* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download The sixth sense: hematopoietic stem cells detect danger through
Immune system wikipedia , lookup
Molecular mimicry wikipedia , lookup
Lymphopoiesis wikipedia , lookup
Adaptive immune system wikipedia , lookup
Polyclonal B cell response wikipedia , lookup
Psychoneuroimmunology wikipedia , lookup
Cancer immunotherapy wikipedia , lookup
Immunosuppressive drug wikipedia , lookup
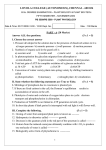
From www.bloodjournal.org by guest on June 16, 2017. For personal use only. Review article The sixth sense: hematopoietic stem cells detect danger through purinergic signaling Lara Rossi,1 Valentina Salvestrini,1 Davide Ferrari,2 Francesco Di Virgilio,2 and Roberto M. Lemoli1 1Department of Hematology and Oncological Sciences, L. and A. Seràgnoli, Institute of Hematology, University of Bologna and S. Orsola-Malpighi Hospital, Bologna, Italy; and 2Department of Experimental and Diagnostic Medicine, Section of General Pathology and Interdisciplinary Center for the Study of Inflammation, University of Ferrara, Ferrara, Italy Over the past decade, extracellular nucleotides (such as ATP and UTP) have emerged as key immunomodulators. This family of molecules, already known for its key metabolic functions, has been the focus of intense investigation that has unambiguously shown its crucial role as mediators of cell-to-cell communication. More recently, in addition to its involvement in inflammation and immunity, purinergic signaling has also been shown to modulate BM-derived stem cells. Extracel- lular nucleotides promote proliferation, CXCL12-driven migration, and BM engraftment of hematopoietic progenitor and stem cells. In addition, purinergic signaling acts indirectly on hematopoietic progenitor and stem cells by regulating differentiation and release of proinflammatory cytokines in BM-derived human mesenchymal stromal cells, which are part of the hematopoietic stem cell (HSC) niche. HSC research has recently blended into the field of immunology, as new findings highlighted the role played by immunologic signals (such as IFN-␣, IFN-␥, or TNF-␣) in the regulation of the HSC compartment. In this review, we summarize recent reports unveiling a previously unsuspected ability of HSCs to integrate inflammatory signals released by immune and stromal cells, with particular emphasis on the dual role of extracellular nucleotides as mediators of both immunologic responses and BM stem cell functions. (Blood. 2012;120(12):2365-2375) Introduction Living organisms are constantly exposed to foreign, and sometimes harmful, agents. To protect tissues from damage and preserve homeostasis, multicellular organisms have developed an array of defense responses of which inflammation is a major manifestation. As part of this defense mechanism, inflammation is instrumental for mounting an effective innate and adaptive immune response. Terminally differentiated cells (granulocytes, monocytes/macrophages, dendritic cells, B- and T-lymphocytes) have classically been considered the principal players in inflammation and immunity. Conversely, hematopoietic stem cells (HSCs), from which all immune and inflammatory cells derive, are usually thought not to be part of the immune system. Localized in the nurturing environment of the BM niche, HSCs were thought to reside within an “immunologic sanctuary,” protected from the insults affecting peripheral tissues. However, recent findings suggest that HSCs are not confined in a “splendid isolation”: BM-HSCs and circulating HSCs can sense the presence of danger or stress signals in the surrounding microenvironment and switch to an activated state or reach injured tissues in need of repair.1,2 Therefore, HSCs respond to early mediators of inflammation and distress that were so far thought to be active on immune cells only, such as TNF-␣, IFNs, Toll-like receptor (TLR) ligands and, most interestingly, extracellular nucleotides (eNTPs). From the evolutionary standpoint, nucleotides are among the most ancient biologic molecules; thus, it is not surprising that they have been used by living organisms for multiple purposes: storage and transmission of genetic information, energy metabolism, and extracellular communication.3 eNTPs compose both extracellular purines (ATP and its derivatives, ADP and adenosine) and extracellular pyrimidines (uridine-5⬘-phosphate [UTP] and [UDP]), which intervene in a variety of biologic processes by binding NTPspecific cell-membrane receptors, collectively named purinergic receptors. The presence of purinergic signaling in taxa as diverse as mammals, plants, yeasts and bacteria suggests that nucleotides are indeed an archaic, ubiquitous, communication system.4,5 However, their messenger role has been realized comparatively late, and only thanks to the pioneering studies of Geoffrey Burnstock in the central and peripheral nervous system.6 It is now well established that nucleotides mediate intercellular communication in virtually all tissues and typify one of the most important indicators of cell stress in the pericellular environment.7 In the hematopoietic and immune systems, eNTPs act as potent immunomodulators of neutrophil, monocyte, macrophage, dendritic cell, and T-lymphocyte responses.8 In addition, eNTPs drive blood cell proliferation and differentiation at different levels, including the compartment of hematopoietic progenitors and stem cells (HPSCs). Here we discuss how HSCs react to signals of cell injury and inflammation to mount an integrated response to pathogens and tissue damage. In our view, purinergic signaling activated by eNTPs emerges as a key element bridging inflammation to HSC activation. Submitted April 5, 2012; accepted July 2, 2012. Prepublished online as Blood First Edition paper, July 11, 2012; DOI 10.1182/blood-2012-04-422378. © 2012 by The American Society of Hematology BLOOD, 20 SEPTEMBER 2012 䡠 VOLUME 120, NUMBER 12 How immunology blends into stem cell biology: the effect of immunomodulators on HSCs Lying at the roots of the hematopoietic system, HSCs are a reservoir of rare, multipotent stem cells that provide a continuous supply of cells circulating in the peripheral blood (PB), such as erythrocytes, platelets, lymphoid cells, and myeloid cells. Under 2365 From www.bloodjournal.org by guest on June 16, 2017. For personal use only. 2366 ROSSI et al steady-state conditions, HSCs are highly quiescent cells that divide infrequently and are found mainly in the G0 phase of the cell cycle.9 Despite dormancy being the privileged status for HSCs, these cells retain a considerable resilience that enables them to adjust their cell-cycle dynamics and undergo proliferation when needed. Hemorrhagic stress is among the strongest triggers of HSC proliferation, aiming at replenishing the population of circulating erythrocytes lost through bleeding.10 Similarly, chemotherapic drugs (such as 5-fluorouracil or hydroxyurea), which kill proliferating hematopoietic progenitors, recruit HSCs out of quiescence to reconstitute the whole downstream subset of differentiated cells.11 Interestingly, increased HSC proliferation has also been observed in response to immunologic stress, such as infections. Under these conditions, HSCs skew their differentiation toward lymphoid and/or myeloid cells to maintain an efficient army of pathogenfighting cells, until infectious agents are cleared. In analogy to stimulation of erythropoiesis by massive bleeding, pathogeninduced HSC proliferation has traditionally been interpreted as a physiologic reaction to infections, aimed at counterbalancing the loss of immune cells from PB. However, it is now clear that HSCs do not only react to the depletion of differentiated PB cells; rather, the HSC compartment reacts directly to danger signals and inflammatory cytokines released by pathogens, tissues, and resident immune cells. Several recent studies highlighted the role of IFNs as major regulators of HSC cell cycle.12-14 Both IFN-␣ and IFN-␥ stimulate HSC proliferation in mice,14,15 and HSCs from IFN-␥-deficient mice are more quiescent and engraft better in transplantation assays than those from wild-type animals.12 Conversely, overactivation of IFN pathway impairs HSC functions and decreases their engraftment, suggesting a link between chronic infections and HSC exhaustion.16 The impact of infections on HSCs is also shown by the dual role of TNF-␣ on their proliferation and differentiation. Depending on the context, TNF-␣ plays inhibitory or stimulatory effects on HSCs.17,18 For instance, murine Tnfrsf1a⫺/⫺ HSCs perform poorly in competitive repopulation assays because of self-renewal defects. On the other hand, excessive activation of TNF-␣ signaling is associated with impaired hematopoiesis,16 suggesting that any drastic imbalance in TNF-␣ signaling may be detrimental for HSC function. HSCs sensing danger: the role of PRRs Modulation of HSC functions by inflammatory cytokines is of great interest, but not novel and surprising by itself. More interesting and unexpected is the ability of HPSCs to respond directly to factors released by pathogens or by injured tissues, in other words to sense danger directly, unveiling a new skill for these cells and a potentially novel function in the activation of first-line immunity.1 Traditionally, immunology has focused on the self/non–selfdiscrimination. However, it is now gaining support the view that immune responses would be more efficient if discrimination was based not only on “foreignness” but also on “dangerousness,” as proposed by Matzinger’s danger model.19 Multicellular organisms have evolved a wide array of extracellular receptors, named pattern recognition receptors (PRRs), specialized in recognizing pathogens or molecules released from injured cells (danger signals).20 PRRs bind viral or microbial pathogen-associated molecular patterns (PAMPs, such as lipopolysaccharide, peptidogycans, single-strand RNA, or unmethylated CpG motifs), and may also detect damageassociated molecular patterns. Damage-associated molecular pat- BLOOD, 20 SEPTEMBER 2012 䡠 VOLUME 120, NUMBER 12 terns are endogenous molecules released by damaged or distressed tissues, may be of intracellular or extracellular origin, and include proteins (such as calgranulins) and nonprotein molecules (uric acid, reactive oxygen species, heparin sulfate, biglycans, tenascin C, and eNTPs).21 These molecules are collectively known as alarmins, a term recently coined to indicate endogenous molecules that alert immunity on tissue injury.22 Vertebrates possess a vast array of conserved PRRs (TLRs, RIG-I–like receptors, NOD-like receptors, AIM2-like receptors, and purinergic receptors), mostly expressed by monocytes, macrophages, neutrophils, and dendritic cells. Nonetheless, recent evidence indicates that also nonimmune cells, such as endothelial cells, and, more recently, HSCs express PRRs. These findings suggest that the network created by PAMPs, damage-associated molecular patterns, and PRRs transversally affects the whole hematopoietic system, from the compartment of immature HSCs up to the terminally differentiated immune cells.23,24 Through this signaling network, HSCs can directly sense a proinflammatory microenvironment even before inflammatory cytokines are released, driving a swift response to pathogens and accelerating the replenishment of circulating immune cells. As a direct consequence, repeated or chronic infections could negatively affect HSC long-term survival. As recently demonstrated in a model of chronic low-grade infection,25 the prolonged systemic exposure to TLR ligands is detrimental to long-term HSCs, thus highlighting a possible link between HSCs defects and different disease states, including infection, inflammation, autoimmune diseases, and aging.26-28 Purinergic danger signals and HSCs Extracellular nucleotides as alarmins Endogenous danger signals, collectively named alarmins, originate from cells or from the extracellular matrix. Those of cellular origin share a few fundamental features: (1) are rapidly released on necrotic cell death; (2) can be released either passively or through specialized efflux pathways; (3) recruit, by chemotaxis, target cells and activate innate and adaptive immune responses; (4) promote recovery from tissue injuries and restore homeostasis; and (5) their activity is counterbalanced by inhibitory pathways that avoid inflammatory loops.22 Purinergic signaling fulfils all these requirements, as nucleotides (1) are released into the extracellular environment on tissue injuries and cells death (passively or via specialized pathways)29; (2) stimulate immune cell chemotaxis and recruitment at inflammation sites by binding nucleotide-selective receptors, also known as purinergic receptors or P2 receptors (P2Rs)30-32; (3) activate innate and adaptive immune responses by stimulating antigen-presenting cells, neutrophils, monocytes- and macrophages8; (4) drive tissue recovery by stimulating cell proliferation33; and (5) promote resolution of the immune response by activating anti-inflammatory pathways dependent on ATP degradation products (eg, adenosine).34,35 Similarly to other inflammatory cascades, purinergic signaling progresses through 3 phases: initiation, amplification, and resolution (Figure 1). Initiation: release of eNTPs. Several mechanisms responsible for nucleotide release into the extracellular fluids have been described so far. Extensive tissue injury, traumatic shock, or inflammation produces massive, nonspecific leakage of nucleotides because of cell lysis.8 However, nonlytic mechanisms are concurrently activated after stimulation with PAMPs. ATP, ADP, and other nucleotides are released via constitutive or stimulated exocytosis, From www.bloodjournal.org by guest on June 16, 2017. For personal use only. BLOOD, 20 SEPTEMBER 2012 䡠 VOLUME 120, NUMBER 12 PURINERGIC SIGNALING AND INFLAMMATION IN HSCs 2367 Figure 1. The role of extracellular ATP and purinergic signaling in inflammation. On insults inducing cell damage and stress, cells can release into the extracellular environment nucleotides, such as ATP. Once released, ATP can take part in all the different steps of inflammatory responses. 1. Initiation: after being secreted into the pericellular environment, ATP can act as a danger signal and alert the immune system, thus helping initiate the inflammatory response. 2. Progression: ATP can bind to P2 receptors exposed on the cell membrane of target cells and induce granulocyte and macrophage chemotactic attraction toward the inflammatory focus, as well as activation of antigen-presenting cells. These responses induce the activation of both the innate and the adaptive branches of the immune system, leading to the amplification of the inflammatory response. 3. Resolution: under physiologic conditions, inflammatory responses need to be restrained from self-amplifying without control. To protect tissues from extended damages, anti-inflammatory responses are activated. With specific regard to purinergic signaling, CD39 and CD73 endonucleosidases concur to down-regulate inflammation by hydrolyzing ATP in adenosine, with a double effect: prevent ATP from further activate P2R signaling and increase adenosine concentration, which activates antiinflammatory responses by binding to P1 receptors. as well as through poorly selective plasma membrane channels, such as connexins and pannexins.29 P2Rs themselves may participate in ATP release, as there is convincing evidence that the P2X7R subtype allows nucleotide efflux.36,37 It is now clear that virtually all cell types (hematopoietic cells included) constitutively release ATP to maintain a steady nucleotide concentration in the nanomolar range in the pericellular environment. However, different cell types release ATP in response to different stimuli (eg, erythrocytes in response to deformation, endothelial cells to shear stress, macrophage to endotoxin, osteoblasts, to mechanical loading). Thus, it is conceivable that eNTP release is a general signal of cellular stress, subsequently decoded by other cells to ignite inflammation.8,38 It is probable that a steady ATP level causes a tonic stimulation of P2Rs that is responsible for chronic, low-level, cellular activation. This is clearly shown by the in activity of ATP-hydrolyzing enzymes (eg, apyrase), which cause a decrease in cytoplasmic Ca2⫹ concentration or mitochondrial potential. Conversely, transient increases in eNTP concentration above steady-state levels are induced by several mechanical (shear stress, osmotic swelling, cell shrinking), chemical (reactive oxygen species, xenobiotics) or biologic agents (lipopolysaccharide)39,40 (Figure 1). Although initial evidence dates back to several decades ago, it is only during the last 10 years that the role of ATP as extracellular messenger has been generally accepted despite some initial skepticism.41 One of the main arguments against the involvement of ATP in extracellular communication is the lack of an unequivocal in vivo demonstration that ATP is present in the extracellular space and that its levels are modulated during pathophysiologic responses. The very high cellular ATP content and its instability make ATP measurement very liable to sampling artifacts secondary to tissue manipulation. These experimental limitations have been finally overcome by developing ATP-sensing probes capable of detecting ATP in the pericellular space, where most of the biologic activity of eNTPs is localized.42,43 This innovative probe is a modified firefly luciferase engineered with a leader sequence and a glycosylphosphatidylinositol anchor, which enables routing and localization on the outer surface of the plasma membrane. Thanks to this bioluminescent ATP probe, pmeLUC (plasma membrane luciferase), we have been able to perform noninvasive sampling of eATP in vivo and to demonstrate conclusively that eATP is present at sites of inflammation and in tumor microenvironments.43 Similar detection assays for extracellular uridine nucleotides, based on the highly selective UDP-glucose pyrophosphorylase-coupled reaction, have been developed by other groups.44 This technical breakthrough paved the way for a systematic in vivo investigation of eATP involvement in inflammation and immunity and should also allow measurements in the BM. Average eATP concentration ranges under steady-state conditions in the 10⫺9-10⫺6M range. In proximity of the plasma membrane, it is expected to be higher, especially in protected pouches, which do not easily equilibrate with the pericellular space, but as of now it is very difficult to give From www.bloodjournal.org by guest on June 16, 2017. For personal use only. 2368 ROSSI et al BLOOD, 20 SEPTEMBER 2012 䡠 VOLUME 120, NUMBER 12 Figure 2. The family of purinergic receptors: classification, structure, and signaling pathway. The family of purinergic receptors comprises 2 major groups of membrane receptors: adenosine-activated P1 receptors (P1Rs) and nucleotide-activated P2 receptors (P2Rs). Based on pharmacologic profile and molecular structure, 2 subfamilies have been identified within P2Rs, namely, P2XRs and P2YRs. P2XRs (composing 7 subtypes, P2X1R through P2X7R) are trimeric ATP-gated plasma membrane channels, whereas P2YRs are classic G protein-coupled receptors. Based on their ligand selectivity, P2YRs are further subdivided in subtypes preferentially responding to ATP (human and rodent P2Y1R, and human P2Y11R), to ADP (P2Y12R and P2Y13R), uridine5⬘-phosphate (UTP) and UDP (human P2Y4R and P2Y6R), and ATP and UTP (human and rodent P2Y2R and rodent P2Y4R), whereas human P2Y14R binds sugar-linked nucleotides, such as UDP-glucose and UDP-galactose. Two different signaling cascades are associated with P2YRs: some subtypes mainly couple to Gq proteins (P2Y1R, P2Y2R, P2Y4R, P2Y6R, and P2Y11R), whereas others preferentially couple to Gi proteins (P2Y11R, P2Y12R, P2Y13R, and P2Y14R), with P2Y11R activating both molecular pathways. accurate estimates. On cell stimulation, extracellular ATP levels increase to reach 10⫺4M40 (Figure 1). Although robust evidence shows that terminally differentiated erythroid, myeloid, and lymphoid cells release ATP, the precise pattern of eATP release in the BM microenvironment remains largely unknown: future studies measuring in situ eNTP concentrations in the BM are highly warranted. Progression: activation of purinergic signaling. eNTPs bind to nucleotide-selective receptors, collectively named P2Rs. Based on pharmacologic profile and on molecular structure, 2 subfamilies have been identified, P2XRs and P2YRs.45 P2XRs (composing 7 subtypes, P2X1R through P2X7R) are trimeric ATP-gated plasma membrane channels.46 P2YRs are classic G protein-coupled receptors that, based on their ligand selectivity, are further subdivided in subtypes preferentially responding to ATP, ADP, UTP, UDP, or sugar-linked nucleotides, such as UDP-glucose and UDPgalactose30 (Figure 2). Depending on tissue, engagement of P2XRs and P2YRs triggers a vast array of responses, ranging from cell proliferation or differentiation to necrotic cell death or apoptosis, from secretory exocytosis to chemotaxis, from reactive oxygen species generation to cytokine release. P2YRs respond to low nucleotide concentrations; thus, they are particularly suited to “sense” minute changes in nucleotide levels within the extracellular milieu and start chemotaxis. P2Y2R, P2Y6R, P2Y12R, and possibly P2Y13R appear to be the main subtypes involved in chemotaxis or inflammatory cell recruitment. Conversely, P2X7R seems to deliver a “stop signal” once cells have reached the core of inflammation.47 This is consistent with the different signals delivered by increasing ATP gradients: first, ATP activates high-affinity P2YRs and then the low-affinity P2X7R subtype, where ATP release and inflammation are higher. P2X7R plays an undisputed role in cytokine release. This receptor has emerged as a potent activator of the inflammasome and thus of IL-1 processing and release.48 Molecular details of this activity are however as yet obscure. The ability of eATP and P2X7R to promote inflammation has been established through several lines of in vivo evidence: of particular interest is their participation in GVHD. Like severe infections or traumas, GVHD leads to systemic inflammatory responses and causes tissue destruction and massive release of danger signals. In both humans and mice, ATP concentrations are increased during the development of GVHD, contributing to ignite a self-sustaining proinflammatory cascade involving IL-1␣, IFN-␥ production, donor T-cell expansion, and regulatory T-cell decrease.49 Resolution: down-regulation of purinergic signaling. In the extracellular environment, nucleotides are also a substrate for nucleotide- and nucleoside-converting ectoenzymes, which rapidly hydrolyze ATP to ADP, adenosine-monophosphate (AMP), and eventually adenosine. The activity of ectoenzymes makes eNTPs very labile in the blood (and in general in the extracellular environment): consequently, eNTPs are mainly viewed as “shortrange” mediators, although it is unlikely that they can act in an “hormone-like” fashion affecting responses of remote tissues and organs. Enzymes known to hydrolyze nucleotides include the ectonucleoside triphosphate diphosphohydrolase (E-NTPDase) family, the ecto-nucleotide pyrophosphatase/phosphodiesterase (E-NPP) family, the ecto-5⬘-nucleotidase, and alkaline phosphatases.40 NTPDase1/CD39 is one of the major nucleotide-hydrolyzing enzymes; and accordingly, CD39-null mice show clinical signs of exacerbated inflammatory responses, as seen in a model of skin inflammation secondary to chemical insults.50,51 The ecto-5⬘-nucleotidase CD73, which converts AMP into adenosine, is also critical in inflammation because of its anti-inflammatory/immunosuppressive activity. The anti-inflammatory role of CD73 is supported by in vivo experiments showing that CD73⫺/⫺ mice develop enhanced inflammation and an accelerated graft-versus-host reaction.52 Antiinflammatory effects of adenosine are mediated via a specific From www.bloodjournal.org by guest on June 16, 2017. For personal use only. BLOOD, 20 SEPTEMBER 2012 䡠 VOLUME 120, NUMBER 12 subfamily of purinergic receptors, named P1 receptors (ie, the A1, A2A, A2B, and A3 receptors.35 Interestingly, ATP is also a key modulator of immunosuppressive activity of T-regulatory lymphocytes. For a detailed description of ATP and adenosine function in immune cells, we refer readers to previously published reviews.53,54 Purinergic signaling in HPSCs Purinergic signaling in hematopoiesis has been mostly investigated in terminally differentiated cells55 and found to participate in several cell functions, including platelet aggregation,56 chemotaxis,31,50 cell death, and proinflammatory activity,57 as summarized in Table 1. Historically, the investigation of purinergic signaling in hematopoietic cells has focused on ATP, UTP, and derivatives. On the contrary, little information is currently available on other purines or pyrimidines, reflecting the limited activity that nucleotides, such as CTP, GTP, ITP, and TTP, have generally displayed.30 Despite the large body of data on purinergic signaling in immune effector cells, investigation of eNTP-mediated responses on HPSCs started only a few years ago. Here, we summarize the effects of eNTPs on HPSC proliferation, differentiation, and migration. Proliferation. In 2004, we found that P2Rs are expressed on CD34⫹ hematopoietic progenitors and that their engagement produced fast changes in the intracellular calcium homeostasis. ATP and UTP enhanced the stimulatory activity of several cytokines on clonogenic CD34⫹ cells. Similar effects were also observed in lineage-negative CD34⫺ progenitors, as well as in CD34⫹-derived long-term culture-initiating cells.58 Interestingly, stimulation with UTP increased the number of human BMrepopulating CD34⫹ cells after transplantation into immunodeficient mice.58 ATP-induced increase in the intracellular Ca2⫹ concentration also stimulated murine HSC proliferation and differentiation.59 More recently, eATP has been shown to reduce the number of HSCs as well as that of common myeloid progenitors and granulocyte myeloid progenitors, whereas mature BM myeloid cells were expanded. Interestingly, ATP-induced proliferation of HSCs resulted in a reduction in Notch expression, a marker of HSC quiescence.60 More recently, the link between ATP autocrine loops and HSC proliferation was investigated using the nucleotide-binding fluorescent probe quinacrine. ATP was found to actively accumulate within cytoplasmic vescicles in murine HPSCs.61 On stimulation of Ca2⫹-sensitive pathways, HPSCs can release these vesicles, igniting a positive autocrine loop that leads to P2Rs stimulation and further ATP release.61 Similarly to what previously observed,58 ATP positively affected cell-cycle dynamics in Lineage⫺c-Kit⫹Sca-1⫹ HPSCs in a cell-autonomous manner, with P2X1R and P2X4R subtypes most likely involved in the process.61 Finally, the role of endogenous ATP on HSCs becomes more prominent under inflammatory conditions. As assessed in 2 mouse models of T-cellmediated chronic inflammation, ATP positively contributed to the expansion of both Lineage⫺c-Kit⫹Sca-1⫹ cells and phenotypically defined HSCs via the activation of P2XRs.61 However, inflammatory conditions have been shown to modify the phenotype of HSCs, potentially leading to imprecise conclusions. In the future, it will be important to address how purinergic signaling affects HSC ability to repopulate the BM in the context of inflammation. The findings collected over the past decade suggest that purinergic signaling may promote the expansion of hematopoietic progenitors at the expense of more immature HSC subsets.60 Quiescence is fundamental for the long-term maintenance of hematopoiesis: a continuous stimulation of primitive HSCs with PURINERGIC SIGNALING AND INFLAMMATION IN HSCs 2369 high concentrations of danger signals, such as eNTPs, may drive HSCs out of quiescence and lead to a premature exhaustion of hematopoiesis. In the future, knockout mice lacking P2 receptors or endonucleotidases are expected to provide new clues on the effects of eNTPs on HSC quiescence and long-term hematopoiesis. If confirmed, such a scenario may help understand the detrimental effect that chronic inflammation might have on long-term hematopoiesis (Figure 3). Differentiation. Historically, investigations of purinergic signaling in hematopoiesis focused on lineage differentiation. Several reports contributed over the years to demonstrate the role of ATP in the differentiation of leukemia cell lines (HL-60 and NB4). Subsequently, new lines of evidence emerged supporting the widespread expression of P2Rs in hematopoietic cells. However, the pharmacologic profile of P2Rs sensibly differs among lineages and changes over time depending on the differentiation step. The differentiation of myeloid, erythroid, mekacaryocitic, and lymphoid progenitors has been shown to be influenced by eNTPs, although different receptors appear to be involved, depending on the specific lineage. For a detailed discussion on purinergic signaling in hematopoietic differentiation, we refer the reader to more comprehensive reviews on this topic.55,62 More recently, eNTPs have been found to have a tuning role on more immature myeloid progenitors. Barbosa et al showed that the in vivo administration of ATP depletes the number of granulocytemacrophage progenitors in mice while increasing the fraction of mature (Gr1⫹, Mac1⫹) myeloid cells.60 Prospectively, this activity could be a direct response of the hematopoietic system to generic alarm signals, such as those released during infections. Besides accelerating the production of a larger army of immune cells from primitive progenitors, eNTPs can also provide a molecular bridge between cell damage and immune responses: ATP and UTP can act as “find-me” signals when released by apoptotic cells, helping recruit phagocytes and allowing clearance of dying cells from tissues.63 Migration. Several reports suggested that molecules belonging to the circuit of innate immunity and regulating chemotaxis in immune cells may also play a role in enforcing HSC migration from the BM to peripheral tissues. Under physiologic conditions, HSCs are thought to primarily dwell in the BM, within the nurturing environment of the stem cell niche. The niche shields HSCs from external injury and helps maintain their survival, quiescence, and self-renewal. Nevertheless, HSCs have been found to circulate in the PB and other tissues as well. Although HSC peripheral traffic has been extensively characterized in clinical settings, their ability to egress the BM, circulate in peripheral tissues, and eventually home back to the BM under physiologic conditions is yet to be fully characterized. At any given time, between 100 and 400 HSCs are found circulating in the mouse PB64: some of these reenter the BM, in a continuous exchange between the 2 compartments.65 It has been suggested that circulating HSCs are actually patrolling peripheral tissues, looking for potential injuries and infections.66 Lipopolysaccharide and other bacterial products have also been shown to easily reach the BM environment, where they stimulate TLR-expressing HSCs to produce more immune effectors. Nonetheless, migrating HSCs have an advantage over BM-resident HSCs: they may act as scouts in the peripheral tissues and sense the presence of pathogens directly at infection sites, possibly promoting a rapid and localized production of immune cells. For instance, complement cleavagefragments released during immune responses have been shown to take part in HSC migration: C5 cleavage-fragments drive HSC From www.bloodjournal.org by guest on June 16, 2017. For personal use only. 2370 BLOOD, 20 SEPTEMBER 2012 䡠 VOLUME 120, NUMBER 12 ROSSI et al Table 1. Expression and function of P1 and P2 receptor subtypes in normal human hematopoietic cells Cell type CD34⫹ cells Receptor subtype P2X1, P2X2, P2X3, P2X4, P2X5, P2X6, P2X7 Responses/functions References In vivo and in vitro proliferation, chemotaxis, cell adhesion* 58,83 IL-12 inhibition 84 P2Y1, P2Y2, P2Y11, P2Y12, P2Y13 DCs A1 A2A 84,85 A3 86,87 Chemotaxis* 87 Chemotaxis 88 P2Y4 CXCL8 88 P2Y6 IL-8, maturation of moncytes derived DCs, chemotaxis 88,89 IL-1 secretion 88 Chemotaxis 92 P2Y1 P2Y2 31,88 P2Y11 P2X1, P2X4 88,90 P2X7 88,91 Plasmacytoid DCs A1 A2A Down-regulation IL-6, IL-12, IFN-␣ 92 Eosinophils A3 Apoptosis 93 P2X1, P2X4, P2X7 Chemotaxis 94 P2Y1 94 P2Y2 31,94 P2Y4, P2Y6, P2Y11 94 CD11 up-regulation, ROIs, IL-8 and ECP secretion* 94,95 P2X7 Shedding of L-selectin and CD23 83,96 TCD4⫹ lymphocytes A2A Inhibition of proliferation 97 TCD8⫹ lymphocytes A2A Inhibition of cytotoxicity 97 T lymphocytes A1 Anergy, induction of Treg 99 B lymphocytes P2X1, P2X2, P2X4 A2A 83,96 98 A2B 100 A3 87 P2X1, P2X4, P2X7 83 P2Y1, P2Y2, P2Y4, P2Y6, P2Y11, P2Y12, P2Y13 Macrophages 83 A1 Enhancement of Fc␥ receptor-mediated phagocytosis 101 A2A IL-4-induced TIMP-1 secretory, inhibitory IL-12, NO, MIP-1␣, TNF-␣ 102 decrease of Fc␥ receptor-mediated phagocytosis A2B IL-4-induced TIMP-1 secretory, inhibitory IL-12, NO, MIP-1␣, TNF-␣ 102 Polycarion formation, IL-1 secretion 103 P2Y2 Enhancement of ROI production 104,105 A1 Activation of mast cell degranulation 106 A2A Potentiation of Fc⑀RI-induced degranulation 107 A2B Inhibition of mast cell degranulation 106 A3 P2X1, P2X4, P2X7 102 P2Y1, P2Y4, P2Y6 Mast cells 104 P2X1, P2X4 108 P2Y1, P2Y2, P2Y11, P2Y12, P2Y13 Monocytes 108 A2A Inhibition of TNF-␣, IL-6, IL-8, IL-12 102 Stimulation of IL-10 secretion 102 A3 Inhibition ROIs production 109 P2X1, P2X4, P2X7 83,110 P2Y1, P2Y2, P2Y4, P2Y6, P2Y11, P2Y12, P2Y13 Neutrophils A1 83,104 Increase of chemotaxis Increase of Fc␥R-mediated phagocytosis and ROI production 101 Inhibition of Fc␥R-mediated phagocytosis and ROI production 101 Inhibition of cell adhesion 102 A3 Degranulation and ROI production inhibition, chemotaxis 111 P2X1 Chemotaxis 112 Chemotaxis 111 Inhibition of cytotoxicity 97 A2A A2B 100 P2X7 P2Y2 110 P2Y4, P2Y6, P2Y11 NK cells 102 A2A 103,111 P2X1, P2X4, P2X5, P2X6, P2X7 110,113 P2Y1, P2Y2, P2Y4, P2Y6, , P2Y12, P2Y13, P2Y14 P2Y11 113 Inhibition of CX3CL1-elicited NK-mediated killing ROI indicates reactive oxygen intermediate; ECP, eosinophil cationic protein; and TIMP-1, tissue inhibitor of matrix metalloproteinase-1. *Responses/functions that have been documented in a cell type but not linked to a specific receptor subtype. 113 From www.bloodjournal.org by guest on June 16, 2017. For personal use only. BLOOD, 20 SEPTEMBER 2012 䡠 VOLUME 120, NUMBER 12 PURINERGIC SIGNALING AND INFLAMMATION IN HSCs 2371 Table 1. Expression and function of P1 and P2 receptor subtypes in normal human hematopoietic cells (continued) Cell type Platelets Receptor subtype Responses/functions References A2A Antiaggregation 114 P2Y1 Aggregation and shape changes 114 P2Y12 Aggregation, phosphatidylserine exposure 115 P2X1 Transient shape changes 109 Phosphatidylserine exposure 116 P2X7 Red blood cells P2X2 P2X7 P2Y1 116 ROI indicates reactive oxygen intermediate; ECP, eosinophil cationic protein; and TIMP-1, tissue inhibitor of matrix metalloproteinase-1. *Responses/functions that have been documented in a cell type but not linked to a specific receptor subtype. mobilization, whereas C3 cleavage-products promote HSC retention in the BM. This finding has also been confirmed in animal models, with C5-deficient mice acting as poor mobilizers and C3-deficient mice mobilizing HSCs more efficiently.67 Such a scenario help envision HSC mobilization as an integral part of innate immunity.68 Recently, eNTPs have been shown to modulate HSC migration in the presence of CXC-chemokine 12 (CXCL12), considered the most important chemotactic factor for HSCs and responsible of stem cell retention in the BM niche. eUTP improves human HSC migration toward CXCL12 gradients and inhibits the downregulation of membrane CXCR4 (CXCL12 receptor) in migrating CD34⫹ cells.69 Similarly, pretreatment with eUTP significantly increases BM homing of CD34⫹ HSCs when transplanted into immunodeficient mice.69 Of note, purinergic signaling can affect HPSCs also indirectly, by acting on the HSC niche. BM-derived mesenchymal stromal cells (BM-MSCs) represent a key component of the hematopoietic niche and secrete several HSC regulatory molecules, such as CXCL12 and stem cell factor. Recent findings Figure 3. Purinergic signaling in BM-derived HPSCs, leukemic cells, and BM-derived MSCs. Recent findings suggest that purinergic signaling may affect HSCs at 2 different levels: by directly binding P2Rs on HPSCs or by targeting cells that are part of the HSC niche (such as MSCs). This figure summarizes how eNTPs directly modulate proliferation, migration, and engraftment in HPSCs and leukemic stem cells. BM-derived MSCs are also a target for eNTPs: activation of purinergic signaling in these cells has been shown to enhance their adipogenic/osteogenic differentiation, as well as the release of proinflammatory cytokines. showed that ATP treatment is associated with an increase in the production of proinflammatory cytokines in BM-MSCs (such as IL-2, IFN-␥, and IL-12p70), and the expression of purinergic receptors is modulated during adipogenic and osteogenic differentiation.70,71 Purinergic signaling in malignant hematopoiesis It is becoming increasingly evident that tumor onset and progression depend not only on properties intrinsic to cancer cells. Both the biochemical composition of the tumor microenvironment and the cancer-host interaction appear to be important in disease evolution. eNTPs may now acquire a new biologic significance as part of the complex molecular miscellany composing the tumor environment. Over the past decade, several in vitro studies described ATP’s capability of suppressing cell growth in several cancer cell lines, From www.bloodjournal.org by guest on June 16, 2017. For personal use only. 2372 ROSSI et al including human HL-60 acute promyelocytic leukemia cells.72 In line with these findings, our group recently investigated the role of purinergic signaling in the tumor microenvironment associated with acute myeloid leukemia (AML). We found that AML cells express several functional P2XRs and P2YRs. Very interestingly, and conversely to HSCs from healthy donors,58 ATP inhibits cell proliferation and colony formation in AML cells, by restraining AML cells in G0, and reduces AML cell engraftment in immunodeficient mice.73 Among P2Rs, P2X7R appears to be a major mediator of ATP-dependent inhibition of cell growth in AML cells. As previously reported in chronic lymphocytic leukemia,74 also in AML P2X7 expression is higher, with highest levels in patients with a decreased remission rate. Remarkably, the highest P2X7R levels were detected in patients undergoing relapse, suggesting a role for this receptor in AML progression.75 P2X7R is also overexpressed in adult AML cells where its tonic stimulation promotes cell proliferation. Other P2XRs, such as P2X1R, P2X4R, and P2X5R are abnormally expressed in AML cells, suggesting a wide dysregulation and a possible pathogenic role of purinergic signaling in hematologic malignancies.76 On the contrary, ATP exerts an antiproliferative activity on leukemic blasts by down-modulating P2X7R expression.73 Based on this findings, eNTPs emerge as key components of the leukemic microenvironment where they appear to modulate proliferation and differentiation (Figure 3). In addition, eNTPs affect the motility of cells derived from AML patients.73 In migration assays, ATP inhibited the spontaneous migration of AML cells in vitro, whereas UTP also reduced CXCL12-driven migration. P2Y2R and P2Y4R receptors appeared to be the subtypes mainly involved in the process. Interestingly, AML BM homing and long-term engraftment are also decreased on exposure to eNTPs. Remarkably, ATP and UTP, as well as P2YR-agonists, significantly inhibited the long-term engraftment of highly purified CD38⫺CD34⫹ leukemic stem cells,73 suggesting that purinergic signaling can also affect rare leukemic stem cells, which usually escape most therapeutic approaches, making AML difficult to eradicate (Figure 3). Translational implications and future perspectives Translational studies on nucleotides are a rapidly expanding field that has prompted experimental therapeutic strategies against chronic inflammation and autoimmune diseases. In hematology, blocking purinergic signaling is now regarded as a promising pharmacologic approach for reducing the detrimental effects of GVHD without compromising graft-versus-leukemia responses.77 Purinergic signaling could be targeted at different levels: (1) by counteracting ATP release in response to chemical or infective insults; (2) by preventing the activation of P2Rs signaling cascades, such as the P2X7R-NALP3-inflammasome pathway; and (3) by enhancing ATP hydrolysis by ecto-enzymes (CD39 or CD73), promoting a quicker resolution of inflammation. On the contrary, therapies enhancing purinergic signaling in the tumor microenvironment may prove useful in firing immunity against cancer cells.78 In addition, regulation of cell proliferation by nucleotides presents sensible differences between leukemic stem cells and HSCs: inhibition of AML proliferation and engraftment highlights novel routes of investigations for treating hematopoietic tumors while sparing healthy HSCs. BLOOD, 20 SEPTEMBER 2012 䡠 VOLUME 120, NUMBER 12 Deciphering what role purinergic signaling plays in vivo will also be critical for the mechanistic integration of eNTP effects on HSCs and the environment in which they reside. Because of the widespread expression of P2Rs, the biologic outcome of their stimulation will probably reflect the concerted activity on different cell subsets, including hematopoietic and nonhematopoietic cells. New insights are also expected to arise from the role of purinergic signaling in bone physiology. Osteoblast cells play a pivotal role in the BM niche and osteoblast defects have previously been associated with impaired maintenance of HSCs. Interestingly, osteoblasts and osteoclasts are important sources of extracellular ATP, potentially affecting HPSC responses in the niche. In addition, several investigators reported bone deficiency in knockout mice lacking specific P2Rs. P2Y1R⫺/⫺, P2Y2R⫺/⫺, P2Y6R⫺/⫺, and P2Y13R⫺/⫺ mice present bone abnormalities, and P2X7R⫺/⫺ mice display a striking reduction in bone formation and remodeling,79 suggesting a role in balancing osteoclasts and osteoblast activity.80 Recently, studies in A2B knockout mice also highlighted a reduction in osteoblast differentiation, hinting at a role for adenosine in bone formation and resorption. Similar conclusions were drawn from the analysis of mice lacking CD73, suggesting that the disruption of adenosine signaling is highly detrimental to osteoblasts. Interestingly, CD73 blocking has been shown to significantly reduce tumor growth and metastasis.81 Of note, both BM-MSCs (from which osteoblasts are derived) and HPSCs (which give rise, among other lineages, to osteoclasts) express both CD39 and CD73,60 suggesting that new insights could arise from the pharmacologic targeting of endonucleosidases. If confirmed, purinergic signaling may emerge as a regulator of HSC-stromal cell interactions within the osteoblastic stem cell niche, and future studies may help elucidate the role of P2Rs in both steady-state and stressed hematopoiesis. In conclusion, over the past 2 decades, a new picture of defense mechanisms in vertebrates has emerged. Not just specialized immune cells, but nonimmune cells as well may be involved, adding versatility and resilience to the whole system. Strikingly, some of these cells are primitive progenitors and stem cells, suggesting that immune effectors only represent the visible tip of a complex defense mechanism that deepens its roots into the stem cell compartment. In this view, the hematopoietic system no longer appears as a hierarchical model where the different compartments are hermetically organized. Instead, hematopoiesis is a dynamic system that reacts as a whole, where cells, either terminally differentiated or HSCs, speak a common language and react synergistically to protect the organism from danger and reestablish homeostasis (Figure 4). Several insults can subvert homeostatic conditions. Ionizing radiations, infections, chemical insults, and chemotherapeutic drugs all contribute to the release of nucleotides into the extracellular milieu. In the hematopoietic system, eNTPs can act at different levels: (1) by stimulating HPSC proliferation and differentiation, eNTPs and other alarmins contribute to immune cell production, invigorating defense mechanisms; and (2) circulating HSCs may sense danger signals coming from injured or inflamed tissues and migrate where immune effectors are needed the most, providing an in loco supply of granulocytes or antigen-presenting cells. Future insights may arise from other cell types participating to the healing of injured areas by responding to purinergic signaling, such as endothelial progenitor cells: in these cells, ATP has been shown to negatively affect proliferation and inhibit TLR4 expression, decreasing the release of proinflammatory cytokines.82 From www.bloodjournal.org by guest on June 16, 2017. For personal use only. BLOOD, 20 SEPTEMBER 2012 䡠 VOLUME 120, NUMBER 12 PURINERGIC SIGNALING AND INFLAMMATION IN HSCs 2373 Figure 4. Extracellular nucleotides: pleiotropic players in the maintenance of homeostasis. A prospective overview of the role played by eNTPs in modulating responses to danger and how purinergic pathway integrates with immunomodulatory responses. Several insults can contribute to subvert the homeostatic condition in the hematopoietic system. Infective agents, ionizing radiations, chemical insults, and mechanical stress contribute to the release of nucleotides into the extracellular environment and the engagement of P2Rs on target cells (HSCs, regulatory T cells, MSCs, and endothelial progenitor cells), where eNTPs can cooperate in containing damage at different levels: (1) stimulate HSC proliferation and the subsequent production of immune effectors that will invigorate defense mechanisms; (2) attract HSCs, in synergy with other chemokines (eg, CXCL12), toward sites of inflammation and infection to activate tissue repair; and (3) contain detrimental effects of prolonged inflammation and immune responses acting on mature immune cells (eg, regulatory T cells). The net result of such a widespread effect on the hematopoietic system is aimed at damage containment and return to homeostatic conditions. EPC indicates endothelial progenitor cells. The authors apologize to those authors whose work could not be referenced or discussed because of space limitations. Acknowledgments The authors thank Margaret A. Goodell for her valuable comments and suggestions. This research was supported by the Italian Ministry for University Education and Research (PRIN 2008), Cassa di Risparmio di Bologna (project on Leukemic Stem Cells), the Italian Association for Cancer Research (IG 5354), Telethon of Italy (GGP11014), the Regione Emilia Romagna (Research Programs “Innovative approaches to the diagnosis of inflammatory diseases” and “Moniter”), and the University of Ferrara (institutional funds). L.R. was also supported by the Italian Leukemia and Lymphoma Association, section of Bologna (BolognaAIL). Authorship Contribution: L.R., V.S., D.F., F.D.V., and R.M.L. designed and wrote the manuscript. Conflict-of-interest disclosure: The authors declare no competing financial interests. Correspondence: Lara Rossi, Department of Hematology and Oncological Sciences, L. and A. Seràgnoli, Institute of Hematology, University of Bologna, Orsola-Malpighi Hospital, via Massarenti, 9, I-40138 Bologna, Italy; e-mail: [email protected] References 1. Baldridge MT, King KY, Goodell MA. Inflammatory signals regulate hematopoietic stem cells. Trends Immunol. 2011;32(2):57-65. 2. Boiko JR, Borghesi L. Hematopoiesis sculpted by pathogens: toll-like receptors and inflammatory mediators directly activate stem cells. Cytokine. 2012;57(1):1-8. 3. Lazarowski ER, Boucher RC. UTP as an extracellular signaling molecule. News Physiol Sci. 2001; 16:1-5. 4. Tanaka K, Gilroy S, Jones AM, Stacey G. Extracellular ATP signaling in plants. Trends Cell Biol. 2010;20(10):601-608. 5. Esther CR Jr, Dohlman HG, Ault AD, et al. Similarities between UDP-glucose and adenine nucleotide release in yeast: involvement of the secretory pathway. Biochemistry. 2008;47(35):92699278. 6. Burnstock G. Purine and pyrimidine receptors. Cell Mol Life Sci. 2007;64(12):1471-1483. 7. Burnstock G. Pathophysiology and therapeutic potential of purinergic signaling. Pharmacol Rev. 2006;58(1):58-86. 8. Bours MJL, Swennen ELR, Di Virgilio F, Cronstein BN, Dagnelie PC. Adenosine 5⬘triphosphate and adenosine as endogenous signaling molecules in immunity and inflammation. Pharmacol Ther. 2006;112(2):358-404. 9. Trumpp A, Essers M, Wilson A. Awakening dormant haematopoietic stem cells. Nat Rev Immunol. 2010;10(3):201-209. 10. Cheshier SH, Prohaska SS, Weissman IL. The effect of bleeding on hematopoietic stem cell cycling and self-renewal. Stem Cells Dev. 2007; 16(5):707-717. chronic infection. Nature. 2010;465(7299):793797. 13. Sato T, Onai N, Yoshihara H, et al. Interferon regulatory factor-2 protects quiescent hematopoietic stem cells from type I interferon-dependent exhaustion. Nat Med. 2009;15(6):696-700. 14. Essers MG, Offner S, Blanco-Bose WE, et al. IFNalpha activates dormant haematopoietic stem cells in vivo. Nature. 2009;458(7240):904-908. 15. Zhao X, Ren G, Liang L, et al. Brief report: interferon-gamma induces expansion of Lin(⫺)Sca-1(⫹)c-Kit(⫹) cells. Stem Cells. 2010; 28(1):122-126. 11. Harrison D, Lerner C. Most primitive hematopoietic stem cells are stimulated to cycle rapidly after treatment. Blood. 1991;78(5):1237-1240. 16. Kitagawa M, Saito I, Kuwata T, et al. Overexpression of tumor necrosis factor (TNF)-alpha and interferon (IFN)-gamma by bone marrow cells from patients with myelodysplastic syndromes. Leukemia. 1997;11(12):2049-2054. 12. Baldridge MT, King KY, Boles NC, Weksberg DC, Goodell MA. Quiescent haematopoietic stem cells are activated by IFN-gamma in response to 17. Zhang Y, Harada A, Bluethmann H, et al. Tumor necrosis factor (TNF) is a physiologic regulator of hematopoietic progenitor cells: increase of early From www.bloodjournal.org by guest on June 16, 2017. For personal use only. 2374 ROSSI et al hematopoietic progenitor cells in TNF receptor p55-deficient mice in vivo and potent inhibition of progenitor cell proliferation by TNF alpha in vitro. Blood. 1995;86(8):2930-2937. 18. Rebel VI, Hartnett S, Hill GR, et al. Essential role for the p55 tumor necrosis factor receptor in regulating hematopoiesis at a stem cell level. J Exp Med. 1999;190(10):1493-1504. 19. Matzinger P. The danger model: a renewed sense of self. Science. 2002;296(5566):301-305. 20. Hansen JD, Vojtech LN, Laing KJ. Sensing disease and danger: a survey of vertebrate PRRs and their origins. Dev Comp Immunol. 2011; 35(9):886-897. 21. Bianchi ME. DAMPs, PAMPs and alarmins: all we need to know about danger. J Leukoc Biol. 2007; 81(1):1-5. 22. Oppenheim JJ, Yang D. Alarmins: chemotactic activators of immune responses. Curr Opin Immunol. 2005;17(4):359-365. 23. Nardini E, Morelli D, Aiello P, et al. CpGoligodeoxynucleotides induce mobilization of hematopoietic progenitor cells into peripheral blood in association with mouse KC (IL-8) production. J Cell Physiol. 2005;204(3):889-895. 24. Nagai Y, Garrett KP, Ohta S, et al. Toll-like receptors on hematopoietic progenitor cells stimulate innate immune system replenishment. Immunity. 2006;24(6):801-812. 25. Esplin BL, Shimazu T, Welner RS, et al. Chronic exposure to a TLR ligand injures hematopoietic stem cells. J Immunol. 2011;186(9):5367-5375. 26. Chen C, Liu Y, Liu Y, Zheng P. Mammalian target of rapamycin activation underlies HSC defects in autoimmune disease and inflammation in mice. Bone. 2010;120(11):4091-4101. BLOOD, 20 SEPTEMBER 2012 䡠 VOLUME 120, NUMBER 12 38. Fredholm BB. Adenosine, an endogenous distress signal, modulates tissue damage and repair. Cell Death Differ. 2007;14(7):1315-1323. 39. Lazarowski ER, Boucher RC, Harden TK. Constitutive release of ATP and evidence for major contribution of ecto-nucleotide pyrophosphatase and nucleoside diphosphokinase to extracellular nucleotide concentrations. J Biol Chem. 2000; 275(40):31061-31068. 40. Yegutkin GG. Nucleotide- and nucleosideconverting ectoenzymes: important modulators of purinergic signalling cascade. Biochim Biophys Acta. 2008;1783(5):673-694. 41. Burnstock G. Purinergic signalling: its unpopular beginning, its acceptance and its exciting future. Bioessays. 2012;218-225. 42. Joseph SM, Buchakjian MR, Dubyak GR. Colocalization of ATP release sites and ecto-ATPase activity at the extracellular surface of human astrocytes. J Biol Chem. 2003;278(26):2333123342. 59. Paredes-Gamero EJ, Leon CMMP, Borojevic R, Oshiro MEM, Ferreira AT. Changes in intracellular Ca2⫹ levels induced by cytokines and P2 agonists differentially modulate proliferation or commitment with macrophage differentiation in murine hematopoietic cells. J Biol Chem. 2008; 283(46):31909-31919. 60. Barbosa CMV, Leon CMMP, Nogueira-Pedro A, et al. Differentiation of hematopoietic stem cell and myeloid populations by ATP is modulated by cytokines. Cell Death Dis. 2011;2:e165. 61. Casati A, Frascoli M, Traggiai E, et al. Cellautonomous regulation of hematopoietic stem cell cycling activity by ATP. Cell Death Differ. 2011;18(3):396-404. 62. Sak K, Boeynaems JM, Everaus H. Involvement of P2Y receptors in the differentiation of haematopoietic cells. J Leukoc Biol. 2003;73:442-447. 43. Pellegatti P, Raffaghello L, Bianchi G, et al. Increased level of extracellular ATP at tumor sites: in vivo imaging with plasma membrane luciferase. PloS One. 2008;3(7):e2599. 63. Elliott MR, Chekeni FB, Trampont PC, et al. Nucleotides released by apoptotic cells act as a findme signal to promote phagocytic clearance. Nature. 2009;461(7261):282-286. 44. Lazarowski ER, Homolya L, Boucher RC, Harden TK. Direct demonstration of mechanically induced release of cellular UTP and its implication for uridine nucleotide receptor activation. J Biol Chem. 1997;272(39):24348-24354. 64. Morrison SJ, Wright DE, Weissman IL. Cyclophosphamide/granulocyte colony-stimulating factor induces hematopoietic stem cells to proliferate prior to mobilization. Proc Natl Acad Sci U S A. 1997;94(5):1908-1913. 45. Ralevic V, Burnstock G. Receptors for purines and pyrimidines. Pharmacol Rev. 1998;50(3): 413-492. 65. Wright DE, Wagers AJ, Gulati AP, Johnson FL, Weissman IL. Physiological migration of hematopoietic stem and progenitor cells. Science. 2001; 294(5548):1933-1936. 46. Khakh BS, North RA. P2X receptors as cellsurface ATP sensors in health and disease. Nature. 2006;442(7102):527-532. 27. Chen C, Liu Y, Liu Y, Zheng P. mTOR regulation and therapeutic rejuvenation of aging hematopoietic stem cells. Sci Signal. 2009;2(98):ra75. 47. Wiley JS, Sluyter R, Gu BJ, Stokes L, Fuller SJ. The human P2X7 receptor and its role in innate immunity. Tissue Antigens. 2011;78(5):321-332. 28. Takizawa H, Regoes RR, Boddupalli CS, Bonhoeffer S, Manz MG. Dynamic variation in cycling of hematopoietic stem cells in steady state and inflammation. J Exp Med. 2011;208(2): 273-284. 48. Piccini A, Carta S, Tassi S, et al. ATP is released by monocytes stimulated with pathogen-sensing receptor ligands and induces IL-1beta and IL-18 secretion in an autocrine way. Proc Natl Acad Sci U S A. 2008;105(23):8067-8072. 29. Lazarowski ER. Vesicular and conductive mechanisms of nucleotide release. Purinergic Signal. 2012;359-373. 49. Wilhelm K, Ganesan J, Müller T, et al. Graftversus-host disease is enhanced by extracellular ATP activating P2X7R. Nat Med. 2010;16(12): 1434-1438. 30. Abbracchio MP, Burnstock G, Boeynaems JM, et al. International union of pharmacology LVIII: update on the P2Y G protein-coupled nucleotide receptors: from molecular mechanisms and pathophysiology. Pharmacol Rev. 2006;58(3): 281-341. nucleotides are potent stimulators of human hematopoietic stem cells in vitro and in vivo. Blood. 2004;104(6):1662-1670. 50. Hyman MC, Petrovic-Djergovic D, Visovatti SH, et al. Self-regulation of inflammatory cell trafficking in mice by the leukocyte surface apyrase CD39. J Clin Invest. 2009;119(5):1136. 66. Massberg S, Schaerli P, Knezevic-Maramica I, et al. Immunosurveillance by hematopoietic progenitor cells trafficking through blood, lymph, and peripheral tissues. Cell. 2007;131(5):994-1008. 67. Reca R, Cramer D, Yan J, et al. A novel role of complement in mobilization: immunodeficient mice are poor granulocyte-colony stimulating factor mobilizers because they lack complementactivating immunoglobulins. Stem Cells. 2007; 25(12):3093-3100. 68. Lee H, Ratajczak MZ. Innate immunity: a key player in the mobilization of hematopoietic stem/ progenitor cells. Arch Immunol Ther Exp. 2009; 57(4):269-278. 69. Rossi L, Manfredini R, Bertolini F, et al. The extracellular nucleotide UTP is a potent inducer of hematopoietic stem cell migration. Blood. 2007; 109(2):533-542. 31. Müller T, Robaye B, Vieira R, et al. The purinergic receptor P2Y2 receptor mediates chemotaxis of dendritic cells and eosinophils in allergic lung inflammation. Allergy. 2010;65(12):1545-1553. 51. Mizumoto N, Kumamoto T, Robson SC, et al. CD39 is the dominant Langerhans cellassociated ecto-NTPDase: modulatory roles in inflammation and immune responsiveness. Nat Med. 2002;8(4):358-365. 70. Ferrari D, Gulinelli S, Salvestrini V, et al. Purinergic stimulation of human mesenchymal stem cells potentiates their chemotactic response to CXCL12 and increases the homing capacity and production of proinflammatory cytokines. Exp Hematol. 2011;39(3):360-374. 32. Lee B, Cheng T, Adams GB, et al. P2Y-like receptor, GPR105 (P2Y14) identifies and mediates chemotaxis of bone-marrow hematopoietic stem cells. Genes Dev. 2003;105:1592-1604. 52. Zernecke A, Bidzhekov K, Ozüyaman B, et al. CD73/ecto-5⬘-nucleotidase protects against vascular inflammation and neointima formation. Circulation. 2006;113(17):2120-2127. 71. Zippel N, Limbach CA, Ratajski N, et al. Purinergic receptors influence the differentiation of human mesenchymal stem cells. Stem Cells Dev. 2012;21(6):884-900. 33. Burnstock G, Verkhratsky A. Long-term (trophic) purinergic signalling: purinoceptors control cell proliferation, differentiation and death. Cell Death Dis. 2010;1(1):e9. 53. Bours MJL, Dagnelie PC, Giuliani AL, Wesselius A, Di Virgilio F. P2 receptors and extracellular ATP: a novel homeostatic pathway in inflammation. Front Biosci (Schol Ed). 2011;3:1443-1456. 34. Di Virgilio F, Boeynaems J-M, Robson SC. Extracellular nucleotides as negative modulators of immunity. Curr Opinion Pharmacol. 2009;9(4): 507-513. 54. Trautmann A. Extracellular ATP in the immune system: more than just a “danger signal.” Sci Signal. 2009;2(56):19193605. 72. Conigrave AD, van der Weyden L, Holt L, et al. Extracellular ATP-dependent suppression of proliferation and induction of differentiation of human HL-60 leukemia cells by distinct mechanisms. Biochem Pharmacol. 2000;60(11):1585-1591. 35. Blackburn M, Vance C, Morschl E, Wilson C. Adenosine receptors and inflammation. Handb Exp Pharmacol. 2009;193:215-269. 36. Suadicani SO, Brosnan CF, Scemes E. P2X7 receptors mediate ATP release and amplification of astrocytic intercellular Ca2⫹ signaling. J Neurosci. 2006;26(5):1378-1385. 37. Brandao-Burch A, Key ML, Patel JJ, Arnett TR, Orriss IR. The P2X7 receptor is an important regulator of extracellular ATP levels. Front Endocrinol. 2012;3:41. 55. Di Virgilio F. Nucleotide receptors: an emerging family of regulatory molecules in blood cells. Blood. 2001;97(3):587-600. 56. Cattaneo M, Lecchi A, Ohno M, et al. Antiaggregatory activity in human platelets of potent antagonists of the P2Y 1 receptor. Biochem Pharmacol. 2004;68(10):1995-2002. 57. Pizzirani C, Ferrari D, Chiozzi P, et al. Stimulation of P2 receptors causes release of IL-1betaloaded microvesicles from human dendritic cells. Blood. 2007;109(9):3856-3864. 58. Lemoli RM, Ferrari D, Fogli M, et al. Extracellular 73. Salvestrini V, Zini R, Rossi L, et al. Purinergic signaling inhibits human acute myeloblastic leukemia cell proliferation, migration and engraftment in immunodeficient mice. Blood. 2012;119(1): 217-226. 74. Adinolfi E. P2X7 receptor expression in evolutive and indolent forms of chronic B lymphocytic leukemia. Blood. 2002;99(2):706-708. 75. Zhang X-J, Zheng G-G, Ma X-T, et al. Expression of P2X7 in human hematopoietic cell lines and leukemia patients. Leuk Res. 2004;28(12):13131322. 76. Chong J-H, Zheng G-G, Zhu X-F, et al. Abnormal expression of P2X family receptors in Chinese From www.bloodjournal.org by guest on June 16, 2017. For personal use only. BLOOD, 20 SEPTEMBER 2012 䡠 VOLUME 120, NUMBER 12 pediatric acute leukemias. Biochem Biophys Res Commun. 2010;391(1):498-504. 77. Zeiser R, Penack O, Holler E, Idzko M. Danger signals activating innate immunity in graft-versushost disease. J Mol Med. 2011;89(9):833-845. PURINERGIC SIGNALING AND INFLAMMATION IN HSCs 91. Ferrari D, La Sala A, Chiozzi P, et al. The P2 purinergic receptors of human dendritic cells: identification and coupling to cytokine release. FASEB J. 2000;14(15):2466-2476. 2375 Virgilio F. P2X(7) receptor and polykarion formation. Mol Biol Cell. 2000;11(9):3169-3176. 104. Jin J, Dasari VR, Sistare FD, Kunapuli SP. Distribution of P2Y receptor subtypes on haematopoietic cells. Br J Pharmacol. 1998;123(5):789-794. 78. Stagg J, Smyth MJ. Extracellular adenosine triphosphate and adenosine in cancer. Oncogene. 2010;29(39):5346-5358. 92. Schnurr M, Toy T, Shin A, et al. Role of adenosine receptors in regulating chemotaxis and cytokine production of plasmacytoid dendritic cells. Blood. 2004;103(4):1391-1397. 79. Ke HZ, Qi H, Weidema AF, et al. Deletion of the P2X7 nucleotide receptor reveals its regulatory roles in bone formation and resorption. Mol Endocrinol. 2003;17(7):1356-1367. 93. Kohno Y, Ji X, Mawhorter SD, Koshiba M, Jacobson KA. Activation of A3 adenosine receptors on human eosinophils elevates intracellular calcium. Blood. 1996;88(9):3569-3574. 105. Schmid-Antomarchi H, Schmid-Alliana A, Romey G, et al. Extracellular ATP and UTP control the generation of reactive oxygen intermediates in human macrophages through the opening of a charybdotoxin-sensitive Ca2⫹-dependent K⫹ channel. J Immunol. 1997;159(12):62096215. 80. Orriss IR, Wang N, Burnstock G, et al. The P2Y(6) receptor stimulates bone resorption by osteoclasts. Endocrinology. 2011;152(10):37063716. 94. Ferrari D, Idzko M, Dichmann S, et al. P2 purinergic receptors of human eosinophils: characterization and coupling to oxygen radical production. FEBS Lett. 2000;486(3):217-224. 106. Yip KH, Lau HYA, Wise H. Reciprocal modulation of anti-IgE induced histamine release from human mast cells by A1 and A(2b) adenosine receptors. Br J Pharmacol. 2011;164(2b):807-819. 95. Dichmann S, Idzko M, Zimpfer U, et al. Adenosine triphosphate-induced oxygen radical production and CD11b up-regulation: Ca mobilization and actin reorganization in human eosinophils adenosine triphosphate-induced oxygen radical production and CD11b up-regulation. Blood. 2000;95(3):973-978. 107. Gomez G, Zhao W, Schwartz LB. Disparity in Fc⑀RI-induced degranulation of primary human lung and skin mast cells exposed to adenosine. J Clin Immunol. 2011;31(3):479-487. 81. Stagg J, Divisekera U, Duret H, et al. CD73deficient mice have increased antitumor immunity and are resistant to experimental metastasis. Cancer Res. 2011;71(8):2892-2900. 82. Xiao Z, Yang M, Li F, Lv Q, He Q. Extracellular nucleotide inhibits cell proliferation and negatively regulates toll-like receptor 4 signaling in human progenitor endothelial cells. Cell Biol Int. 2012; 36(7):625-633. 83. Wang L, Jacobsen SEW, Bengtsson A, Erlinge D. P2 receptor mRNA expression profiles in human lymphocytes, monocytes and CD34⫹ stem and progenitor cells. BMC Immunol. 2004;5:16. 84. Gessi S, Varani K, Merighi S, et al. Expression of A3 adenosine receptors in human lymphocytes: up-regulation in T cell activation. Mol Pharmacol. 2004;65(3):711-719. 85. Haskó G, Cronstein B. Adenosine: an endogenous regulator of innate immunity. Trends Immunol. 2004;25(1):33-39. 86. Panther E, Corinti S, Idzko M, et al. Adenosine affects expression of membrane molecules, cytokine and chemokine release, and the T-cell stimulatory capacity of human dendritic cells. Blood. 2003;101(10):3985-3990. 87. Panther E, Idzko M, Herouy Y, et al. Expression and function of adenosine receptors in human dendritic cells. FASEB J. 2001;15(11):1963-1970. 96. Gu B, Bendall LJ, Wiley JS. Adenosine triphosphate-induced shedding of CD23 and L-selectin (CD62L) from lymphocytes is mediated by the same receptor but different metalloproteases. Blood. 1998;92(3):946-951. 97. Häusler SFM, Montalbán del Barrio I, Strohschein J, et al. Ectonucleotidases CD39 and CD73 on OvCA cells are potent adenosinegenerating enzymes responsible for adenosine receptor 2A-dependent suppression of T cell function and NK cell cytotoxicity. Cancer Immunol Immunother. 2011;60(10):1405-1418. 98. Himer L, Csóka B, Selmeczy Z, et al. Adenosine A2A receptor activation protects CD4⫹ T lymphocytes against activation-induced cell death. FASEB J. 2010;24(8):2631-2640. 99. Zarek PE, Huang C-T, Lutz ER, et al. A2A receptor signaling promotes peripheral tolerance by inducing T-cell anergy and the generation of adaptive regulatory T cells. Blood. 2008;111(1): 251-259. 88. Idzko M. Nucleotides induce chemotaxis and actin polymerization in immature but not mature human dendritic cells via activation of pertussis toxin-sensitive P2Y receptors. Blood. 2002; 100(3):925-932. 100. Gessi S, Varani K, Merighi S, et al. Expression, pharmacological profile, and functional coupling of a 2B receptors in a recombinant system and in peripheral blood cells using a novel selective antagonist radioligand. Mol Pharmacol. 2005;67(6): 2137-2147. 89. Idzko M, Panther E, Sorichter S, et al. Characterization of the biological activities of uridine diphosphate in human dendritic cells: influence on chemotaxis and CXCL8 release. J Cell Physiol. 2004;201(2):286-293. 101. Salmon JE, Cronstein BN. Fc gamma receptormediated functions in neutrophils are modulated by adenosine receptor occupancy: A1 receptors are stimulatory and A2 receptors are inhibitory. J Immunol. 1990;145(7):2235-2240. 90. Wilkin F, Duhant X, Bruyns C, et al. The P2Y11 receptor mediates the ATP-induced maturation of human monocyte-derived dendritic cells. J Immunol. 2001;166(12):7172-7177. 102. Cronstein BN. Adenosine, an endogenous antiinflammatory agent. J Appl Physiol. 1994;76(1):513. 103. Falzoni S, Chiozzi P, Ferrari D, Buell G, Di 108. Bradding P, Okayama Y, Kambe N, Saito H. Ion channel gene expression in human lung, skin, and cord blood-derived mast cells. J Leukoc Biol. 2003;73:614-620. 109. Broussas M, Cornillet-Lefèbvre P, Potron G, Nguyen P. Inhibition of fMLP-triggered respiratory burst of human monocytes by adenosine: involvement of A3 adenosine receptor. J Leukoc Biol. 1999;66(3):495-501. 110. Gu BJ, Zhang WY, Bendall LJ, et al. Expression of P2X 7 purinoceptors on human lymphocytes and monocytes: evidence for nonfunctional P2X 7 receptors. Am J Physiol Cell Physiol. 2000;279: C1189-C1197. 111. Chen Y, Shukla A, Namiki S, Insel PA, Junger WG. A putative osmoreceptor system that controls neutrophil function through the release of ATP, its conversion to adenosine, and activation of A2 adenosine and P2 receptors. J Leukoc Biol. 2004;76:245-253. 112. Lecut C, Frederix K, Johnson DM, et al. P2X1 ion channels promote neutrophil chemotaxis through Rho kinase activation. J Immunol. 2009;183(4): 2801-2809. 113. Gorini S, Callegari G, Romagnoli G, et al. ATP secreted by endothelial cells blocks CX3CL1elicited natural killer cell chemotaxis and cytotoxicity via P2Y11 receptor activation. Blood. 2010; 116(22):4492-4500. 114. Cattaneo M. ADP receptors: inhibitory strategies for antiplatelet therapy. Drug News Perspect. 2006;19(5):253-259. 115. Mahaut-Smith MP, Jones S, Evans RJ. The P2X1 receptor and platelet function. Purinergic Signal. 2011;7(3):341-356. 116. Sluyter R, Shemon AN, Barden JA, Wiley JS. Extracellular ATP increases cation fluxes in human erythrocytes by activation of the P2X7 receptor. J Biol Chem. 2004;279(43):44749-44755. From www.bloodjournal.org by guest on June 16, 2017. For personal use only. 2012 120: 2365-2375 doi:10.1182/blood-2012-04-422378 originally published online July 11, 2012 The sixth sense: hematopoietic stem cells detect danger through purinergic signaling Lara Rossi, Valentina Salvestrini, Davide Ferrari, Francesco Di Virgilio and Roberto M. Lemoli Updated information and services can be found at: http://www.bloodjournal.org/content/120/12/2365.full.html Articles on similar topics can be found in the following Blood collections Hematopoiesis and Stem Cells (3432 articles) Review Articles (710 articles) Information about reproducing this article in parts or in its entirety may be found online at: http://www.bloodjournal.org/site/misc/rights.xhtml#repub_requests Information about ordering reprints may be found online at: http://www.bloodjournal.org/site/misc/rights.xhtml#reprints Information about subscriptions and ASH membership may be found online at: http://www.bloodjournal.org/site/subscriptions/index.xhtml Blood (print ISSN 0006-4971, online ISSN 1528-0020), is published weekly by the American Society of Hematology, 2021 L St, NW, Suite 900, Washington DC 20036. Copyright 2011 by The American Society of Hematology; all rights reserved.