* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
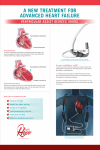
Download Left Ventricular Assist Device (LVAD)
Management of acute coronary syndrome wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Coronary artery disease wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Heart failure wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Jatene procedure wikipedia , lookup
Electrocardiography wikipedia , lookup
Myocardial infarction wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Heart arrhythmia wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
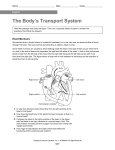
Left Ventricular Assist Device (LVAD) LVAD uses an external pump outside the body to bypass the left ventricle. The blood is drained from the apex of the left ventricle via an intake cannula and ejected into the aorta via an output cannula. BiVAD bypasses both ventricles. The development of LVAD began in the 1960s as a bridge to cardiac transplant. It has evolved into a “destination therapy,” meaning a permanent therapy rather than a transitional stage until another therapy. The indication for LVAD candidates is New York Heart Association class 4 heart failure, ejection fraction <25%, VO2 max (the maximum rate of oxygen consumption) less than 15, among other criteria. All VADs are preload dependent, but ECG independent, unlike ICDs. VADs have 3 major variables: speed, flow, and power. Four Key Variables for the Cardiac Function Preload is affected by the end diastolic pressure that stretches the right or left ventricle of the heart to its greatest geometric dimensions under variable physiologic demand. In other words, it is the initial stretching of the sarcomeres in cardiomyocytes prior to contraction. Preload is affected by venous blood pressure and the rate of venous return. Regulation of the preload is related to the atrial natriuretic peptide (ANP) and the kidney function. Afterload is the resistance that the ventricle of the heart has to overcome to eject the blood from the ventricle chamber during systole. The resistance comes from the blood in the vessels and the constriction of the vessel walls. Contractility represents the intrinsic ability of the heart/myocardium to contract. Changes in the ability to produce force during contraction result from incremental degrees of binding between myosin (thick) and actin (thin) filaments. Heart rate is the speed of the heartbeat measured by the number of beats of the heart per minute (bpm). The normal resting adult human heart rate ranges from 60–80 bpm. Bradycardia is a slow heart rate, defined as below 60 bpm. Tachycardia is a fast heart rate, defined as above 100 bpm at rest. The heart rate can vary according to the body's physical needs, including the need to absorb oxygen and excrete carbon dioxide. Activities that can provoke change include physical exercise, sleep, anxiety, stress, illness, ingesting, and drugs. The maximum heart (MHR) achieved by exercise can be age-dependent; a rough estimate is MHR = 220 – age.