* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Red Blood Cells
Survey
Document related concepts
Transcript
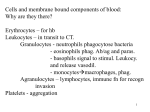
Medical Biology Blood Cells Introduction The blood is a mixture of cellular elements, fluid, proteins and metabolites Blood has four major elements: 1. Red blood cells (erythrocytes) transport oxygen from the lungs to the peripheral tissues 2. White blood cells (leukocytes) have a defensive role. 3. Platelets (thrombocytes) are important in haemostasis. 4. Plasma is the proteinaceous solution in which the above-mentioned cells circulate, and carries nutrients, metabolites, antibodies, hormones, proteins of the blood clotting system and other molecules throughout the body. Bone Marrow Derived Stem Cells The bone marrow contains at least two kinds of stem cells One population, called ‘haematopoietic stem cells’ can form all of the types of blood cells in the body. These are the cells useful clinically for bone marrow transplants. A second population is called ‘bone marrow stromal stem cells’ or ‘mesenchymal stem cells’. These nonhaematopoietic stem cells make up a small proportion of the stromal cell population in the bone marrow, and can generate bone, cartilage, fat, cells that support the formation of blood and fibrous connective tissue. These cells are under study as sources of different cell types for regenerative medicine. Methods of Studying the Blood Cells Blood is readily accessible by sampling with a needle and syringe. The name for the two main types of cells in blood derives from what is seen if blood is prevented from clotting and left to stand in a tube. Blood settles into several layers: a thick layer of clear plasma is seen at the top of the tube, beneath which is a very thin layer of white material on top of a thick layer of red material. The cells in the white material are called ‘white cells’ and the cells in the red material ‘red cells’. The usual way to look at blood is to make a very thin smear on a glass slide. The main staining method used (Romanovsky stain) involves applying several dyes which have an affinity for different cellular constituents. Under the microscope it is possible to count the proportion of different cell types in blood and, as it has been found that this reflects disease processes, a blood count is a valuable diagnostic tool. In modern laboratory practice, routine counting of cells in blood is done electronically on preparations of cells in suspension. Smears of blood are still examined for morphological abnormalities of cells. Dr. Mohammed Hussein Assi MBChB – MSc – DCH (UK) – MRCPCH Medical Biology Blood Cells Red Blood Cells Red blood cells are highly deformable and are specialized for carrying oxygen The red blood cells are responsible for oxygen transport. Red cells in peripheral blood smears appear as rounded, bright pink-stained cells. They are 6.5–8.5 µm in diameter and have a biconcave shape, appearing paler in the centre and darker at the periphery. The biconcave shape maximizes their surface area/volume ratio and thereby maximizes oxygen exchange. The bright pink colour (acidophilia) is due to the content of oxygen-carrying haemoglobin, which binds the acidic eosin dye used in staining. Red cells do not have a nucleus, as this is lost during formation. The normal concentration of erythrocytes in blood is approximately 3.9–5.5 million per microliter in women and 4.1–6 million per microliter in men. Ultrastructurally, red cells have a cell membrane which surrounds an electron-dense cytoplasm that contains haemoglobin. There are no discernible organelles as these have been lost during differentiation. Despite a lack of organelles, red cells are metabolically active and derive energy by anaerobic metabolism of glucose, and through ATP generation by the hexose monophosphate shunt. Functionally, red cells are highly deformable and are able to squeeze through small blood vessels down to 3–4 µm in diameter. The cell membrane is braced by an actin/spectrin-containing cytoskeletal meshwork, which is largely responsible for maintaining the distinctive biconcave shape. Dr. Mohammed Hussein Assi MBChB – MSc – DCH (UK) – MRCPCH Medical Biology Blood Cells Red cells have a limited lifespan and are eventually destroyed in the spleen Red cells have a lifespan of 100–120 days in the circulation. The mature red cell is unable to synthesize new enzymes to replace those lost during normal metabolic processes. Diminishing efficiency of ion pumping mechanisms is probably the main factor in red cell ageing, the cell becoming progressively less deformable until it is unable to negotiate the splenic microcirculation and is removed by phagocytosis. Hereditary spherocytosis Hereditary spherocytosis is caused by an abnormal arrangement of the internal cytoskeleton of red cells. Normally the internal surface of the cell membrane is braced by cytoskeletal proteins via interactions between ankyrin and spectri. In hereditary spherocytosis, a defect in spectrin or the ankyrin binding of spectrin is the main underlying abnormality. As a result, the red cell membrane is not braced and is easily deformed. In hereditary spherocytosis, red cells do not form their normal biconcave disc shape, but appear round and convex. They are abnormally brittle and less deformable than normal red cells, and so do not pass easily through the splenic microcirculation. They are trapped there and rapidly destroyed in large numbers; this excessive breakdown of red blood cells is called haemolysis. Sickle Cell Anaemia Point mutations in the haemoglobin gene may cause abnormal red cells. Sickle cell anaemia is caused by such a mutation, leading to precipitation of haemoglobin in red cells subject to hypoxia, which causes a sickle shape instead of the biconcave disc. sickled cells become disrupted and can also block blood vessels Hypochromic, microcytic anaemia The most common cause of anemia is deficiency of iron, which is essential for the formation of hemoglobin. Red cells are released into the circulation containing much less hemoglobin than normal, and are therefore pale staining (hypochromic) and small (microcytic) Key Facts: RBCs • Biconcave shape for high surface area/volume ratio • Main function is oxygen and carbon dioxide transport • Contain haemoglobin • Have no cell organelles • Cell membrane is braced by an actin/spectrin-containing cytoskeleton which maintains shape. Dr. Mohammed Hussein Assi MBChB – MSc – DCH (UK) – MRCPCH Medical Biology Blood Cells White Blood Cells There are five main types of white blood cells White cells use the blood for transport from the bone marrow to their major sites of activity. The majority of the functions of white blood cells take place when they leave the circulation to enter tissues. The total number of WBCs in peripheral blood is normally 4.0–11.0 × 109/L, (4000-11000/µL) There are five types of WBCs, and their names and relative proportions in the circulation are as follows: • Neutrophils 50–70% (~ 60%) • Lymphocytes 20–40% (~ 30%) • Monocytes 2–8% (~ 6%) • Eosinophils 1-4% (~ 3%) • Basophils 0-2% (~ 1%) Neutrophils, eosinophils and basophils are known as granulocytes because their cytoplasm contains prominent granules, and may also be referred to as myeloid cells because of their origin from bone marrow. Neutrophils are also commonly called polymorphonuclear leukocytes (or polymorphs) because of their multilobed nucleus. Lymphocytes and monocytes are called agranulocytes because their cytoplasm not contains prominent granules. They are found mainly in tissues such as lymph nodes and spleen. In the tissues, monocytes transform into macrophages. Dr. Mohammed Hussein Assi MBChB – MSc – DCH (UK) – MRCPCH Medical Biology Blood Cells Neutrophils Neutrophils are the most common type of white blood cell Neutrophils are the most abundant of the circulating white cells. They circulate in a resting state but, with appropriate activation, leave the blood and enter tissues, where they become highly motile, phagocytic cells. Their primary function is to ingest and destroy invading microorganisms in tissues. They play a central role in the early stages of the acute inflammatory response to tissue injury and are the major constituent of pus. There are normally 1.5–10 × 109 /L neutrophils in peripheral blood; a rise to above 10 × 10 9/L is called neutrophilia and is usually an indication of bacterial infection or tissue necrosis (e.g. myocardial infarction). A reduction in numbers of circulating neutrophils below 1.5 × 109 /L is called neutropenia or agranulocytosis; this reduction in numbers can be due to decreased production in the bone marrow or to increased destruction in the tissues. The danger of persistent neutropenia is that the patient becomes very vulnerable to severe bacterial infections. Neutrophils contain three types of granules Neutrophil cytoplasm contains three types (i.e. primary, secondary and tertiary) of membranebound vesicles (granules). o Primary granules are similar to lysosomes in other cells. They are the first granules to appear during neutrophil formation, but as the cell matures, their number falls with respect to secondary granules, making them difficult to see with light microscopy. Primary granules contain acid hydrolases, and antibacterial and digestive substances, most notably myeloperoxidase, which can be detected by the peroxidase stain. Myeloperoxidase is therefore a useful light microscopic marker not only for these granules, but also in establishing cell lineage in the diagnosis of leukaemias. o Secondary granules are specific to neutrophils and twice as numerous as primary granules, and smaller than them, they are barely visible by light microscopy. They contain substances involved in the mobilization of inflammatory mediators and complement activation. These substances are secreted into the extracellular environment. o Tertiary granules have only recently been described and contain enzymes (e.g. gelatinase) secreted into the extracellular environment. They also insert some glycoproteins into cell membranes, and this may promote cellular adhesion and hence may be involved in the phagocytic process. Dr. Mohammed Hussein Assi MBChB – MSc – DCH (UK) – MRCPCH Medical Biology Blood Cells The neutrophil nucleus has several lobes The characteristic neutrophil nucleus is composed of 2–5 distinct lobes, joined to one another by fine strands of nuclear material, the lobulation developing with cellular maturity. The chromatin is highly condensed, reflecting a low degree of protein synthesis. Neutrophils migrate into areas of tissue damage, where they have a defensive role Phagocytosis is the process whereby cells ingest extracellular particles for destruction. Neutrophils have a role in the phagocytosis of bacteria and dead cells. To reach an area of infection or tissue damage, neutrophils leave the circulation by adhering to endothelial cells using adhesion molecules expressed in response to local secretion of cytokines, and move through the endothelium and basement membrane. Once in the extravascular tissue, neutrophils respond to chemicals (chemotaxins), moving towards the highest concentration. Neutrophils typically die soon after phagocytosis, as this highly energy-dependent process uses up their glycogen reserve. When they die, their lysosomal enzymes are released into the extracellular space, causing liquefaction of adjacent tissue. The collection of dead neutrophils, tissue fluid and debris is termed ‘pus’. Key Facts: Neutrophils One of the myeloid series of white blood cells One of the granulocyte type of white blood cells Main role in phagocytosis and bacterial killing Contains three types of granule in cytoplasm Cells marked by myeloperoxidase Increase in number in blood in bacterial infection and inflammation (‘neutrophilia’). Dr. Mohammed Hussein Assi MBChB – MSc – DCH (UK) – MRCPCH Medical Biology Blood Cells Eosinophils Eosinophils have a bilobed nucleus and acidophilic granules Eosinophils have a bilobed nucleus and contain strongly eosinophilic granules. They are phagocytic, with a particular affinity for antigen–antibody complexes, but have less microbicidal activity than neutrophils. After production in the bone marrow, eosinophils are stored for approximately 8 days before release into the circulation, where they remain for about 8 h before preferentially migrating to the skin, lungs and GIT where they reside for about 8 days. They may enter lung and gut secretions via lymphatics or by direct migration. Circulating eosinophil numbers show a marked diurnal variation, being maximal in the morning and minimal in the afternoon. They increase greatly in many types of parasitic infestation, and protection against parasitic disease appears to be one of their main functions. Tissue (and sometimes blood) eosinophil numbers are also increased in certain allergic states, for example in the nasal and bronchial mucosae in hay fever and asthma and in adverse reactions to drugs. Eosinophils do not usually re-enter the circulation after tissue migration. Basophils Basophils and mast cells have common lineage and similar functions Basophils are the least common white cell in the blood. They are characterized by large, intensely basophilic, cytoplasmic granules, and share a common lineage with tissue mast cells, with which they have many structural and functional similarities. The granules of basophils and mast cells contain the proteoglycans heparin and chondroitin sulfate, together with histamine and leukotriene 3. Both basophils and mast cells have highly specific membrane receptors for the IgE produced in response to allergens. Exposure to allergens results in rapid exocytosis of their granules, thereby releasing histamine and other vasoactive mediators, and resulting in an immediate hypersensitivity (anaphylactoid) reaction. Such a reaction causes allergic rhinitis (hay fever), some forms of asthma, urticaria and anaphylaxis. Mast cells reside in support tissues, especially those beneath epithelia, around blood vessels and lining serous cavities. They are long-lived (weeks to months) and can proliferate in the tissues. In mucosae, but not in other sites, proliferation appears to depend on interaction with T lymphocytes. Dr. Mohammed Hussein Assi MBChB – MSc – DCH (UK) – MRCPCH Medical Biology Blood Cells Monocytes Monocytes are part of a cell network, the monocyte–macrophage system Monocytes are the blood- and bone marrow-located precursors of the macrophages found in tissues and lymphoid organs, and are members of a single functional unit, the monocyte– macrophage system (mononuclear phagocyte system). This system consists of: 1. The bone marrow precursors (monoblasts and promonocytes) 2. Circulating monocytes 3. Tissue macrophages, both free and fixed (histiocytes) 4. Kupffer cells of the liver 5. Sinus lining cells of the spleen and lymph nodes 6. Pulmonary alveolar macrophages 7. Free macrophages in synovial, pleural and peritoneal fluid 8. Dendritic antigen-presenting cells Monocytes are large motile, phagocytic cells. In blood films, they often have vacuolated cytoplasm. Each cell has a large, elongated nucleus, often assuming kidney or horseshoe shapes. Ultrastructurally, monocyte cytoplasm contains numerous small lysosomal granules and cytoplasmic vacuoles. The granules are of two types. One type represents primary lysosomes and is analogous to the primary granules of neutrophils. The content of the other group of granules is less certain. Numerous small pseudopodia extend from the monocyte, reflecting its phagocytic ability and amoeboid movement. Monocytes respond chemotactically to the presence of necrotic material, invading microorganisms and inflammation, and leave the blood to enter the tissues, where they are called macrophages. Lymphocytes Lymphocytes are responsible for generating specific immune responses In adults and older children lymphocytes are the second most numerous white cell in the blood, their numbers increasing in response to viral infections; they are the most numerous white cell in young children. Most circulating lymphocytes are small, but about 3% are large. Their nuclei are ovoid, with the dense chromatin typical of cells with little biosynthetic activity. There are two main types of lymphocyte, termed B and T cells, which perform different but linked roles in the generation of specific immune responses. The small mature lymphocytes circulating in the blood emigrate into tissues and into special organs of the immune system. They are responsible for immune surveillance, constantly sampling their environment for foreign material. Lymphocytes then transform into active cells, mediating the immune responses, particularly in specialized lymphoid tissues. Large lymphocytes may be seen in the blood, representing such activated lymphocytes en route to the tissues. Dr. Mohammed Hussein Assi MBChB – MSc – DCH (UK) – MRCPCH Medical Biology Blood Cells Plasma cells Plasma cells are formed from B lymphocytes and secrete immunoglobulin Plasma cells are a differentiated form of B lymphocyte and actively synthesize immunoglobulin. Plasma cells form a small population in normal marrow and are usually seen in support tissues and specialized lymphoid organs. In health, they are not found in the blood. Plasma cells are large and have an eccentrically located, round or oval nucleus with the chromatin coarsely clumped in a characteristic cartwheel or clock-face pattern, reflecting active transcription. Their cytoplasm is moderately basophilic owing to its large content of ribosomal RNA in abundant rough endoplasmic reticulum, required to manufacture the immunoglobulin protein. A well-developed Golgi complex displaces the nucleus and is visible as a paranuclear haloor pale zone (Golgi zone). WHITE BLOOD CELL ABNORMALITIES Analysis of the peripheral blood is an important part of diagnosing disease in sick patients. Part of a full blood count lists the numbers of white cells in the peripheral blood. The number of circulating white blood cells is altered in many disease processes and changes in different cell types are associated with different diseases. Increased numbers of white cells appear in the peripheral blood in a variety of disorders and provide a useful clue to underlying disease. For example: • An increase of circulating neutrophils in bacterial infections (neutrophilia) • An increase of circulating eosinophils in parasitic infestations and some allergies (eosinophilia) • An increase in circulating lymphocytes in certain viral infections (lymphocytosis) Leukemias are classified according to the cell line involved (i.e. granulocytic, monocytic, lymphocytic) and also according to their degree of malignancy. Golgi Zone Dr. Mohammed Hussein Assi MBChB – MSc – DCH (UK) – MRCPCH Medical Biology Blood Cells Platelets Platelets are small cell fragments derived from megakaryocytes and are important in haemostasis Platelets (also called ‘thrombocytes’) are small, disc shaped anuclear structures that are formed by the cytoplasmic fragmentation of huge precursor cells (megakaryocytes) in the bone marrow. Platelets contain mitochondria, microtubules, glycogen granules, occasional Golgi elements and ribosomes, as well as enzyme systems for aerobic and anaerobic respiration. Their most conspicuous organelles, however, are their granules, of which there are three types: 1. α granules are variable in size and shape and contain: PF4 (platelet factor 4), vWF(von Willebrand Factor and platelet derived growth factor, fibrinogen, fibronectin, and others. 2. Dense granules (δ granules) are electron-dense and contain small molecules such as ADP, serotonin and calcium. These components are critical for platelet activation and vasoconstriction 3. Lysosomes are membrane-bound vesicles containing lysosomal enzymes (e.g. cathepsins and hexosaminidase). Platelet cell membrane, which has a prominent glycocalyx that includes cell adhesion molecules for platelet adhesion contains many external pits which connect a system of interconnected canalicular membrane channels with the external environment. This canalicular system secretes the contents of the α granule, whereas the contractile proteins in the actin cortex are involved in clot retraction and extrusion of granule contents. A well-developed cytoskeleton incorporates a marginal band of microtubules arranged beneath the cell periphery; these polymerize into component filaments at the onset of platelet aggregation. Deep to the marginal band of microtubules and also scattered throughout the cytoplasm is the dense tubular system (dTs), consisting of narrow membranous tubules containing a homogeneous electron-opaque substance. Although histochemical studies have shown a platelet-specific isoenzyme of peroxidase within the dTs, the function of this system is poorly understood; there is some evidence that it may be the site of prostaglandin synthesis. Dr. Mohammed Hussein Assi MBChB – MSc – DCH (UK) – MRCPCH Medical Biology Blood Cells Platelets aggregate together and degranulate in haemostasis Platelets are essential to normal haemostasis, undergoing aggregation in the process. Haemostasis is achieved by the following steps: After loss of the lining endothelium of blood vessels, platelets adhere to exposed collagen by interacting with glycoprotein receptors for von Willebrand Factor attached to it. Platelet actin, myosin and microtubules cause reversible platelet moulding and adhesion along a broad surface. They then irreversibly release the contents of their granules through the canalicular system, in a secretion reaction, and synthesize thromboxane. Thromboxane, ADP and Ca2+ ions mediate adhesion of other platelets. Platelet phospholipids (with Ca ions) activate the blood clotting cascade, leading to the formation of fibrin. PLATELET DISORDERS • • • • The normal platelet count is 150-400× 109/L Severe reduction in the number of platelets well below 150 × 10 9/L in circulating blood is called ‘thrombocytopenia’. It causes spontaneous bleeding because of the failure of platelets to plug microscopic breaches in vessel walls, resulting from minor trauma. The presence of excessive numbers of circulating platelets is called ‘thrombocytosis’, and frequently occurs as a transient phenomenon when a general burst of bone marrow hyperactivity follows acute blood loss. A more persistent thrombocytosis occurs as a part of so-called ‘myeloproliferative disorder’, an uncontrolled clonal proliferation of the bloodforming cell colonies in the bone marrow. Thrombocytosis is an important predisposing factor in the development of pathological thrombosis. Dr. Mohammed Hussein Assi MBChB – MSc – DCH (UK) – MRCPCH