* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Macrophages, pathology and parasite persistence in
Survey
Document related concepts
Lymphopoiesis wikipedia , lookup
Neonatal infection wikipedia , lookup
Hospital-acquired infection wikipedia , lookup
DNA vaccination wikipedia , lookup
Infection control wikipedia , lookup
Schistosoma mansoni wikipedia , lookup
Immune system wikipedia , lookup
Polyclonal B cell response wikipedia , lookup
Molecular mimicry wikipedia , lookup
Sarcocystis wikipedia , lookup
Hygiene hypothesis wikipedia , lookup
Hepatitis B wikipedia , lookup
Adaptive immune system wikipedia , lookup
Cancer immunotherapy wikipedia , lookup
Adoptive cell transfer wikipedia , lookup
Immunosuppressive drug wikipedia , lookup
Transcript
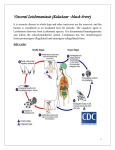
Review TRENDS in Parasitology Vol.20 No.11 November 2004 Immunoparasitology series: Macrophages, pathology and parasite persistence in experimental visceral leishmaniasis Christian R. Engwerda1, Manabu Ato2 and Paul M. Kaye2 1 Immunology and Infection Laboratory, Queensland Institute of Medical Research and Australian Centre for International and Tropical Health and Nutrition, 300 Herston Road, Herston, Queensland, 4029, Australia 2 Department of Infectious and Tropical Diseases, London School of Hygiene and Tropical Medicine, Keppel Street, London, WC1E 7HT, UK Many infectious diseases are associated with parasite persistence, often restricted to certain tissue sites, yet the determinants of such persistence are poorly understood. Infection with the protozoan parasite Leishmania donovani has proved a useful experimental tool to address how immune responses can be differentially effective in clearing parasites from different tissues and, conversely, it might also provide a good model for understanding the basis of parasite persistence. This article reviews recent studies on the determinants and consequences of persistent parasite infection in the spleen and suggest that some of the messages to emerge could have important implications for the study of a broad range of infectious diseases. splenomegaly associated with parasite persistence. This review discusses recent studies on the immunological and pathological alterations that occur in the spleen, concurrent with the establishment of this chronic infection. In addition, future directions for research in this field are suggested, which might help to increase our understanding of the immunological basis for organ-specific immunity during infectious disease. Contrasting outcomes of infection in liver and spleen The diversity in the quality and quantity of host immunity against pathogen infection is apparent when distinct target tissues are examined, and experimental models of Box 1. Visceral leishmaniasis Many of the major bacteria, protozoa and helminth infections of humans are associated with systemic pathogen spread and parasitism of multiple organ systems. This might occur sequentially (as seen in the migrating helminths) or many tissues could be simultaneously involved [as seen in visceral leishmaniasis (VL), tuberculosis and malaria]. Whereas it is apparent from experiments with simple defined antigens that the immune response could be compartmentalised with tissue-specific regulation of the quality and quantity of response, how such factors impact on the outcome of complex infections is poorly understood. In 2000, we reviewed our understanding of the events that mediate organ-specific immune responses during murine infections with the protozoan parasite Leishmania donovani [1], a model of human VL (Box 1). At that time, the focus was largely on understanding the acute but ultimately resolving infection that is observed in the liver of most mouse strains (including BALB/c and C57BL/6). This response is analogous to the protective granulomatous response seen in the majority of humans infected with L. donovani and which remain sub-clinically infected [2]. In contrast to the self-limiting infection observed in the liver, however, these same mouse strains develop life-long Corresponding author: Paul M. Kaye ([email protected]). Available online 3 September 2004 Unlike the many Leishmania spp. that can cause cutaneous leishmaniasis, Leishmania donovani and Leishmania infantum are largely responsible for the systemic disease, visceral leishmaniasis (VL) or kala azar. Approximately 500 000 new cases of VL are reported annually, mostly from India, the Sudan and Brazil, although this is probably a considerable underestimate. In the absence of chemotherapy, most clinical cases of VL result in death. Many infections (possibly O95%) do not, however, progress to clinical VL; parasites are contained, although probably not completely removed, by a self-limiting granulomatous tissue response. Drug resistance against conventional antimonial drugs is now common in India and, despite the availability for a new oral drug, miltefosine, vaccines appear to be the best hope for control of VL. Unfortunately, most efforts in vaccine research have focused on cutaneous disease and those trials that have been performed against VL have been largely unsuccessful. VL is an emergent disease in Europe in association with HIV and also poses a major veterinary problem in areas where domestic dogs serve as reservoir hosts. As with all Leishmania infections, natural transmission occurs during the bloodmeal of a phlebotamine sandfly, which introduces metacyclic infective promastigotes into the dermis. These are resistant to complement attack and they enter local phagocytes rapidly. Transformation into aflagellate amastigotes then occurs and the life history of the infection in humans is perpetuated by this life cycle stage. At what stage of the infection visceralisation occurs is not clear. Infected macrophages might migrate from the initial site of infection to the spleen, liver and bone marrow; alternatively, free promastigotes could enter the bloodstream directly as a result of the pool-feeding behaviour of the sandfly. Why L. donovani and L. infantum are so viscerotropic compared with other species is a key unanswered question. www.sciencedirect.com 1471-4922/$ - see front matter Q 2004 Elsevier Ltd. All rights reserved. doi:10.1016/j.pt.2004.08.009 Review TRENDS in Parasitology VL is perhaps the clearest representation of this diversity (Figure 1). In experimental VL, caused by L. donovani [3] or Leishmania infantum (Leishmania chagasi) [4–6], hepatic infection is usually self-limiting, and the hepatic immune response is a good example of a mononuclear celldominated granulomatous inflammatory response, involving resident Kupffer cells, monocytes and CD4C and CD8C T cells. Many of the cellular and molecular interactions required for efficient hepatic granuloma formation which are necessary to kill Leishmania have been recently reviewed [2]. Of the many cytokines involved [including interferon (IFN)-g, interleukin (IL)-12, IL-4 and tumour necrosis factor (TNF)], moderate levels of TNF clearly make a major contribution to host protection in the liver, with focal TNF production readily observed in hepatic granulomas [7]. By contrast, simultaneously with the resolution of hepatic infection, control of amastigote growth in the spleen is lost and destructive pathology is the norm (Figure 1). Strikingly, excess TNF in this lymphoid environment mediates much of the architectural damage and immunological dysfunction associated with this chronic inflammatory state. While the current literature provides some clues to the basis of this dichotomous host response, many of the in vitro systems and host-cell–parasite combinations that dominate the literature might not be most appropriate for a full appreciation of its complexity. Vol.20 No.11 November 2004 525 different tissues. Although this diversity is largely ignored when studying the pathways for uptake and recognition of Leishmania, it could play a key role in directing many of the ensuing organ-specific events. Identifying the receptors involved in L. donovani recognition by mononuclear phagocytes (including monocytes, tissue macrophages, dendritic cells and their various precursor populations) will be of fundamental importance for understanding several stages in the establishment of infection and initiation of immune responses (Figure 2). One of the most fascinating features of L. donovani and L. infantum infections is their systemic nature; although the underlying biology of visceralisation has yet to be carefully dissected, recent studies are beginning to shed some light on this matter. The development of a low-dose skin dermal model of experimental VL [8] provides a new opportunity to study the visceralisation process in the context of a biologically relevant parasite dose. Another recent study indicated that differential expression of the A2 gene locus between L. donovani and L. major could have a role in visceralisation. Leishmania major does not normally express A2 and transgenic expression of A2 in L. major inhibited the capacity of this parasite to develop local cutaneous lesions and prevented survival in skin macrophages [9]. Future proteomic and genomic comparisons between L. major and L. infantum will soon be possible with the completion of their respective genome sequencing Uptake and recognition of L. donovani amastigotes Mononuclear phagocytes are extremely heterogeneous, which is often evident when isolating these cells from Blood MZ PALS (b) Parasite load (LDU) (a) 1000 (c) 500 (a) (e) (d) 3 14 56 28 128 Days p.i. Parasite load (LDU) (b) 400 Key: 200 DC Macrophage Leishmania 3 14 28 56 128 Days p.i. TRENDS in Parasitology Figure 1. Discrete phases of Leishmania donovani infection in the spleen and liver of inbred mice. The mice were infected with 1!107 to 2!107 amastigotes of L. donovani and a characteristically different outcome is seen in (a) the liver and (b) the spleen. In the liver, amastigote growth is evident from the earliest times post-infection, but is brought under control around Day 28 p.i., with the maturation of the granulomatous tissue response. By contrast, after an early acute phase where amastigote replication is not evident, the spleen shows exaggerated splenomegaly, loss of microarchitecture and persistent presence of amastigotes. Broken green lines indicate approximate range of outcomes encountered in studies of common inbred strains of mice. Broken black lines indicate limit of detection for parasite quantification. Abbreviation: LDU, Leishman Donovan unit; p.i., post-infection. www.sciencedirect.com T cell IL-12p40 TRENDS in Parasitology Figure 2. Early interactions between Leishmania donovani and spleen mononuclear phagocytes. After intravenous injection, amastigotes can be rapidly phagocytosed by blood-borne DC precursors or by monocytes (a). On entry to the MZ, they are phagocytosed by MZM (b) and, to a lesser extent, MMM (not shown). DC could bind amastigotes or antigens released by them (c) and, in rare cases, could themselves be infected (d). Parasite-derived antigens could be passed between macrophages and various DC subsets (arrows) either in the form of released free antigen, by exosomes, or by phagocytosis of apoptotic host cells. Acquired immunity is initiated following traffic of DC into the T-cell zone (PALS) where they encounter T cells and are further stimulated to secrete IL-12 (e). Abbreviations: DC, dendritic cells; IL, interleukin; IL-12p40, interleukin-12/23 p40 subunit; MMM, marginal metallophilic macrophages; MZ, marginal zone; MZM, marginal zone macrophages; PALS, peri-arteriolar lymphoid sheath. 526 Review TRENDS in Parasitology projects (http://www.sanger.ac.uk/Projects/L_infantum/ and http://www.sanger.ac.uk/Projects/L_major/), thus enabling the identification of gene products potentially involved in tissue tropism or differential recognition by mononuclear phagocytes. Using macrophages from both humans and mice, in vitro studies have produced a plethora of candidate receptors involved in parasite uptake (reviewed in Ref. [10]), with more-recent reports emphasizing the complex interplay between recognition of parasite surface structures per se [11] and the role of serum opsonins (including mannose-binding lectin [12] and C-reactive protein [13]). Much attention has also focussed on the C-type lectin DC-specific intracellular adhesion molecule 3-grabbing non-integrin (DC-SIGN; CD209) as a determinant of parasite attachment to dendritic cells (DC) [14,15]. Both L. donovani amastigotes and promastigotes bind DC-SIGN on transfected fibroblasts, and binding to DC can be inhibited by anti-DC-SIGN monoclonal antibodies (mAb). DC-SIGN also binds some (Leishmania pifanoi), but not all (L. major) parasites associated with cutaneous leishmaniasis [16]. Unfortunately, as commented earlier, few of these studies take into account the extreme diversity of tissue mononuclear phagocytes in both receptor expression and phagocytic capacity. Immunohistochemical analysis has been used to localize L. donovani to specific sub-populations of splenic macrophages [17]. Following intravenous high dose infection, the model currently used for most studies of VL, amastigotes are rapidly removed from circulation by marginal zone macrophages (MZM) and marginal metallophilic macrophages (MMM) which are found in the splenic marginal zone (MZ) (Box 2). The removal of amastigotes by MMM is surprising, given that MMM are normally regarded as having limited phagocytic capacity. Red pulp F4/80C macrophages also avidly phagocytose L. chagasi amastigotes [18]. Rarely, amastigotes are observed within Box 2. The marginal zone of the mouse spleen The spleen is a major secondary lymphoid organ, as well as a site for the clearance of damaged red blood cells and blood-borne pathogens. The specialized areas of lymphocyte accumulation are known as the white pulp, which contains B cells that accumulate in follicles, and the peri-arteriolar lymphoid sheath (PALS), which contain T cells that accumulate around the central arteriole. The white pulp is separated from the erythrocyte-rich red pulp by the marginal zone (MZ). The MZ of the mouse spleen comprises sinuslining reticular cells, MZ B cells, dendritic cells (DCs), marginal metallophilic macrophages (MMM) and MZ macrophages (MZM). The MMM are located on the inner border of the MZ, adjacent to the white pulp, whereas the MZM are present at the outer boundary of the MZ, adjacent to the red pulp (reviewed in Ref. [49]). In the MZ, blood flows from terminal arterioles into open sinuses, where flow is slowed down and blood-borne particles are removed by MZM and DCs with high efficiency. In addition to removing antigens from the blood, the MZ also plays a key role in directing lymphocyte traffic from the blood into the white pulp. Interest in the function of the MZ has undergone a recent resurgence following recognition of the key role this structure must play in generating acquired immune responses against blood-borne pathogens. Specialized DC subpopulations have been found within this structure, placing them in a location where antigens can be captured, and where T- and B- cell responses can be readily modulated. www.sciencedirect.com Vol.20 No.11 November 2004 the T-cell zone of the spleen, suggesting that they are phagocytosed by migratory DCs [17,19], although the frequency with which this is observed makes further characterisation of this potential interaction difficult. Studies using green-fluorescent protein (GFP)-transgenic parasites have confirmed that much of the DC response occurs in cells containing no obvious intracellular amastigotes [19]. While most studies on Leishmania uptake in the liver have focused on phagocytosis by Kupffer cells, the role of other hepatic mononuclear cells needs to be investigated. Modulation of host cell function by L. donovani Following recognition and uptake of Leishmania, mononuclear phagocytes could elect to produce a functional response. A new paradigm in immunology is that conserved microbial structures or pathogen-associated molecular patterns (PAMPs) can be recognized by a broad array of host cellular pattern-recognition receptors (PPRs). Such recognition is believed to serve both for immediate activation of innate immune defences and as a bridge for the instruction of acquired immunity (reviewed in Ref. [20]). Of the many PPRs expressed by mononuclear phagocytes, those of the Toll-like receptor (TLR) family have been under the most recent scrutiny. Pathogens as diverse as mycobacteria, virus, fungi and protozoa are all variably recognized by one or more of the ten TLRs identified to date. As a consequence of TLR recognition, most of these pathogens stimulate the production of inflammatory (TNF, IL-12p70) and/or anti-inflammatory (IL-10) cytokines, and trigger a maturation process in DCs which endows these cells with an enhanced antigenpresenting capacity and the ability to promote functional T-cell differentiation [21,22]. Leishmania donovani stands out among the range of pathogens studied, including its Leishmania relatives, as a consummately quiet invader of mononuclear phagocytes, initiating limited cytokine release from macrophages and DCs, and largely failing to activate DC maturation in vitro [23]. Whether this equates to an absence of TLR ligands on the surface of L. donovani promastigotes and/or amastigotes, or the action of a potent suppressive mechanism is unclear. Intracellular amastigotes actively inhibit cytokine responses of macrophages (at least those populations of macrophages studied in vitro) to third party stimuli, through pathways including; (i) activation of the suppressor of cytokine signalling (SOCS)-3 [24]; (ii) inhibition of p38 mitogen-activated protein kinase (MAPK) [25]; (iii) local activation of latent transforming growth factor (TGF)-b [26]; and/or (iv) through ceramide-induced modulation of extracellular signal-related kinase (ERK), activated protein-1 (AP-1) and NFkB transactivation [27]. Whether such pathways are also activated in the few DCs that become targets of infection in vivo and whether different macrophage populations have differing susceptibility to these parasite evasion tactics are important gaps in our knowledge. Examination of DCs ex vivo at various times after infection indicates that maturation occurs at the population level, although most mature DCs are apparently not infected by parasites [19]. DC maturation following infection has also been demonstrated to be at Review TRENDS in Parasitology least partly dependent on Myd88 signalling [19] and, at least for L. major infection, Myd88K/K mice are more susceptible to infection than that by wild-type mice [28–30]. However, because Myd88 is involved in signalling through other key cytokine receptors including IL-1R [31], and TLRs have endogenous ligands such as heat-shock proteins [32] and defensins [33], these experiments do not conclusively demonstrate TLR-mediated DC activation in vivo. A recent report indicates that lipophosphoglycan of L. major might however be the first defined TLR ligand in these parasites [29]. T cell–DC interactions and the spleen immune response Although a low dose model of infection has recently been established, most studies on the early immune response to L. donovani and L. infantum have employed high dose (107) inoculation of amastigotes. Under these conditions, there are a few indications that initiation of immune responses to this parasite are anything other than would have been expected from studies of simple non-microbial antigens delivered with weak adjuvant. Following infection, there is a rapid and transient burst of IL-12p70 secretion by splenic DC, which is localized within the T-cell-rich periarteriolar lymphoid sheath (PALS) (Figure 2). The appearance of IL-12p70-producing DC in the PALS parallels an increase in high affinity IL-2 receptors on CD4C T cells, suggesting a classical model of DC-mediated T-cell activation [17]. Both IL-12p40 and IL-12p70 production peaks at five hours post-infection (p.i.) and then diminishes, with IL-12p70 being produced exclusively by CD8C DC in a T cell-dependent, yet surprisingly CD40-independent, manner. Early DC-derived IL-12p70 production is important for the activation of host-protective CD4C and/or CD8C T cells because IL-12 neutralisation during the first few days of infection results in enhanced parasite growth [34]. The data also suggest that there is rapid induction of IL-10 in the MZ [18], and that this might contribute significantly to the establishment of infection [35]. CD8C T-cell responses are also prominent in the early response to L. donovani, but pathways for the induction of CD8C T cells specific for this exogenous parasite have only recently become apparent. Examination of the cell biology of L. donovani phagocytosis by macrophages has demonstrated that the loading of parasite-derived antigens onto major histocompatibility complex (MHC) Class I molecules might be facilitated by endoplasmic reticulum-mediated phagocytosis [36,37]. In addition, CD8C DC might acquire Leishmania antigens for cross-presentation by phagocytosis of infected macrophages or their remnants [38]. The extent to which responses by non-classical T cells [e.g. gd T cells and natural killer (NK) T cells] are activated in the spleen following infection is not yet known. However, a recent report suggests that, among the many other cell surface molecules whose expression can be manipulated by Leishmania, L. donovani infection of DCs inhibits expression of CD1 [39]. It should be considered that in vivo, these events occur in a complex microenvironment, increasing the extent to which various cell types can communicate together (Figure 2). Furthermore, whether these conclusions concerning the initiation of the immune www.sciencedirect.com Vol.20 No.11 November 2004 527 response to L. donovani and L. infantum will be confirmed following further studies using low-dose needle infections or natural sandfly infections remains to be seen. The spleen as a site of chronic inflammation Following high-dose intravenous infection with L. donovani, the first 14 days progress normally in immunological terms. There is evidence of extensive T-cell activation as germinal centres develop rapidly, antibody titres begin to increase albeit slowly and recall in vitro T-cell responses can be readily detected. From Day 1–14 p.i., the growth of amastigotes appears minimal or is matched by death. Nevertheless, immune responses generated over this time are clearly ineffective at eliminating amastigotes; within three weeks p.i., the situation changes dramatically. To date, three main events have been characterised that occur between Day 14 and Day 21 p.i.: (i) alterations to MZ structure; (ii) altered stromal cell function; and (iii) loss of DC migration (see Figure 3). The functional consequences of these changes are dramatic. A major advance in understanding and unifying these events came with the identification of TNF as a primary mediator of splenic pathology and immune dysfunction. Alterations to MZ structure The splenic MZ is a primary site for parasite clearance and is also involved in the regulation of lymphocyte homing (Box 2). At the onset of the chronic phase of infection, the MZ is subject to extensive, but selective remodelling. Technically, it is often difficult to show that a cell type is lost from a tissue using histological or flow cytometric analysis based on phenotypic markers because it can always be argued that downregulation of such markers has occurred. However, in the case of MZM, it is possible to specifically label these cells and in a stable manner by virtue of their uptake of injected Indian ink. By this approach, MZM, but not MMM, were rapidly depleted from the MZ. This process was mediated by TNF because TNFK/K mice or mice receiving TNF blockade largely retained their MZM. As predicted, the loss of MZ macrophages resulted in severely restricted migration of lymphocytes into the white pulp during VL [40]. Altered stromal cell function The PALS comprises a reticular network of collagen fibres ensheathed by fibroblastic reticular cells, which extend to connective tissue spaces of the arterioles [41]. This network of tubular stromal cells is a conduit system that is accessible for small molecules from the blood. The stromal cells in the PALS express gp38 [42] and ER-TR7 [43], and are a major source of the constitutively expressed lymphoid chemokines CCL21 and CCL19, which mediate recruitment of CCR7-expressing naı̈ve T cells and mature DCs. These chemokines are present within the tubular system, as well as on the surface of the stromal cells that enfold it, providing a framework along which T cells and DCs can migrate within the PALS. At around the same time as MZMs are lost from the spleen following L. donovani infection, gp38C stromal cells in the PALS also disappear. Again, TNF mediates the loss of gp38C stromal cells in the PALS, with a resultant significant Review 528 TRENDS in Parasitology Vol.20 No.11 November 2004 (a) (b) (iv) (v) (ii) (i) MZ (iii) PALS MZ PALS Key: gp38+ stromal cell CCL21 and/or CCL19 MMM TNF-α T cell Central arteriole Reticular fibers Endothelial cell MZM IL-10 DC Leishmania TRENDS in Parasitology Figure 3. Changes to splenic architecture during chronic infection. (a) The structure of the spleen remains normal during acute stages of infection. The MZ comprises two discrete populations of macrophages: (i) the MZM at the outer boundary; and (ii) the MMM in close proximity to the PALS. Within the PALS, T-zone gp38C stromal cells and the endothelium of the central arteriole are rich sources of the constitutive chemokines CCL19 and CCL21, which attract CCR7C DCs and T cells from the MZ into the PALS. (b) The disrupted architecture of the spleen during chronic infection. Excess TNF production, probably from immigrant macrophages (i) leads to destruction of gp38 stromal cells, loss of the reticular matrix they produce, and a loss of CCL19 and CCL21 expression (ii). The high levels of TNF production also positively regulate IL-10 production. It is not known whether TNF induces IL-10 production by different subsets of macrophages (e.g. MMM) (iii) or whether the same macrophages make both TNF and IL-10 (iv). High levels of IL-10 downregulate CCR7 expression on DC, inhibiting their ability to migrate into the PALS (v). Arrows indicate likely cellular sources and targets of TNF and IL-10. Abbreviations: DC, dendritic cells; IL, interleukin; IL-12p40, interleukin-12/23 p40 subunit; MMM, marginal metallophilic macrophages; MZ, marginal zone; MZM, marginal zone macrophages; PALS, peri-arteriolar lymphoid sheath; TNF, tumour necrosis factor. decrease in production of the constitutively expressed chemokines CCL19 and CCL21 [44]. Loss of DC migration The increased level of TNF in the spleen also results in increased production of the anti-inflammatory cytokine IL-10, and this cytokine induces downregulation of the crucial chemokine receptor CCR7 on the surface of DC, preventing their migration into the PALS [44]. When mature DCs from naı̈ve mice were administered to mice with VL, significant reductions in splenic parasite burdens were observed [44], indicating that the failure of DC migration into the PALS during L. donovani infection has an important impact on disease outcome. These findings provide a rationale for delivering vaccines by antigenloaded DCs or immunotherapy using DCs. In addition to these structural changes, there is other evidence of a changing immune response, as follows: (i) T helper cell type (Th) 1 and Th2 cytokine profiles could shift in their balance slightly (although they remain far from polarised) [45]; (ii) local TGF-b levels are increased and with apparent differences in kinetics in spleen and liver [46,47]; (iii) monocyte chemoattractant protein 1 (MCP-1) synthesis is sustained, compatible with increased macrophage recruitment [5]; and (vi) local haematopoietic www.sciencedirect.com activity is dramatically increased [48]. What is less clear and important to understand is to what extent such events are the consequence of, or precede the breakdown in, lymphoid microarchitecture, and to what extent each of these factors contributes to the relative levels of organspecific immunity versus persistence (alone or in combination with other factors)? Concluding remarks Several issues will need to be addressed before the full basis for Leishmania persistence and the varied immunological responses seen in different tissues is fully understood (Box 3). Among these many outstanding questions, the issue of mononuclear phagocyte heterogeneity is probably paramount. However, studying these cells in situ in their unique locations poses great experimental challenges. Such studies will be important to ensure that future development of vaccines, immunomodulators and chemotherapy takes into account the various requirements for host protection in different tissue sites. The development of new infection models and new tools to study immune responses to Leishmania is progressing fast, such that investigators will soon have the benefit of the many tools (e.g. TCR transgenic models) cherished by those who study viral and bacterial immune responses Review TRENDS in Parasitology Box 3. Outstanding questions † What receptors govern amastigote internalisation by the heterogeneous subpopulations of mononuclear phagocytes found in the spleen, liver and other target tissue of Leishmania infection? † Do all Leishmania parasites express Toll-like receptor ligands? † What is the relative importance of each of the numerous evasion strategies that have been identified in vitro for long-term parasite persistence in vivo? † Will our view of the early immune response to Leishmania donovani hold true upon examination of infection by natural transmission? † What are the key immunological events that switch the spleen into a state of chronic inflammation? † What governs the local regulation of and/or cellular responsiveness to tumour necrosis factor (TNF)? It is host protective in the liver, but in the spleen it causes pathology? † Can therapeutic targeting of TNF aimed at limiting pathology be balanced with the need to retain some TNF function for optimal immunity against both Leishmania and possible latent infections (e.g. tuberculosis)? in vivo. On a more practical note, our hypothesis that pathology is intimately linked to parasite persistence, and the observations that such pathology results from the action of TNF together suggest that intervention to block TNF, as with other chronic inflammatory diseases [50], could have some beneficial effects. Indeed, TNF blockade with pentoxyfylin has some remarkable clinical effects in drug-resistant cases of chronic cutaneous leishmaniasis [51]. However, given the requirement for TNF for protection against Leishmania in the liver of mice with experimental VL, and the potential for reactivation of tuberculosis in patients with TNF blockade, caution would be needed in evaluating this approach in countries where both VL and tuberculosis are common. Acknowledgements Work in the authors’ laboratories is funded by grants from the British Medical Research Council, The Wellcome Trust, the Australian National Health and Medical Research Council, and the UNDP/World Bank/WHO Special Programme for Research and Training in Tropical Diseases (TDR). M.A. was a recipient of a Wellcome Trust International Fellowship; C.E. is a recipient of a NHMRC Career Development Fellowship. References 1 Engwerda, C.R. and Kaye, P.M. (2000) Organ-specific immune responses associated with infectious disease. Immunol. Today 21, 73–78 2 Murray, H.W. (2001) Tissue granuloma structure-function in experimental visceral leishmaniasis. Int. J. Exp. Pathol. 82, 249–267 3 Smelt, S.C. et al. (1997) Destruction of follicular dendritic cells during chronic visceral leishmaniasis. J. Immunol. 158, 3813–3821 4 Leclercq, V. et al. (1996) The outcome of the parasitic process initiated by Leishmania infantum in laboratory mice: a tissue-dependent pattern controlled by the Lsh and MHC loci. J. Immunol. 157, 4537–4545 5 Rousseau, D. et al. (2001) Sustained parasite burden in the spleen of Leishmania infantum-infected BALB/c mice is accompanied by expression of MCP-1 transcripts and lack of protection against challenge. Eur. Cytokine Netw. 12, 340–347 6 Wilson, M.E. et al. (1996) Local suppression of IFN-gamma in hepatic granulomas correlates with tissue-specific replication of Leishmania chagasi. J. Immunol. 156, 2231–2239 7 Tumang, M.C. et al. (1994) Role and effect of TNF-alpha in experimental visceral leishmaniasis. J. Immunol. 153, 768–775 www.sciencedirect.com Vol.20 No.11 November 2004 529 8 Ahmed, S. et al. (2003) Intradermal infection model for pathogenesis and vaccine studies of murine visceral leishmaniasis. Infect. Immun. 71, 401–410 9 Zhang, W.W. et al. (2003) Comparison of the A2 gene locus in Leishmania donovani and Leishmania major and its control over cutaneous infection. J. Biol. Chem. 278, 35508–35515 10 Stafford, J.L. et al. (2002) Macrophage-mediated innate host defense against protozoan parasites. Crit. Rev. Microbiol. 28, 187–248 11 Chava, A.K. et al. (2004) Identification of sialic acids on Leishmania donovani amastigotes. Biol. Chem. 385, 59–66 12 Santos, I.K. et al. (2001) Mannan-binding lectin enhances susceptibility to visceral leishmaniasis. Infect. Immun. 69, 5212–5215 13 Bodman-Smith, K.B. et al. (2002) C-reactive protein-mediated phagocytosis of Leishmania donovani promastigotes does not alter parasite survival or macrophage responses. Parasite Immunol. 24, 447–454 14 Colmenares, M. et al. (2002) Dendritic cell (DC)-specific intercellular adhesion molecule 3 (ICAM-3)-grabbing nonintegrin (DC-SIGN, CD209), a C-type surface lectin in human DCs, is a receptor for Leishmania amastigotes. J. Biol. Chem. 277, 36766–36769 15 Geijtenbeek, T.B. et al. (2002) DC-SIGN, a C-type lectin on dendritic cells that unveils many aspects of dendritic cell biology. J. Leukoc. Biol. 71, 921–931 16 Colmenares, M. et al. (2004) The dendritic cell receptor DC-SIGN discriminates among species and life cycle forms of Leishmania. J. Immunol. 172, 1186–1190 17 Gorak, P.M. et al. (1998) Dendritic cells, but not macrophages, produce IL-12 immediately following Leishmania donovani infection. Eur. J. Immunol. 28, 687–695 18 Melby, P.C. et al. (2001) Leishmania donovani: evolution and architecture of the splenic cellular immune response related to control of infection. Exp. Parasitol. 99, 17–25 19 De Trez, C. et al. (2004) Myd88-dependent in vivo maturation of splenic dendritic cells induced by Leishmania donovani and other Leishmania species. Infect. Immun. 72, 824–832 20 Janeway, C.A., Jr. and Medzhitov, R. (2002) Innate immune recognition. Annu. Rev. Immunol. 20, 197–216 21 Reis e Sousa, C. (2004) Toll-like receptors and dendritic cells: for whom the bug tolls. Semin. Immunol. 16, 27–34 22 Sher, A. et al. (2003) Shaping the immune response to parasites: role of dendritic cells. Curr. Opin. Immunol. 15, 421–429 23 McDowell, M.A. et al. (2002) Leishmania priming of human dendritic cells for CD40 ligand-induced interleukin-12p70 secretion is strain and species dependent. Infect. Immun. 70, 3994–4001 24 Bertholet, S. et al. (2003) Leishmania donovani-induced expression of suppressor of cytokine signaling 3 in human macrophages: a novel mechanism for intracellular parasite suppression of activation. Infect. Immun. 71, 2095–2101 25 Junghae, M. and Raynes, J.G. (2002) Activation of p38 mitogenactivated protein kinase attenuates Leishmania donovani infection in macrophages. Infect. Immun. 70, 5026–5035 26 Gantt, K.R. et al. (2003) Activation of TGF-beta by Leishmania chagasi: importance for parasite survival in macrophages. J. Immunol. 170, 2613–2620 27 Ghosh, S. et al. (2002) Leishmania donovani suppresses activated protein 1 and NF-kappaB activation in host macrophages via ceramide generation: involvement of extracellular signal-regulated kinase. Infect. Immun. 70, 6828–6838 28 Debus, A. et al. (2003) High levels of susceptibility and T helper 2 response in MyD88-deficient mice infected with Leishmania major are interleukin-4 dependent. Infect. Immun. 71, 7215–7218 29 de Veer, M.J. et al. (2003) MyD88 is essential for clearance of Leishmania major: possible role for lipophosphoglycan and Toll-like receptor 2 signaling. Eur. J. Immunol. 33, 2822–2831 30 Muraille, E. et al. (2003) Genetically resistant mice lacking MyD88-adapter protein display a high susceptibility to Leishmania major infection associated with a polarized Th2 response. J. Immunol. 170, 4237–4241 31 Hawn, T.R. et al. (2002) Leishmania major activates IL-1 alpha expression in macrophages through a MyD88-dependent pathway. Microbes Infect. 4, 763–771 32 Vabulas, R.M. et al. (2002) HSP70 as endogenous stimulus of the Toll/interleukin-1 receptor signal pathway. J. Biol. Chem. 277, 15107–15112 Review 530 TRENDS in Parasitology 33 Biragyn, A. et al. (2002) Toll-like receptor 4-dependent activation of dendritic cells by beta-defensin 2. Science 298, 1025–1029 34 Engwerda, C.R. et al. (1998) Neutralization of IL-12 demonstrates the existence of discrete organ-specific phases in the control of Leishmania donovani. Eur. J. Immunol. 28, 669–680 35 Murphy, M.L. et al. (2001) IL-10 mediates susceptibility to Leishmania donovani infection. Eur. J. Immunol. 31, 2848–2856 36 Houde, M. et al. (2003) Phagosomes are competent organelles for antigen cross-presentation. Nature 425, 402–406 37 Gagnon, E. et al. (2002) Endoplasmic reticulum-mediated phagocytosis is a mechanism of entry into macrophages. Cell 110, 119–131 38 Jung, S. et al. (2002) In vivo depletion of CD11c(C) dendritic cells abrogates priming of CD8(C) T cells by exogenous cell-associated antigens. Immunity 17, 211–220 39 Amprey, J.L. et al. (2004) Inhibition of CD1 expression in human dendritic cells during intracellular infection with Leishmania donovani. Infect. Immun. 72, 589–592 40 Engwerda, C.R. et al. (2002) A role for tumor necrosis factor-alpha in remodeling the splenic marginal zone during Leishmania donovani infection. Am. J. Pathol. 161, 429–437 41 Nolte, M.A. et al. (2003) A conduit system distributes chemokines and small blood-borne molecules through the splenic white pulp. J. Exp. Med. 198, 505–512 42 Farr, A.G. et al. (1992) Characterization and cloning of a novel glycoprotein expressed by stromal cells in T-dependent areas of peripheral lymphoid tissues. J. Exp. Med. 176, 1477–1482 Vol.20 No.11 November 2004 43 Van Vliet, E. et al. (1986) Reticular fibroblasts in peripheral lymphoid organs identified by a monoclonal antibody. J. Histochem. Cytochem. 34, 883–890 44 Ato, M. et al. (2002) Defective CCR7 expression on dendritic cells contributes to the development of visceral leishmaniasis. Nat. Immunol. 3, 1185–1191 45 Mukherjee, P. et al. (2003) Infection pattern and immune response in the spleen and liver of BALB/c mice intracardially infected with Leishmania donovani amastigotes. Immunol. Lett. 86, 131–138 46 Wilson, M.E. et al. (2002) The TGF-beta response to Leishmania chagasi in the absence of IL-12. Eur. J. Immunol. 32, 3556–3565 47 Gomes, N.A. et al. (2000) TGF-beta mediates CTLA-4 suppression of cellular immunity in murine kalaazar. J. Immunol. 164, 2001–2008 48 Cotterell, S.E. et al. (2000) Enhanced hematopoietic activity accompanies parasite expansion in the spleen and bone marrow of mice infected with Leishmania donovani. Infect. Immun. 68, 1840–1848 49 Kraal, G. (1992) Cells in the marginal zone of the spleen. Int. Rev. Cytol. 132, 31–74 50 Feldmann, M. and Maini, R.N. (2003) Lasker Clinical Medical Research Award. TNF defined as a therapeutic target for rheumatoid arthritis and other autoimmune diseases. Nat. Med. 9, 1245–1250 51 Bafica, A. et al. (2003) American cutaneous leishmaniasis unresponsive to antimonial drugs: successful treatment using combination of N-methilglucamine antimoniate plus pentoxifylline. Int. J. Dermatol. 42, 203–207 World Health Organisation targets leishmaniasis in Afghanistan The World Health Organisation (http://www.who.int/en/), in conjunction with the Massoud Foundation and HealthNet International (http://www.heathnetinternational.org/), has stepped in to curb the current epidemic of cutaneous leishmaniasis in Afghanistan before it escalates beyond control. A donation from the Belgian government made this intervention possible and the initiative aims to reduce the incidence of the disease within the next two years. The past two decades of conflict have eroded away any pre-existing leishmaniasis control programmes in the country. Environmental damage and poor sanitary conditions have resulted in the proliferation of breeding sites for the vector of the Leishmania parasite, the sand fly, and the influx of large numbers of displaced people, who possess little or no immunity to the disease, threatens to worsen the situation. As an immediate measure, WHO and its partners are combining drug treatment with the distribution of 16 000 insecticide-treated bednets which will help to protect >30 000 people from sandflies. Initially, the program will focus on Kabul, the largest centre of cutaneous leishmaniasis in the world and accountable for one-third of the 200 000 cases reported in Afghanistan. For more information, please go to: http://www.who.int/mediacentre/releases/2004/pr55/en/ Written by Anthony Li ([email protected]) www.sciencedirect.com