* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Urinary system Nephron From the renal artery, an afferent arteriole
Duffy antigen system wikipedia , lookup
Lymphopoiesis wikipedia , lookup
Atherosclerosis wikipedia , lookup
Molecular mimicry wikipedia , lookup
Psychoneuroimmunology wikipedia , lookup
Immune system wikipedia , lookup
Complement system wikipedia , lookup
Monoclonal antibody wikipedia , lookup
Adoptive cell transfer wikipedia , lookup
Adaptive immune system wikipedia , lookup
Cancer immunotherapy wikipedia , lookup
Innate immune system wikipedia , lookup
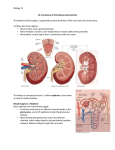
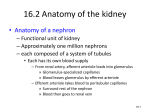
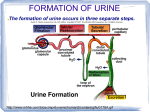
Urinary system Nephron From the renal artery, an afferent arteriole transports blood to the glomerulus, a knot of capillaries inside the glomerular capsule. Blood leaving the glomerulus is carried away by the efferent arteriole. Blood pressure is higher in the glomerulus because the efferent arteriole is narrower than the afferent arteriole. The efferent arteriole divides and forms The peritubular capillary network, which surrounds the rest of the nephron. Blood from the efferent arteriole travels through the peritubular capillary network. Thenthe blood goes into a venule that carries blood into the renal vein Each nephron is made up of several parts Some functions are shared by all parts of the nephron. However, the specifi c structure of each part is especially suited to a particular function First, the closed end of the nephron is pushed in on itself to form a cuplike structure called the glomerular capsule (Bowman’s capsule). The outer layer of the glomerular capsule is composed of squamous epithelialcells. The inner layer is made up of podocytes that have long cytoplasmic extensions. The podocytes cling to the capillary walls of the glomerulus and leave pores that allow easy passage of small molecules from the glomerulus to the inside of the glomerular capsule. This process ,called glomerular filtration, produces a filtrate of the blood. Next, there is a proximal convoluted tubule. The cuboidal epithelial cells lining this part of the nephron have numerous microvilli, about 1 μm in length, that are tightly packed and form a brush border A brush border greatly increases the surface area for the tubular reabsorption of filtrate components. Each cell also has many mitochondria, which can supply energy for active transport of molecules from the lumen to the peritubular capillary network. the tube narrows and makes a U-turn called the loop of the nephron (loop of Henle). Each loop consists of a descending limb and an ascending limb. The descending limb of the loop allows water to diffuse into tissue surrounding the nephron The ascending limb actively transports salt from its lumen to interstitial tissue. As we shall see, this activity facilitates the reabsorption of water by the nephron and collecting duct The cuboidal epithelial cells of the distal convoluted tubule have numerous mitochondria, but they lack microvilli This means that the distal convoluted tubule is not specialized for reabsorption. Instead, its primary function is ion exchange. During ion exchange, cells reabsorb certain ions, returning them to the blood. Other ions are secreted from the blood into the tubule. The distal convoluted tubules of several nephrons enter one collecting duct. Many collecting ducts carry urine to the renal pelvis Urine Formation 1-Glomerular filtration. Due to glomerular blood pressure, water and small molecules move from the glomerulus to the inside of the glomerular capsule. large molecules and formed elements are unable to pass through glomerulus . The glomerular fi ltrate inside the glomerular capsule now contains the fi lterable blood components. nephrons in the kidneys filter 180 liters of water per day, along with a considerable amount of small molecules (such as glucose) and ions (such as sodium). 2-Tubular reabsorption occurs as molecules and ions are passively and actively reabsorbed from the nephron into the blood of the peritubular capillary network. The osmolarity of the blood is maintained by the presence of plasma proteins and salt. When sodium ions (Na+) are actively reabsorbed, chloride ions (Cl–) follow passively. The reabsorption of salt (NaCl) increases the osmolarity of the blood compared with the fi ltrate. Therefore, water moves passively from the tubule into the blood. About 65% of Na+ is reabsorbed at the proximal convoluted tubule. Nutrients such as glucose and amino acids return to the peritubular capillaries almost exclusively at the proximal convoluted tubule This is a selective process because only molecules recognized by carrier proteins are actively reabsorbed. Glucose is an example of a molecule that ordinarily is completely reabsorbed because there is a plentiful supply of carrier proteins for it. However, every substance has a maximum rate of transport. After all its carriers are in use, any excess in the fi ltrate will appear in the urine. In diabetes mellitus, the blood glucose level is above normal and glucose appears in the urine. The presence of excess glucose in the fi ltrate raises its osmolarity. Therefore, less water is reabsorbed into the peritubular capillary network. The frequent urination and increased thirst experienced by people with untreated diabetes are due to less water being reabsorbed from the fi ltrate into the blood. 3-Tubular secretion is a second way by which substances are removed from blood and added to the tubular fluid. Hydrogen ions (H+), creatinine, and drugs such as penicillin are some of the substances moved by active transport from blood into the kidney tubule. In the end, urine contains substances that have undergone glomerular filtration but have not been reabsorbed and substances that have undergone tubular secretion. Immunity . Immunity is the ability of the body to defend itself against infectious agents, foreign cells, and even abnormal body cells, such as cancer cells. Thereby, the internal environment has a better chance of remaining stable. Immunity includes nonspecific and specific defenses. The four types of nonspecific defenses—barriers to entry, the inflammatory reaction, natural killer cells, and protective proteins— are effective against many types of infectious agents -1Barriers to Entry 1-Skin and Mucous Membranes The intact skin is generally an effective physical barrier thatprevents infection. Mucous membranes lining the respiratory, digestive, reproductive, and urinary tracts are also physical barriers to entry by pathogens. For example, the ciliated cells that line the upper respiratory tract sweep mucus and trapped particles up into the throat, where they can be swallowed, spit, or coughed out. 2-Chemical Barriers The chemical barriers to infection include the secretions of sebaceous (oil) glands of the skin. These secretions contain chemicals that weaken or kill certain bacteria on the skin. Perspiration, saliva, and tears contain an antibacterial enzyme called lysozyme. Saliva also helps to wash microbes of the teeth and tongue, and tears wash the eyes. Similarly, as urine is voided from the body, it fl ushes bacteria from the urinary tract.The acid pH of the stomach inhibits growth or kills many types of bacteria. At one time, it was thought that no bacterium could survive the acidity of the stomach. But now we know that ulcers are caused by the bacterium Helicobacter pylori 2 Natural Killer Cells Natural killer (NK) cells kill virus-infected cells and tumor cells by cellto-cell contact. They are large, granular lymphocytes. They have no specificity and no memory. Their number is not increased by immunization. 3 Protective Proteins The complement system, often simply called complement, is a number of plasma proteins designated by the letter C Complement is activated when pathogens enter the body, it is involved in and amplifies the inflammatory response because 1- complement proteins attract phagocytes to the scene. 2- Some complement proteins bind to the surface of pathogens already coated with antibodies, which ensures that the pathogens will be phagocytized by a neutrophil or macrophage 3- Certain other complement proteins join to form a membrane attack complex that produces holes in the walls and plasma membranes of bacteria. Fluids and salts then enter the bacterial cell to the point that they burst 4- inflammatory response (as demonsterated in diagram below) Specific Defenses When nonspecific defenses have failed to prevent an infection specific defenses come into play. An antigen is any foreign substance (often a protein or polysaccharide) that stimulates the immune system to react to itLymphocytes are capable of recognizing an antigen because they have antigen receptors—plasma membrane receptor proteins whose shape allows them to combine with a specific antigen. . Immunity is primarily the result of the action of the B lymphocytes and the T lymphocytes. B lymphocytes mature in the bone marrow,1 and T lymphocytes mature in the thymus gland. B lymphocytes, also called B cells, give rise to plasma cells, which produce antibodies, proteins shaped like the antigen receptor and capable of combining with a specific antigen. These antibodies are secreted into the blood, lymph, and other body fluids. In contrast, T lymphocytes, also called T cells, do not produce antibodies. Instead, certain T cells directly attack cells that bear nonself antigens. Other T cells regulate the immune response Immunity occurs naturally through infection or is brought about artifi cially by medical intervention. The two types of acquired immunity are active and passive. In active immunity the individual alone produces antibodies against an antigen. Active immunity sometimes develops naturally after a person is infected with a pathogen. However, active immunity is often induced when a person is well to prevent future infection. Artifi cial exposure to an antigen through immunization can prevent future disease. The United States is committed to immunizing all children against the common types of childhood disease Immunization involves the use of vaccines, substances that contain an antigen to which the immune system responds. Passive Immunity Passive immunity occurs when an individual is given prepared antibodies or immune cells to combat a disease These antibodies are not produced by the individual’s plasma cells, so passive immunity is temporary. For example newborn infants are passively immune to some diseases because IgG antibodies have crossed the placenta from the mother’s blood). These antibodies soon disappear, and within a few months, infants become more susceptible to infections. Breast-feeding prolongs the natural passive immunity an infant receives from the mother because IgG and IgA antibodies are present in the mother’s milk

















![Urinary System_student handout[1].](http://s1.studyres.com/store/data/008293858_1-b77b303d5bfb3ec35a6e80f57f440bef-150x150.png)