied. In the direct system, the level of HBV DNA was reduced with all three E:T ratios; the most significant decrease was with an E:T ratio of 1:6, with a reduction of 87% (p # 0.001) after 48 h compared with 2.2.15 cells cultured alone (Fig. 4A, Supplemental Fig. 4A). In the indirect system, in which only the effect of cytokines on HBV DNA was studied, there was a profound reduction in the viral DNA levels with all E:T ratios; again, the greatest decrease (54.67% [p # 0.001]), occurred after 48 h with an E:T ratio of 1:6 compared with 2.2.15 cells cultured with a nonstimulated CD8+ T cell line (Fig. 4A, Supplemental Fig. 4A). The kinetics of viral particle secretion in the 2.2.15 supernatants was also monitored in the absence of T cells, and it showed a log increase over 48 h (Supplemental Fig. 3). As observed with cytoplasmic HBV DNA, the interaction of the direct or indirect systems with the different E:T ratios influenced the secretion of HBV DNA. With the indirect system, a significant decrease of 23.7% (p # 0.05), 39.1% (p # 0.005), and 74.1% (p # 0.001) was observed with 1:300, 1:60, and 1:6 ratios, respectively, after 48 h (Fig. 4A, Supplemental Fig. 4B). In the direct system, an E:T ratio of 1:60 induced an 82.3% (p # 0.005) decrease after 48 h. Surprisingly, with an E:T ratio of 1:6, secreted HBV DNA increased and reached 45% (p # 0.005) at 24 h and 96.6% (p # 0.005) at 48 h (Fig. 4A, Supplemental Fig. 4B). This significant increase could be attributable to the release of viral DNA from the necrotic cells into the culture medium. Cytoplasmic and supernatant HBV DNA were also quantitated after direct and indirect contact between the CD8+ T cell clone and 2.2.15 cells (Fig. 4B). The results supported the findings obtained with the CD8+ T cell line. Cytoplasmic HBV DNA decreased significantly in the direct and indirect coculture systems, and the greatest effect was observed with the 1:6 ratio after 48 h (p # Downloaded from http://www.jimmunol.org/ by guest on August 12, 2017 The degree of target 2.2.15 cell cytotoxicity was assessed after direct and indirect contact with the CD8+ T cell line. The type of culture (direct or indirect), the number of T cells, and the duration of cell culture had an impact on the degree of 2.2.15 cell cytotoxicity. A maximum of 30% (p # 0.005) cell death was reached after 24 h with an E:T ratio of 1:6 (Fig. 3A). Despite an increase of cytotoxicity from 3 to 48 h with E:T ratios of 1:300 and 1:60 ratios, 30% of cell death was not reached, whereas in the indirect system, no cytotoxicity was observed at any E:T ratio (Fig. 3A). The assessment of the percentage of apoptotic and necrotic 2.2.15 cells confirmed these observations (Fig. 3B). During direct contact between the CD8+ T cell line and 2.2.15 cells at a ratio of 1:6 after a 24-h incubation, 11.6% of the target cells were in early-stage apoptosis, and 16.3% were in late-stage apoptosis and necrosis (Fig. 3B). In contrast, there was no difference in the level of apoptosis and necrosis between the 2.2.15 cells in indirect contact with CD8+ T cells and 2.2.15 cells cultured alone, suggesting that the cytokines produced by CD8+ T cells did not have a cytotoxic effect on the human target cells (Fig. 3B). Similar results were found with the CD8+ T cell clone (Fig. 3C). CYTOLYTIC VERSUS NONCYTOLYTIC HBV INHIBITION The Journal of Immunology 291 0.001) (Fig. 4B). The level of HBV DNA in the supernatants was also reduced in the indirect coculture system with the two E:T ratios (p # 0.005) (Fig. 4B). However, as observed with the CD8+ T cell line, the direct contact between the CD8+ T cell clone and 2.2.15 cells at an E:T ratio of 1:6 induced killing of the target cells that could be responsible for the release of HBV DNA in the supernatant at 24 h (p # 0.005) and 48 h (p # 0.001) (Fig. 4B). A strong correlation (r = 0.889; p = 0.003) between target cell death and the increase in the HBV DNA level in the coculture supernatant supports the notion that this was the case (Fig. 4C). Blocking experiments with Abs to IFN-g or TNF-a were performed to evaluate the effect of neutralizing the activity of these cytokines, which were produced by the CD8+ T cell clone in the direct and indirect systems with an E:T ratio of 1:6 (Fig. 4B). Blocking of IFN-g, TNF-a, or both cytokines in the direct system inhibited the antiviral effect, because it decreased the reduction of cytoplasmic HBV DNA at 24 and 48 h. The nucleic acid was only reduced by 28% (p # 0.005), 28% (p # 0.001), and 14% (p # 0.005), respectively, at 48 h compared to the 70% reduction observed when the cytokines were not blocked. In the indirect Downloaded from http://www.jimmunol.org/ by guest on August 12, 2017 FIGURE 4. Effect of HBV-specific CD8+ T cells on intracellular core-associated HBV DNA (cytoplasmic) and HBV DNA from secreted viral particles (secreted) in the presence or absence of neutralizing Abs. A, CD8+ T cell line was cocultured with 2.2.15 cells in the direct and indirect systems for 3, 24, or 48 h with E:T ratios of 1:300,1:60, and 1:6. Quantitation by real-time PCR of intracellular core-associated HBV DNA and HBV DNA from the secreted viral particles. HBV DNA was expressed as a percentage of change (decrease [negative values] or increase [positive values]) compared with HBV DNA produced by the 2.2.15 cells cultured alone (cytoplasmic) or with unstimulated CD8+ T cells (secreted) at the same time point. B, CD8+ T cell clone was cocultured with 2.2.15 cells with E:T ratios of 1:60 and 1:6 in the presence or absence of IFN-g– and TNF-a–neutralizing Abs. Intracellular core-associated HBV DNA and HBV DNA from the secreted viral particles were quantitated as described above. The data are expressed as mean 6 SD from three independent experiments. The statistical significance was calculated versus controls, 2.2.15 cells cultured alone, or 2.2.15 cells cultured with unstimulated CD8+ T cells, except for the cytokine-neutralizing experiments, for which the statistics were calculated versus the same condition in the presence of cytokines. pp # 0.05; ppp # 0.005; pppp # 0.001. C, Correlation between cell death and HBV DNA secreted in the supernatant of the direct system with a 1:6 ratio. 292 Effect of rIFN-g and rTNF-a on HBV replication To further confirm that IFN-g and TNF-a are directly involved in CD8+ T cell antiviral activity against HBV, the target 2.2.15 cells were treated with rIFN-g and rTNF-a for 24 or 48 h (Fig. 5). The concentrations of the two cytokines were within the range of the cytokine levels produced by stimulated CD8+ T cell line or clone. Cytoplasmic and secreted HBV DNA were reduced in the presence of the recombinant cytokines. In the presence of rIFN-g, the reduction in HBV DNA was concentration dependent. Compared with nontreated cells, the maximum decrease in secreted and cytoplasmic HBV DNA was 63% (p # 0.001) and 47% (p # 0.001), respectively, after 48 h of treatment with 3000 pg/ml rIFN-g (Fig. 5A). Moreover, this reduction was within the range of the inhibition found with the CD8+ T cell line and clone. In the presence of rTNF-a, secreted and cytoplasmic HBV DNA were also significantly reduced (Fig. 5B). The maximum inhibition of cytoplasmic and secreted HBV DNA was observed at 24 h: 60% (p # 0.005) and 66% (p # 0.005), respectively. Moreover, combining these two cytokines had an additive effect on secreted HBV DNA replication (Fig. 5C). The noncytolytic activity of the cytokines FIGURE 5. Effect of recombinant human cytokines on HBV DNA and cytotoxic function against 2.2.15 cells. Quantitation of intracellular core-associated HBV DNA and HBV DNA from the secreted viral particles after 24 or 48 h of treatment with rIFN-g (A), rTNF-a (B), and the combined cytokines (C). The viral DNA was expressed as a percentage of change compared with HBV DNA produced by 2.2.15 cells cultured alone at the same time point. The data are expressed as mean 6 SD from four independent experiments. The statistical significance was calculated versus HBV DNA levels in 2.2.15 cells in the absence of cytokine treatment. D, Percentage of apoptotic 2.2.15 cells after 48 h of treatment with recombinant cytokines. The percentages in the lower right corner (AnnexinV positive) and the top of the plots (Propidium Iodide and AnnexinV positive) represent the proportion of early apoptosis and the late stage of apoptosis/necrosis, respectively. Dot plots are representative of two separate experiments. Downloaded from http://www.jimmunol.org/ by guest on August 12, 2017 system, at 48 h, blocking of IFN-g, TNF-a, or both cytokines induced only a 10% (p # 0.05), 14% (p # 0.05), and 4% (p # 0.005) reduction in cytoplasmic HBV DNA, respectively, compared with the 55% reduction observed when the cytokines were not blocked (Fig. 4B). These experiments confirm that these two cytokines are key mediators for the inhibition of HBV, because their blocking induced less HBV DNA reduction. Similarly, the reduction of secreted HBV DNA was inhibited in the indirect system after blocking the activity of these cytokines (Fig. 4B). In the indirect system, secreted HBV DNA, which was subject to a 77% reduction at 48 h in the presence of IFN-g and TNF-a, was only reduced by 27% (p # 0.05), 33% (p # 0.05), and 23% (p # 0.005), respectively, when IFN-g, TNF-a, or both cytokines were neutralized (Fig. 4B). The killing of 2.2.15 cells by the CD8+ T cell clone in the direct system was not affected by the blocking of the cytokines, because high levels of HBV DNA were detected in the coculture supernatants (Fig. 4B). The data allowed us to estimate that a smaller fraction of the HBV DNA reduction—14% of the inhibition—was due to cell killing, whereas .50% of the antiviral effect was mediated by IFN-g or TNF-a. CYTOLYTIC VERSUS NONCYTOLYTIC HBV INHIBITION The Journal of Immunology was confirmed because there was no difference in the level of apoptosis and necrosis between cytokine-treated and nontreated 2.2.15 cells (Fig. 5D). Effect of activated, HLA-mismatched lymphocytes FIGURE 6. Effect of activation of HLA-mismatched lymphocytes on HBV DNA. A, IFN-g production by PHA-stimulated PBMCs from three chronic patients cultured in direct or indirect contact with 2.2.15 cells. The statistical significance was calculated versus nonstimulated PBMCs. B, Percentage of 2.2.15 cell death measured by LDH release after treatment with PBMCs stimulated by PHA in direct or indirect contact. The statistical significance was calculated versus the percentage of cytotoxicity with 200,00 PBMCs. Quantitation of intracellular core-associated HBV DNA (C) and HBV DNA from the secreted viral particles (D) after coculture of 2.2.15 cells with PHA- stimulated PBMCs in direct and indirect contact. HBV DNA was expressed as a percentage of change compared to HBV DNA produced by the 2.2.15 cells cultured alone at the same time point. The statistical significance was calculated versus HBV DNA levels in 2.2.15 cells cultured alone. The data are expressed as mean 6 SD from three independent experiments. pp # 0.05; ppp # 0.005; pppp # 0.001. Discussion The traditional concept has been that HBV clearance is a result of the destruction of HBV-infected hepatocytes. This is supported by clinical observations that patients developing alanine aminotransferase flares during acute HBV infection or during IFN-a treatment of chronic hepatitis B have a greater chance of resolving HBV infection, suggesting that cytolytic mechanisms are important for HBV clearance (19–22). However, studies using experimental models showed that the antiviral immunity to HBV involves cytokines that can directly inactivate viral replication without destroying the infected cells (10–13). This cytokine-mediated noncytolytic control of HBV was also shown to be effective in other viral infections (23–25). The efficacy of IFN-g to induce noncytolytic inhibition of HBV replication without an increase in the alanine aminotransferase levels is also supported by studies using rIL-12 in the HBV transgenic mouse and in patients with chronic hepatitis B (26, 27). However, the relative involvement of the cytolytic and noncytolytic effector functions of CD8+ T cells has not been investigated. The in vitro coculture model used in this study allowed us to investigate independently the cytolytic and noncytolytic functions of virus-specific CD8+ T cells that otherwise happen simultaneously and, furthermore, to dissect the roles of these two functions with human target cells supporting full HBV replication. Also, the use of an increased number of Ag-specific CD8+ T cells in direct contact with the HBV-producing hepatocytes allowed insight into the balance between these two effector functions. The CD8+ T cell line and the T cell clone used in this study were specific for HBc18–27, an HLA-A2–restricted human immunodominant Downloaded from http://www.jimmunol.org/ by guest on August 12, 2017 The effect of mitogen-activated mononuclear cells on HBV replication was also studied (Fig. 6). For this purpose, 2 3 105 and 1.2 3 106 PBMCs from patients negative for HLA-A2 and with chronic hepatitis B were stimulated with PHA and cocultured in direct or indirect contact with 2.2.15 cells. In the direct coculture system, IFN-g levels increased with the number of PBMCs (p # 0.001). In the indirect system, the cytokine was not detectable with 2 3 105 PBMCs, but increased significantly with 1.2 3 106 PBMCs (p # 0.001) (Fig. 6A). There was a significant difference in the target cell cytotoxicity levels between the two culture systems. Although the indirect system showed minimal cytotoxicity, in the direct system, on average, 30.5% and 90.5% of 2.2.15 cells were killed in the presence of 2 3 105 and 1.2 3 106 PBMCs, respectively (Fig. 6B). Intracellular nucleocapsid-associated HBV DNAwas reduced in the presence of PHA-stimulated PBMCs in the direct and indirect systems, with a maximum of 40.5% (p # 0.001) and 50.9% (p # 0.05) reduction in the presence of 1.2 3 106 PBMCs (Fig. 6C). The HBV DNA levels in the supernatants were reduced by an average of 20% (p # 0.05) for the two PBMC concentrations in the indirect system. In the direct system, secreted HBV DNA was reduced only with 2 3 105 PBMCs; HBV DNA significantly increased with 1.2 3 106 PBMCs (p # 0.005) (Fig. 6D). 293 294 maintenance of this balance is the “programmed death” (PD-1) pathway, which was recently identified as an immuno-inhibitory pathway belonging to the B7 family of immune regulators. The PD-1 pathway is involved in the development of T cell tolerance and has been implicated in the persistence of a variety of chronic viral infections, including lymphocytic choriomeningitis virus, HIV, HBV, and hepatitis C virus (37–44). There is already some evidence that blockade of the PD-1/programmed death ligand-1 synapse could alter the balance between cytolytic and noncytolytic CD8+ effector T cell functions, resulting in exacerbation of immune-mediated tissue damage in herpetic keratitis or in autoimmune enteritis (45, 46). It is possible that the PD-1 pathway acts as a mechanism by which CD8+ T cells engage in cross-talk with the target cells to program their effector functions; the hypothesis that the PD-1 pathway may have a role in modulating the effector functions of virus-specific CD8+ T cells deserves to be investigated in future studies. Characterizing the mechanisms by which HBV-specific CD8+ T cell effector function commitment is modulated would be important in understanding the immunopathogenesis of HBV infection and the development of novel therapeutic strategies. Acknowledgments We thank Prof. Antonio Bertoletti (Singapore Institute for Clinical Sciences, Agency for Science Technology and Research) for providing the HBVspecific CD8+ T cell clone. Disclosures The authors have no financial conflicts of interest. References 1. Chisari, F. V., and C. Ferrari. 1995. Hepatitis B virus immunopathogenesis. Annu. Rev. Immunol. 13: 29–60. 2. Ganem, D., and A. M. Prince. 2004. Hepatitis B virus infection—natural history and clinical consequences. N. Engl. J. Med. 350: 1118–1129. 3. Rehermann, B., and M. Nascimbeni. 2005. Immunology of hepatitis B virus and hepatitis C virus infection. Nat. Rev. Immunol. 5: 215–229. 4. Ferrari, C., A. Penna, A. Bertoletti, A. Valli, A. D. Antoni, T. Giuberti, A. Cavalli, M. A. Petit, and F. Fiaccadori. 1990. Cellular immune response to hepatitis B virus-encoded antigens in acute and chronic hepatitis B virus infection. J. Immunol. 145: 3442–3449. 5. Penna, A., F. V. Chisari, A. Bertoletti, G. Missale, P. Fowler, T. Giuberti, F. Fiaccadori, and C. Ferrari. 1991. Cytotoxic T lymphocytes recognize an HLAA2-restricted epitope within the hepatitis B virus nucleocapsid antigen. J. Exp. Med. 174: 1565–1570. 6. Penna, A., G. Del Prete, A. Cavalli, A. Bertoletti, M. M. D’Elios, R. Sorrentino, M. D’Amato, C. Boni, M. Pilli, F. Fiaccadori, et al. 1997. Predominant T-helper 1 cytokine profile of hepatitis B virus nucleocapsid-specific T cells in acute selflimited hepatitis B. Hepatology 25: 1022–1027. 7. Rehermann, B., P. Fowler, J. Sidney, J. Person, A. Redeker, M. Brown, B. Moss, A. Sette, and F. V. Chisari. 1995. The cytotoxic T lymphocyte response to multiple hepatitis B virus polymerase epitopes during and after acute viral hepatitis. J. Exp. Med. 181: 1047–1058. 8. Ando, K., L. G. Guidotti, S. Wirth, T. Ishikawa, G. Missale, T. Moriyama, R. D. Schreiber, H. J. Schlicht, S. N. Huang, and F. V. Chisari. 1994. Class Irestricted cytotoxic T lymphocytes are directly cytopathic for their target cells in vivo. J. Immunol. 152: 3245–3253. 9. Maini, M. K., C. Boni, C. K. Lee, J. R. Larrubia, S. Reignat, G. S. Ogg, A. S. King, J. Herberg, R. Gilson, A. Alisa, et al. 2000. The role of virus-specific CD8(+) cells in liver damage and viral control during persistent hepatitis B virus infection. J. Exp. Med. 191: 1269–1280. 10. Guidotti, L. G., K. Ando, M. V. Hobbs, T. Ishikawa, L. Runkel, R. D. Schreiber, and F. V. Chisari. 1994. Cytotoxic T lymphocytes inhibit hepatitis B virus gene expression by a noncytolytic mechanism in transgenic mice. Proc. Natl. Acad. Sci. USA 91: 3764–3768. 11. Guidotti, L. G., T. Ishikawa, M. V. Hobbs, B. Matzke, R. Schreiber, and F. V. Chisari. 1996. Intracellular inactivation of the hepatitis B virus by cytotoxic T lymphocytes. Immunity 4: 25–36. 12. Guidotti, L. G., R. Rochford, J. Chung, M. Shapiro, R. Purcell, and F. V. Chisari. 1999. Viral clearance without destruction of infected cells during acute HBV infection. Science 284: 825–829. 13. Thimme, R., S. Wieland, C. Steiger, J. Ghrayeb, K. A. Reimann, R. H. Purcell, and F. V. Chisari. 2003. CD8(+) T cells mediate viral clearance and disease pathogenesis during acute hepatitis B virus infection. J. Virol. 77: 68–76. Downloaded from http://www.jimmunol.org/ by guest on August 12, 2017 epitope. The immune response to the HBV nucleocapsid Ag is known to be the key for control of HBV replication (15, 28), and the HBc18–27 epitope is being considered as an immunotherapeutic target (29–31). In this study, using human effector and target cells, we demonstrated that although CD8+ T cells can kill infected cells, they also inactivate HBV by efficiently purging the virus from the infected cells, without inflicting cellular damage, which is primarily mediated by IFN-g and TNF-a production. When the CD8+ T cell line and clone were in direct contact with the target cells at an E:T ratio of 1:6, we observed .30% cell death and a 60–80% reduction in cytoplasmic HBV DNA. At the two lower E:T ratios, cell death was reduced to 10–15%, and cytoplasmic HBV DNA decreased from 30–60%, suggesting that cell killing and cytokine-mediated mechanisms were at play to inhibit HBV replication. In the indirect system, in which only the antiviral effect of cytokines secreted by the CD8+ T cell line and clone is operating, the cytoplasmic HBV DNA was reduced up to 50% with an E:T ratio of 1:6 and between 20–30% with the lower ratios, with no cytotoxicity. This suggests that the noncytolytic mechanisms are more efficient in inhibiting HBV replication compared with direct lytic mechanisms, which extends the observations in the HBV transgenic mouse model (10, 32). IFN-g and TNF-a were the two cytokines that were found to mediate CD8+ T cell antiviral activity in the HBV-transgenic mouse model and in experimental HBV infection of chimpanzees (24, 25, 33, 34). We previously showed that IFN-g produced upon stimulation of CD4+ T cells with recombinant HBcAg could inhibit HBV transcription and replication without target cell lysis (35). In the current study, high levels of these cytokines were produced by the CD8+ T cell line or the T cell clone after Agspecific stimulation in the two coculture systems. The involvement of the two cytokines in this antiviral control of HBV replication was clearly demonstrated through the abrogation of this control by inhibition of the cytokines with neutralizing Abs. Blocking each cytokine individually or together induced less reduction in the cytoplasmic and secreted HBV DNA in both culture systems and showed that .50% of the 70% of total inhibition observed in the direct system was mediated by IFN-g and TNF-a. Interestingly, IFN-g and TNF-a antiviral effects were synergistic. The 4% inhibition remaining after neutralization of both cytokines in the indirect system could be the result of suboptimal levels of IFN-g and TNF-a or other unidentified cytokines. This idea could be further supported by the fact that with an E:T ratio of 1:300, HBV DNA was reduced when IFN-g and TNF-a levels were below the limit of detection of the assay. The cytokine antiviral activity against HBV was further confirmed by treating 2.2.15 cells directly with the rIFN-g and rTNF-a. Although CD8+ T cells can induce cell death by apoptosis, several studies suggested that virus nonspecific inflammatory cells could be responsible for most of the damage in the liver (9, 36). We investigated this in the current study using HLA-mismatched PBMCs stimulated with mitogen (PHA), which resulted in the killing of a high percentage of the target 2.2.15 cells. Moreover, the level of cytotoxicity induced by the HLA-mismatched activated lymphomononuclear cells was much higher than with the CD8+ T cells, providing, for the first time, direct evidence that most of the liver cell damage is caused by HBV-nonspecific inflammatory cells. A higher level of cytotoxicity was expected in the experiments in which CD8+ T cells were freely moving and in direct contact with the target cells, all of which were producing HBV and, therefore, were potential targets for the cytotoxic CD8+ T cells. Instead, we observed that only a relatively small fraction of these target cells were lysed, leading us to hypothesize that a regulatory mechanism was at play that could control the balance between cytolytic and noncytolytic CD8+ T cell functions. Of possible importance in the CYTOLYTIC VERSUS NONCYTOLYTIC HBV INHIBITION The Journal of Immunology 30. Xu, W., Y. Chu, R. Zhang, H. Xu, Y. Wang, and S. Xiong. 2005. Endoplasmic reticulum targeting sequence enhances HBV-specific cytotoxic T lymphocytes induced by a CTL epitope-based DNA vaccine. Virology 334: 255–263. 31. Shi, T. D., Y. Z. Wu, Z. C. Jia, L. Y. Zou, and W. Zhou. 2004. Therapeutic polypeptides based on HBV core 18-27 epitope can induce CD8+ CTL-mediated cytotoxicity in HLA-A2+ human PBMCs. World J. Gastroenterol. 10: 1902– 1906. 32. Chisari, F. V. 1995. Hepatitis B virus transgenic mice: insights into the virus and the disease. Hepatology 22: 1316–1325. 33. Guidotti, L. G., and F. V. Chisari. 1999. Cytokine-induced viral purging—role in viral pathogenesis. Curr. Opin. Microbiol. 2: 388–391. 34. Guidotti, L. G., and F. V. Chisari. 2001. Noncytolytic control of viral infections by the innate and adaptive immune response. Annu. Rev. Immunol. 19: 65–91. 35. Suri, D., R. Schilling, A. R. Lopes, I. Mullerova, G. Colucci, R. Williams, and N. V. Naoumov. 2001. Non-cytolytic inhibition of hepatitis B virus replication in human hepatocytes. J. Hepatol. 35: 790–797. 36. Ando, K., T. Moriyama, L. G. Guidotti, S. Wirth, R. D. Schreiber, H. J. Schlicht, S. N. Huang, and F. V. Chisari. 1993. Mechanisms of class I restricted immunopathology. A transgenic mouse model of fulminant hepatitis. J. Exp. Med. 178: 1541–1554. 37. Barber, D. L., E. J. Wherry, D. Masopust, B. Zhu, J. P. Allison, A. H. Sharpe, G. J. Freeman, and R. Ahmed. 2006. Restoring function in exhausted CD8 T cells during chronic viral infection. Nature 439: 682–687. 38. Boni, C., P. Fisicaro, C. Valdatta, B. Amadei, P. Di Vincenzo, T. Giuberti, D. Laccabue, A. Zerbini, A. Cavalli, G. Missale, et al. 2007. Characterization of hepatitis B virus (HBV)-specific T-cell dysfunction in chronic HBV infection. J. Virol. 81: 4215–4225. 39. Day, C. L., D. E. Kaufmann, P. Kiepiela, J. A. Brown, E. S. Moodley, S. Reddy, E. W. Mackey, J. D. Miller, A. J. Leslie, C. DePierres, et al. 2006. PD-1 expression on HIV-specific T cells is associated with T-cell exhaustion and disease progression. Nature 443: 350–354. 40. Evans, A., A. Riva, H. Cooksley, S. Phillips, S. Puranik, A. Nathwani, S. Brett, S. Chokshi, and N. V. Naoumov. 2008. Programmed death 1 expression during antiviral treatment of chronic hepatitis B: Impact of hepatitis B e-antigen seroconversion. Hepatology 48: 759–769. 41. Golden-Mason, L., B. Palmer, J. Klarquist, J. A. Mengshol, N. Castelblanco, and H. R. Rosen. 2007. Upregulation of PD-1 expression on circulating and intrahepatic hepatitis C virus-specific CD8+ T cells associated with reversible immune dysfunction. J. Virol. 81: 9249–9258. 42. Penna, A., M. Pilli, A. Zerbini, A. Orlandini, S. Mezzadri, L. Sacchelli, G. Missale, and C. Ferrari. 2007. Dysfunction and functional restoration of HCVspecific CD8 responses in chronic hepatitis C virus infection. Hepatology 45: 588–601. 43. Trautmann, L., L. Janbazian, N. Chomont, E. A. Said, S. Gimmig, B. Bessette, M. R. Boulassel, E. Delwart, H. Sepulveda, R. S. Balderas, et al. 2006. Upregulation of PD-1 expression on HIV-specific CD8+ T cells leads to reversible immune dysfunction. Nat. Med. 12: 1198–1202. 44. Urbani, S., B. Amadei, D. Tola, M. Massari, S. Schivazappa, G. Missale, and C. Ferrari. 2006. PD-1 expression in acute hepatitis C virus (HCV) infection is associated with HCV-specific CD8 exhaustion. J. Virol. 80: 11398–11403. 45. Jun, H., S. K. Seo, H. Y. Jeong, H. M. Seo, G. Zhu, L. Chen, and I. H. Choi. 2005. B7-H1 (CD274) inhibits the development of herpetic stromal keratitis (HSK). FEBS Lett. 579: 6259–6264. 46. Reynoso, E. D., K. G. Elpek, L. Francisco, R. Bronson, A. Bellemare-Pelletier, A. H. Sharpe, G. J. Freeman, and S. J. Turley. 2009. Intestinal tolerance is converted to autoimmune enteritis upon PD-1 ligand blockade. J. Immunol. 182: 2102–2112. Downloaded from http://www.jimmunol.org/ by guest on August 12, 2017 14. Sells, M. A., A. Z. Zelent, M. Shvartsman, and G. Acs. 1988. Replicative intermediates of hepatitis B virus in HepG2 cells that produce infectious virions. J. Virol. 62: 2836–2844. 15. Webster, G. J., S. Reignat, D. Brown, G. S. Ogg, L. Jones, S. L. Seneviratne, R. Williams, G. Dusheiko, and A. Bertoletti. 2004. Longitudinal analysis of CD8+ T cells specific for structural and nonstructural hepatitis B virus proteins in patients with chronic hepatitis B: implications for immunotherapy. J. Virol. 78: 5707–5719. 16. Gehring, A. J., D. Sun, P. T. Kennedy, E. Nolte-’t Hoen, S. G. Lim, S. Wasser, C. Selden, M. K. Maini, D. M. Davis, M. Nassal, et al. 2007. The level of viral antigen presented by hepatocytes influences CD8 T-cell function. J. Virol. 81: 2940–2949. 17. Proto, S., J. A. Taylor, S. Chokshi, N. Navaratnam, and N. V. Naoumov. 2008. APOBEC and iNOS are not the main intracellular effectors of IFN-g-mediated inactivation of Hepatitis B virus replication. Antiviral Res. 78: 260–267. 18. Pas, S. D., E. Fries, R. A. De Man, A. D. Osterhaus, and H. G. Niesters. 2000. Development of a quantitative real-time detection assay for hepatitis B virus DNA and comparison with two commercial assays. J. Clin. Microbiol. 38: 2897– 2901. 19. Nair, S., and R. P. Perrillo. 2001. Serum alanine aminotransferase flares during interferon treatment of chronic hepatitis B: is sustained clearance of HBV DNA dependent on levels of pretreatment viremia? Hepatology 34: 1021–1026. 20. Webster, G. J., S. Reignat, M. K. Maini, S. A. Whalley, G. S. Ogg, A. King, D. Brown, P. L. Amlot, R. Williams, D. Vergani, et al. 2000. Incubation phase of acute hepatitis B in man: dynamic of cellular immune mechanisms. Hepatology 32: 1117–1124. 21. Hoofnagle, J. H., M. Peters, K. D. Mullen, D. B. Jones, V. Rustgi, A. Di Bisceglie, C. Hallahan, Y. Park, C. Meschievitz, and E. A. Jones. 1988. Randomized, controlled trial of recombinant human a-interferon in patients with chronic hepatitis B. Gastroenterology 95: 1318–1325. 22. Marinos, G., F. Torre, S. Chokshi, M. Hussain, B. E. Clarke, D. J. Rowlands, A. L. Eddleston, N. V. Naoumov, and R. Williams. 1995. Induction of T-helper cell response to hepatitis B core antigen in chronic hepatitis B: a major factor in activation of the host immune response to the hepatitis B virus. Hepatology 22: 1040–1049. 23. Cavanaugh, V. J., L. G. Guidotti, and F. V. Chisari. 1998. Inhibition of hepatitis B virus replication during adenovirus and cytomegalovirus infections in transgenic mice. J. Virol. 72: 2630–2637. 24. Guidotti, L. G., P. Borrow, A. Brown, H. McClary, R. Koch, and F. V. Chisari. 1999. Noncytopathic clearance of lymphocytic choriomeningitis virus from the hepatocyte. J. Exp. Med. 189: 1555–1564. 25. Guidotti, L. G., and F. V. Chisari. 2000. Cytokine-mediated control of viral infections. Virology 273: 221–227. 26. Cavanaugh, V. J., L. G. Guidotti, and F. V. Chisari. 1997. Interleukin-12 inhibits hepatitis B virus replication in transgenic mice. J. Virol. 71: 3236–3243. 27. Rigopoulou, E. I., D. Suri, S. Chokshi, I. Mullerova, S. Rice, R. S. Tedder, R. Williams, and N. V. Naoumov. 2005. Lamivudine plus interleukin-12 combination therapy in chronic hepatitis B: antiviral and immunological activity. Hepatology 42: 1028–1036. 28. Lau, G. K., D. Suri, R. Liang, E. I. Rigopoulou, M. G. Thomas, I. Mullerova, A. Nanji, S. T. Yuen, R. Williams, and N. V. Naoumov. 2002. Resolution of chronic hepatitis B and anti-HBs seroconversion in humans by adoptive transfer of immunity to hepatitis B core antigen. Gastroenterology 122: 614–624. 29. Zhang, Y., S. Li, M. Shan, X. Pan, K. Zhuang, L. He, K. Gould, and P. Tien. 2007. Hepatitis B virus core antigen epitopes presented by HLA-A2 single-chain trimers induce functional epitope-specific CD8+ T-cell responses in HLA-A2.1/ Kb transgenic mice. Immunology 121: 105–112. 295