* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Increased Association Between Rough Endoplasmic Reticulum
Survey
Document related concepts
Transcript
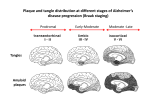
J Neuropathol Exp Neurol Copyright Ó 2009 by the American Association of Neuropathologists, Inc. Vol. 68, No. 5 May 2009 pp. 503Y514 ORIGINAL ARTICLE Increased Association Between Rough Endoplasmic Reticulum Membranes and Mitochondria in Transgenic Mice That Express P301L Tau Sébastien Perreault, MD, Olivier Bousquet, PhD, Michel Lauzon, Jacques Paiement, PhD, and Nicole Leclerc, PhD Abstract INTRODUCTION From the Département de Pathologie et Biologie Cellulaire, Université de Montréal, Montréal, Québec, Canada. Send correspondence and reprint requests to Nicole Leclerc, PhD, Département de Pathologie et Biologie Cellulaire, Université de Montréal, C.P.6128, Succ. Centre-ville, Montréal, Québec, Canada H3C 3J7; E-mail: nicole. [email protected] Sébastien Perreault and Olivier Bousquet equally contributed to the experimental work of this study. Sébastien Perreault had a studentship from Groupe de Recherche sur le Système Nerveux Central. This study was supported by Grant MOP-81092 from the Canadian Institute of Health Research and by Grant ASC-0659 from the Alzheimer Society of Canada. The neuropathologic hallmarks of Alzheimer disease (AD) are plaques that contain amyloid deposits and neurofibrillary tangles (NFTs) formed by paired helical filaments (PHFs) that are composed of insoluble tau protein (1). The numbers of NFTs more consistently correlate with the degree of dementia than amyloid plaques in AD (2Y6). Tau is preferentially associated with the microtubules of the axonal compartment in normal brain (7). During the process of neurodegeneration in AD, tau becomes hyperphosphorylated, has a decreased binding affinity to microtubules, accumulates in the somatodendritic compartment, and aggregates into insoluble intraneuronal filaments called PHFs (8Y10). Insoluble tau filaments are also characteristics of neurodegenerative diseases called tauopathies. These diseases include frontotemporal lobar degeneration with Pick bodies, corticobasal degeneration, progressive supranuclear palsy, sporadic multiple system tauopathy with dementia, argyrophilic grain disease, neurofibrillary tangle dementia, and frontotemporal dementia (FTD) with microtubule-associated protein tau gene mutation, also called FTD with parkinsonism linked to chromosome 17; all these belong to a group of diseases termed frontotemporal lobar degeneration (9, 11). The importance of tau dysfunction in neurodegeneration was recently supported by the identification of mutations in its gene in patients who have FTD with parkinsonism linked to chromosome 17 (12, 13). The precise role of tau in neurodegeneration, however, remains obscure. The contribution of tau to neurodegeneration was confirmed in mouse models in which wild-type human tau is overexpressed. Although these models do not entirely recapitulate the landmarks of tauopathies (i.e. they did not develop NFTs), they indicate that too much tau is detrimental to neurons (14Y17). In the spinal cord, inclusions of hyperphosphorylated tau in the axonal proximal segment were associated with axonal degeneration, fewer microtubules, and reduced axonal transport. Since the discovery of tau mutations, several transgenic mice have been produced that express mutated forms of human tau. For example, the overexpression of the R406W mutation induced formation of tau inclusions that shared some properties with NFTs (18). Most notably, these inclusions were associated with memory deficits. In the transgenic mice JNPL3 that express the mutant J Neuropathol Exp Neurol Volume 68, Number 5, May 2009 503 In several neurodegenerative diseases, including Alzheimer disease, the neuronal microtubule-associated protein tau becomes hyperphosphorylated, accumulates in the somatodendritic compartment, and aggregates into insoluble filaments. The consequences of the accumulation of hyperphosphorylated tau in the somatodendritic compartment remain poorly characterized at the early stage of disease before the formation of tau insoluble filaments. We investigated the ultrastructural changes induced by this accumulation in the neuronal soma of motor neurons in asymptomatic JNPL3 mice that overexpress mutant tau, P301L. More numerous contacts between rough endoplasmic reticulum (RER) membranes and mitochondria were observed in JNLP3 mice compared with wild-type mice. This correlated with a preferential increase of the amount of tau at the surface of RER membranes but not at the surface of mitochondria, as revealed by tau immunogold labeling. Using a subcellular fractionation procedure, an increased amount of phosphorylated tau was identified in the rough microsome subfraction, wherein the RER marker, ribophorin, was enriched. A similar increase was noted in the rough microsome subfraction isolated from Alzheimer disease brains. The association of hyperphosphorylated tau with ER membranes was confirmed by double immunogold labeling of the subfraction enriched in ER membranes isolated from Alzheimer disease brains. These results suggest that more contacts between RER membranes and mitochondria resulting from the accumulation of tau at the surface of RER membranes might contribute to tau-induced neurodegeneration. Key Words: Alzheimer disease, Microtubule-associated protein tau, Mitochondria, Neurodegeneration, P301L, Rough endoplasmic reticulum. Copyright @ 2009 by the American Association of Neuropathologists, Inc. Unauthorized reproduction of this article is prohibited. Perreault et al J Neuropathol Exp Neurol Volume 68, Number 5, May 2009 human form of tau P301L, true NFTs have been observed and correlated with neurodegeneration (19). This mutation is located in the second repeat of tau microtubule-binding domain and reduces its binding to microtubules (20). In JNPL3 mice, hyperphosphorylated tau accumulates in the somatodendritic compartment and forms NFTs in the motor neurons of the spinal cord, whereas neurons at the preYtangle stage predominate in the brain (19). The accumulation of tau protein in the soma of neurons is associated with neurodegeneration, but a pool of tau is detected in the soma in normal conditions. This population of tau has a level of phosphorylation higher than the axonal tau (21, 22). In a recent study, we showed that somatic tau was associated with Golgi membranes (23). The somatic pool of tau can increase under certain physiological conditions. A somatodendritic accumulation of phosphorylated tau in CA3 pyramidal cells was found in the hippocampus of hibernating squirrels (24). This accumulation was correlated with the regression of the synaptic contacts of the mossy fibers on the apical dendrites of the pyramidal cells and disappeared when synaptic contacts were reformed at the end of hibernation, indicating that the somatodendritic accumulation of hyperphosphorylated tau is a transitory and reversible event. In tauopathies, the somatodendritic accumulation of hyperphosphorylated tau becomes irreversible. The consequences of this permanent accumulation on the integrity of the somatodendritic compartment remain poorly characterized. Alterations of the morphology of the endoplasmic reticulum (ER) and the Golgi apparatus have been reported in AD brain (25, 26), but it is unclear whether these changes are caused by the accumulation of hyperphosphorylated tau in the soma. The subcellular distribution of tau filaments was examined in neuronal soma in AD brain using immunogold labeling. Tau filaments were found to arise from the nuclear membrane (which is formed of rough ER [RER] membranes) and smooth ER membranes (27). We recently reported that the overexpression of tau induced a fragmentation of the neuronal Golgi both in neuronal cultures and in JNPL3 mice (28). This event was more frequent when a mutated form of tau associated with frontotemporal lobar degeneration was overexpressed in neuronal cultures. The fragmentation of the Golgi induced by tau was not related to apoptosis in neurons. In JNPL3 mice, the fragmentation of the Golgi coincided with the somatodendritic accumulation of hyperphosphorylated tau before tangle formed, indicating that this reorganization of the Golgi occurred early in the process of neurodegeneration (28). In transgenic mice that overexpress the P301S mutant, a decrease of mitochondria and RER membranes was observed (29). Ultrastructural analysis of tau transgenic mice revealed that tau filaments were often observed in the vicinity of membranes. In JNPL3 mice, tau filaments were located in the vicinity of the nuclear membrane (30). The overexpression of human tau in lamprey also resulted in the formation of tau filaments associated with membranous elements including ER membranes (31). In previous studies, the consequences of tau accumulation on the ultrastructural integrity of the soma were examined at the end stage of the disease when tau filaments were present within a neuron. Several studies have demonstrated, however, that the accumulation of hyperphosphorylated tau in the somatodendritic compartment can be detrimental to a neuron without the formation of tau filaments. For example, in Drosophila, the accumulation of hyperphosphorylated tau after the overexpression of either human wild-type or mutant tau was sufficient to induce neurodegeneration (32). In a mouse model expressing the human mutant form of tau P301L that could be repressed by doxycycline, memory improvement was noted when human tau expression was suppressed although NFTs continued to form (33). In vitro studies have provided some insights on how hyperphosphorylated tau exerts its toxicity. Hyperphosphorylated tau but not PHFs isolated from AD brain inhibited microtubule assembly and promoted the disruption of preformed microtubules by the sequestration of normal tau and MAP2 (34, 35). In the present study, we examined the ultrastructural changes induced by the accumulation of hyperphosphorylated tau in the soma occurring before the formation of NFTs to understand how this accumulation can be detrimental to a neuron. This point was investigated in motor neurons of the spinal cord of JNPL3 mice in which NFTs are observed. 504 MATERIALS AND METHODS Electron Microscope Immunocytochemistry on Spinal Cord Sections JNPL3 and age-matched wild-type mice were purchased from Taconic Farms (Germantown, NY). The use of animals and all surgical procedures described in this article were carried out according to The Guide to the Care and Use of Experimental Animals of the Canadian Council on Animal Care. Adult mice were deeply anesthetized with intraperitoneal sodium pentobarbital (Somnotol, MTC Pharmaceuticals, Cambridge, Ontario, Canada, 65 mg/kg). They were perfused through the ascending aorta with 20 mL of 0.1 M cacodylate buffer ([CB] pH 7.4, room temperature), followed by 100 mL of freshly prepared fixative containing 2.5% glutaraldehyde (J. B. Em Services, Pointe Claire, Quebec, Canada) and 1% paraformaldehyde (Fisher, Ottawa, Ontario, Canada) in CB. The spinal cords were removed and kept in the same fixative for 1 hour at room temperature after which they were washed in CB. The spinal cords were cut in slices of 100 Km with a vibratome. The slices were then cut in half, with one half containing the posterior horns and the other half containing the anterior horns. The anterior horn half slices containing motor neurons were postfixed in 1% osmium tetroxide (J. B. Em Services) and 1.5% potassium ferrocyanide (Sigma, Oakville, Ontario, Canada) in CB for 30 minutes at 4-C. After an extensive wash in buffer, the slices were dehydrated in a graded series of alcohols at 4-C, then washed twice for 10 minutes in 100% ethanol at room temperature and embedded in LR White resin (J. B. Em Services). The resin was polymerized under anaerobic conditions for 48 hours at 56-C. Ultrathin sections (approximately 60 nm) were cut with an ultramicrotome and placed on single-slot nickel grids coated with Formvar (Mecalab Ltd, Pointe-aux-Trembles, Montréal, Quebec, Canada). Each Ó 2009 American Association of Neuropathologists, Inc. Copyright @ 2009 by the American Association of Neuropathologists, Inc. Unauthorized reproduction of this article is prohibited. J Neuropathol Exp Neurol Volume 68, Number 5, May 2009 RER/Mitochondria Association in Mutant Tau Mice grid contained 2 sections of 1 mm (width) 1.5 mm (height). These sections were then processed for postembedding immunocytochemistry, as previously described (36). A polyclonal antibody directed against the human tau 346Y352 (kindly provided by Virginia M.-Y. Lee, University of Pennsylvania, Philadelphia, PA) was used for tau immunogold labeling (37) at a dilution of 1:100. Sections from 1 transgenic and 1 wild-type mouse were simultaneously processed in each immunogold labeling experiment. Four grids per animal were processed at a time for a total of 2 times to make sure that the pattern of the immunogold staining was reproducible. were again washed and then revealed by chemiluminescence (Amersham Pharmacia Biotech, Québec, Quebec, Canada). The following primary antibodies were used: the monoclonal antibody directed against tau not phosphorylated at S198, S199, or S202, Tau-1 (1:1000; Oncogene Research Products, San Diego, CA), a polyclonal phosphorylation-insensitive anti-tau antibody directed against human tau 346-352 (1:1000; kindly provided by Virginia M.-Y. Lee, University of Pennsylvania) (37), the monoclonal antibody HT7 directed against human tau (1:100; Pierce Endogen, Rockford, IL), a polyclonal antibody against ribophorin (1:500; kindly provided by Dr G. Kreibich, New York University School of Medicine, New York, NY), a polyclonal antibody against calnexin (1:3000; Stressgen Biotechnologies, Victoria, British Columbia, Canada), the monoclonal anti-KDEL receptor (KDELR) antibody (1:250), the monoclonal antiYsyntaxin-6 antibody (1:1000; Stressgen Biotechnologies), and the monoclonal antibody anti-MAP2 (1:1000; clone HM2, Sigma). The following primary antibodies directed against phosphorylated tau were used: the monoclonal antibody AT8 (1:200; Pierce Endogen), CP9 (1:100), CP13 (1:100), PG-5 (1:100), and PHF-1 (1:100; kindly provided by Dr Peter Davies, Albert Einstein, Bronx, NY) directed against tau phosphorylated at S199/S202/T205, T231, S202, S409, and S396/S404, respectively. Quantitative Morphometric Analysis of Number of Contacts Between RER and Mitochondria The initial goal of the study was to investigate the subcellular localization of tau in JNPL3 mice before the formation of NFTs. Only motor neurons with well-defined and preserved Golgi, RER, and nuclear membranes were chosen for the analysis. One micrograph that included the Golgi and a portion of the nucleus was taken per motor neuron at a magnification of 28K. During the quantitative analysis of tau immunogold on membranes, we noted that the number of contacts between RER membranes and mitochondria was increased in JNPL3 mice. To quantify this observation, the number of RER/mitochondria contacts per micrometer of RER membranes was calculated for each micrograph representing 1 motor neuron. In wild-type and JNPL3 mice, 52 and 126 motor neurons, respectively, were analyzed. Subcellular Fractionation Brains were dissected from wild-type and JNPL3 mice, and subcellular fractions were generated using the protocol previously described by Lavoie et al (38) in 1996 and modified as described in our recent studies (23, 39). Briefly, total microsomes were isolated by differential centrifugation, and ER and Golgi elements were subsequently separated by ultracentrifugation in a sucrose step-gradient. The same protocol of subcellular fractionation was applied to frozen human tissues from the frontal cortex. Human tissues from 4 AD patients and 4 control patients presenting no sign of cognitive impairment were obtained at the Brain Bank from the Douglas Hospital Research Center affiliated to McGill University, Montréal, Quebec, Canada. A neuropathologic analysis was performed blinded to the clinical diagnosis in accordance with established criteria. The use of human tissue was approved by the institutional ethical review committee of the University of Montreal. Immunoblot Analysis Protein assay was performed on the subfractions isolated from mouse brain and human brain (Bio-Rad kit, Bio-Rad Laboratories, Mississauga, Ontario, Canada). Equal amounts of proteins were loaded in each lane and electrophoresed in a 7.5% polyacrylamide gel. After separation, proteins were electrophoretically transferred to a nitrocellulose membrane. The nitrocellulose strips were incubated with the primary antibodies for 90 minutes at room temperature. They were then washed with PBS and incubated with the peroxidase-conjugated secondary antibodies. Membranes Ó 2009 American Association of Neuropathologists, Inc. Electron Microscopy on the Rough Microsome Subfraction The rough microsome (RM) subfraction isolated from control and AD brain was fixed using 2.5% glutaraldehyde (J. B. Em Services), recovered onto Millipore membranes (Millipore, Bedford, MA) by the random filtration technique of Baudhuin et al (40) and processed for electron microscopy as previously described (38). The PHF-1 antibody was diluted 1:10, and the anti-calnexin antibody, 1:100. An antimouse antibody conjugated to 10-nm gold particles (1:10) and an anti-rabbit antibody conjugated to 5-nm gold particles (1:10) were used to reveal the localization of PHF-1 and the anti-calnexin antibody, respectively (Sigma). Immunogold labeling was performed on the RM subfractions prepared from 2 control and 2 AD brains. Statistical Analysis The counts of the number of gold particles on the membranous elements in motor neurons of the spinal cord of wild-type and JNPL3 mice were subjected to a 2-way analysis of variance test to detect any interaction between the sets of experiments. Because no interaction was found between the sets of experiments, they were combined. The differences between the types of mice (wild-type and JNPL3 mice) were analyzed by a 1-way analysis of variance. Statistical significance was accepted if p G 0.05. RESULTS The Association of RER Membranes With Mitochondria Was Increased in JNPL3 Mice The ultrastructural changes induced by the accumulation of hyperphosphorylated tau in the somatodendritic 505 Copyright @ 2009 by the American Association of Neuropathologists, Inc. Unauthorized reproduction of this article is prohibited. Perreault et al J Neuropathol Exp Neurol Volume 68, Number 5, May 2009 FIGURE 1. Electron microscopy of spinal cord motor neurons of wild-type (Wt) and JNPL3 transgenic (Tg) mice. There are contacts between mitochondria and rough endoplasmic reticulum (RER) membranes in both Wt and Tg mice. The RER membranes are identified by the presence of ribosomes at their surface. These contacts were twice as frequent in Tg as in Wt mice. Immunogold particles label tau protein. Scale bar = 100 nm. compartment are not well characterized at the initial stage of AD. We examined these changes in motor neurons of the spinal cord in JNPL3 mice that overexpress P301L tau. In hemizygous JNPL3 mice, P301L is expressed at levels approximately equivalent to those of endogenous tau (50% of total tau) (19). This mutant tau becomes hyperphosphorylated, accumulates in the somatodendritic compartment, and forms tangles in the motor neurons of the spinal cord in JNPL3 mice. The ultrastructural analysis was carried out in asymptomatic 5- to 10-month-old mice before tangle formation. Neurons that expressed P301L were identified by tau immunogold labeling. No gold particles were found when the primary antibody was omitted as well as when this primary antibody was preabsorbed with pure tau protein. The most noticeable ultrastructural difference between JNPL3 and wild-type mice was an increased number of contacts between RER membranes and mitochondria (Fig. 1). At the regions of contacts, the RER membranes were deprived of ribosomes and were in close apposition to the outer membrane of mitochondria, as previously noted in neuronal and nonneuronal cells (41, 42). The numbers of contacts between mitochondria and RER membranes in motor neurons were evaluated for each mouse type in 2 sets of experiments, and the mean T SD was calculated for each animal. Because no difference was noted between the 2 sets of experiments, the results of each mouse type were combined. In wild-type mice, the number of contacts between mitochondria and RER membranes was 0.58 T 0.72 for each micrograph taken from each motor neuron; in JNPL3 mice, the number almost doubled to 1.14 T 1.08 (Table 1). The increased number of contacts between mitochondria and RER membranes could be caused by an increase in the number of mitochondria in the soma. Indeed, over- 506 expression of tau in neuronal cultures was shown to block the transport of mitochondria to the neurites resulting in their accumulation in the soma (43). Therefore, the numbers of mitochondria were determined. The number of mitochondria per micrograph (each corresponding to a single motor neuron) was 3.09 T 1.26 in wild-type and 3.02 T 1.21 in JNPL3 mice. These numbers were not statistically different (Table 1). The numbers of mitochondria per micrometer of RER membranes for each micrograph taken from each motor neuron were also determined, and no statistical difference TABLE 1. Quantitative Analysis of the Number of Contacts Between RER and Mitochondria No. contacts between RER membranes and mitochondria in each micrograph No. mitochondria per micrometer of RER membrane in each micrograph No. mitochondria in each micrograph Total no. contacts between RER membranes and mitochondria Wild-Type Mice JNPL3 Mice p 0.59 T 0.72 n = 52 1.14 T 1.08 n = 126 G0.001 0.87 T 0.72 n = 52 0.85 T 0.58 n = 126 G0.996 3.09 T 1.26 n = 52 31 3.02 T 1.21 n = 126 143 n = number of motor neurons used for the quantitative analysis of the number of rough endoplasmic reticulum (RER)/mitochondria contacts for each type of mice. Each number represents the mean T SD. The total number of contacts between mitochondria and RER membranes results from the addition of the number of contacts in each type of mouse. Ó 2009 American Association of Neuropathologists, Inc. Copyright @ 2009 by the American Association of Neuropathologists, Inc. Unauthorized reproduction of this article is prohibited. J Neuropathol Exp Neurol Volume 68, Number 5, May 2009 RER/Mitochondria Association in Mutant Tau Mice was identified for this parameter (Table 1). These observations are consistent with a previous study in which the numbers of mitochondria in the soma and neurites were not found to be modified in another transgenic mouse model with P301L expression under the neuron-specific promoter, mThy1.2 (44). The total number of RER/mitochondria contacts for the 2 wild-type and 2 JNPL3 mice was evaluated (Table 1), with 31 and 143 contacts between RER membranes and mitochondria observed in wild-type and JNPL3 mice, respectively. procedure generates a subfraction called RM enriched in RER membranes and 3 subfractions, I1, I2, and I3, which predominantly contain Golgi membranes. In adult rat brain, tau was concentrated in the I2 subfraction (23). We previously confirmed the enrichment of RER membranes by Western blotting analysis using ER markers such as ribophorin and calnexin as well as by ultrastructural analysis (23, 39). As for the ultrastructural analysis, asymptomatic mice were used to reveal the membranous association of tau at the early stage of its accumulation in the somatodendritic compartment. The fractionation procedure was applied to the brains of wild-type and JNPL3 mice and not to the spinal cord because of the relatively limited amount of tissue. Wildtype and JNPL3 mice (n = 5 each) were used for this analysis. Ribophorin, a marker of RER, was enriched in the RM subfraction isolated from wild-type and JNPL3 mice (Fig. 2). Moreover, the dendritic microtubule-associated protein MAP2 was enriched in the RM subfraction, as noted in adult rat brain (39). Syntaxin-6, a marker of the Golgi membranes, was found in both the RM and I2 subfractions. In wild-type mice, tau was predominantly found in the I2 subfraction using a polyclonal phosphorylation-insensitive The Association of P301L With RER Membranes Was Preferentially Increased in JNPL3 Mice To investigate how the accumulation of tau in the soma could induce an increased association between RER membranes and mitochondria, tau distribution on membranous elements was examined using a subcellular fractionation procedure and immunogold labeling. Subfractions enriched in RER and Golgi membranes were isolated from wild-type and JNPL3 mice using the fractionation protocol that we previously used to show that tau was associated with the Golgi membranes in normal adult rat brain (23). This FIGURE 2. Immunoblot analysis of subfractions isolated from a wild-type (Wt1) and 3 JNPL3 (Tg1, Tg2, and Tg3) mice. Upper portions: An antibody directed against the endoplasmic reticulum marker ribophorin (Ribo) demonstrates enrichment of rough endoplasmic reticulum membranes in the rough microsome (RM) subfractions. The dendritic microtubule-associated protein, MAP2, was preferentially found in the RM subfractions as revealed by the anti-MAP2 antibody (HM2). An antibody directed against syntaxin-6 shows that Golgi membranes were found in the I2 and RM subfractions. Lower portions: The distribution of total tau was visualized using the polyclonal anti-tau antibody and the distribution of phosphorylated tau using the paired helical filament 1 (PHF-1) antibody. An arrowhead indicates an additional higher molecular weight band observed in the RM subfraction of the Tg mice by the PHF-1 antibody. The HT7 antibody specific to human tau was used to confirm the presence of human tau in the RM subfraction. E, cytoplasmic extract; I, interface; P, total membrane extract; S, cytosolic fraction. Ó 2009 American Association of Neuropathologists, Inc. 507 Copyright @ 2009 by the American Association of Neuropathologists, Inc. Unauthorized reproduction of this article is prohibited. Perreault et al J Neuropathol Exp Neurol Volume 68, Number 5, May 2009 anti-tau antibody recognizing human and rodent tau, as noted in adult rat brain (Fig. 2). In JNPL3 mice, tau was also enriched in the I2 subfraction. The distribution of phosphorylated tau was also examined in the subfractions generated from wild-type and JNPL3 mice using the antibody PHF-1 recognizing tau phosphorylated at S396/S404 (Fig. 2). Tau in the I2 subfraction was reactive to PHF-1 in both wild-type and JNPL3 mice. Interestingly, in JNPL3 mice, an additional PHF-1Ypositive band of higher molecular weight was detected in the RM subfraction, indicating that tau found in this subfraction was more phosphorylated in JNPL3 than in wild-type mice. No additional band was detected by the phospho-dependent tau antibodies AT8 and T231 (data not shown). The HT7 antibody that specifically recognizes human tau was used to confirm the presence of human tau in the RM subfraction (Fig. 2). A similar pattern of staining was generated by the HT7 antibody and the polyclonal antibody reactive to both rodent and human tau, indicating that human tau was present in all subfractions. The above results suggested that hyperphosphorylated tau could be preferentially associated with RER membranes in the soma in motor neurons in JNPL3 mice. Because other membranous markers such as the Golgi markers syntaxin-6, GM130, and TGN38, and mitochondrial markers such as VDAC were found in the RM subfraction, however, we could not conclude that tau was preferentially found at the surface of RER membranes (23, 39). To directly address this point, we quantified tau immunogold labeling at the surface of the membranous elements in the soma of motor neurons in asymptomatic mice. Quantitative analysis of the immunogold labeling was carried out for the Golgi membrane surfaces, RER membranes, nuclear membrane, and the mitochondria in wild-type and transgenic animals. To verify whether the mutant P301L had a distribution similar to that of endogenous tau, the polyclonal phosphorylation-insensitive anti-tau FIGURE 3. Immunogold labeling of tau on spinal cord sections of wild-type (Wt1 and Wt2) and transgenic (Tg1 and Tg2) mice. , rough endoplasmic reticulum (RER) membranes decorated Tau immunogold labeling was observed on the Golgi membranes , and the nuclear membrane . Panels (a’) and (b’) represent enlarged views of RER membrane portions with ribosomes identified by (a) and (b) in the micrograph above them. In panels (a’) and (b’), ribosomes and gold particles are indicated by arrowheads and arrows, respectively. Scale bar = 250 nm. 508 Ó 2009 American Association of Neuropathologists, Inc. Copyright @ 2009 by the American Association of Neuropathologists, Inc. Unauthorized reproduction of this article is prohibited. J Neuropathol Exp Neurol Volume 68, Number 5, May 2009 TABLE 2. Quantitative Analysis of tau Immunogold Labeling Membranous Organelles No. particles per square micrometer of Golgi membranes No. gold particles per micrometer of RER membranes No. gold particles per micrometer of nuclear membrane Wild-Type Mice JNPL3 Mice p 8.22 T 3.03 n = 52 13.13 T 4.47 n = 126 G0.001 1.39 T 1.12 n = 52 2.75 T 1.41 n = 126 G0.001 1.65 T 1.43 n = 16 1.93 T 1.25 n = 72 G0.049 n = number of motor neurons used for the quantitative analysis of tau immunogold labeling for each type of mouse. Mean T SD are indicated. RER, rough endoplasmic reticulum. antibody recognizing human and rodent tau was used to compare the subcellular localization of total tau in wild-type and JNPL3 mice by immunogold labeling (Fig. 3). The motor neurons of the spinal cord have a large Golgi with multiple stacks of saccules that seem discontinuous around the nucleus (45). Fenestration was used to identify the cis side of the Golgi, and clathrin-coated vesicles were used to identify the trans Golgi side (45Y47). To evaluate the amount of tau on Golgi membranes, the surface of the Golgi was directly measured on enlarged electron negatives using the Northern Eclipse image analysis system. The numbers of gold particles were then counted per square micrometer of Golgi membrane (gold particles per square micrometer) for each micrograph taken from 1 motor neuron. The mean T SD was calculated for each animal. Because no difference was noted between the 2 sets of experiments, the results for each type of mice were combined. The quantitative analysis revealed 8.22 T 3.03 and 13.13 T 4.47 gold particles per square micrometer on Golgi membranes of wild-type and JNPL3 mice, respectively (Table 2). Tau immunolabeling was also noted on the RER membranes in the vicinity of the Golgi. These membranes were identified by the presence of ribosomes at their surface. The number of gold particles per micrometer of RER membrane length present in each micrograph from 1 motor neuron was determined. In wild-type mice, the number of gold particles per micrometer of RER membrane was 1.39 T 1.12, whereas in JNPL3 mice, 2.75 T 1.41 gold particles per micrometer of membrane were found (Table 2). Because the nuclear membrane is composed of RER membranes, the number of gold particles per micrometer of this membrane was also evaluated for each micrograph taken from 1 motor neuron. There were 1.65 T 1.43 gold particles per micrometer and 1.93 T 1.25 per micrometer found in wild-type and JNPL3 mice, respectively. The amount of tau found on the nuclear membrane, Golgi, and RER membranes was 1.1, 1.6, and 1.9 times higher in JNPL3 mice than in wild-type mice. These differences were statistically significant (Table 2). Finally, the number of gold particles per micrometer of mitochondrial outer membrane was analyzed. In the first set of experiments, the number of gold particles was significantly higher in JNPL3 (1.39 T 0.84) than in wild-type (0.73 T 0.63) mice (p e 0.002) (Table 2); this difference was not observed in the second set of Ó 2009 American Association of Neuropathologists, Inc. RER/Mitochondria Association in Mutant Tau Mice experiments (p e 0.375). The above data indicate that the association of the mutant P301L with the RER membranes was preferentially increased in JNPL3 mice and suggest that the increased association between RER membranes and mitochondria could be caused by the accumulation of tau at the surface of RER membranes. Tau Filaments Were Associated With RER Membranes in AD Brain We next investigated the membranous distribution of tau in AD brain. The RM, I1, I2, and I3 subfractions were isolated from control and AD brains (Table 3). The antibody directed against the RER marker ribophorin did not react with the human protein on Western blots. An antibody directed against calnexin, a protein present in both smooth and rough ER membranes, was used to show that ER membranes were concentrated in the RM subfraction in control and AD brains (Fig. 4). Calnexin immunolabeling was also noted in the I3 subfraction in the AD brain. The distribution of the Golgi membranes was investigated using an anti-KDELR antibody. This receptor mediates the recycling of ER resident proteins that have escaped to the Golgi by binding to their KDEL sequence. At steady state, this receptor is concentrated at the Golgi (48). In both control and AD brains, KDELR was predominantly found in the I1 subfraction (Fig. 4). We used the HT7 antibody to reveal the membranous distribution of total tau. In control brains, tau was found in the I2 subfraction as observed in mouse and rat brains; the highest amount of tau was in the I1 subfraction, as noted for the Golgi marker, KDELR (Fig. 4). The distribution of tau dramatically changed in AD brains. Most of the tau was redistributed from the I1 and I2 subfractions to the RM subfraction. This corroborated a previous study reporting the enrichment of hyperphosphorylated tau in a microsomal fraction isolated from the AD brain (49). The signal of tau immunoreactivity detected by the HT-7 antibody in the I1 and RM subfractions was quantified by densitometry in 4 control and 4 AD brains. The mean of the ratio I1/RM was 3.30 and 0.07 in control and AD brains, respectively. These results suggested that hyperphosphorylated tau presented a membranous distribution distinct from that of normal tau. We then examined the state of tau phosphorylation in the I1, I2, and RM subfractions (Fig. 4). In control brains, unphosphorylated tau detected by the Tau-1 antibody was TABLE 3. Characteristics of Human Tissues Clinical Diagnosis AD1 AD2 AD3 AD4 NCI1 NCI2 NCI3 NC4 Sex Age at Death, years Postmortem Delay, hours F F F M F F M F 80 85 79 71 72 67 79 75 8.25 11.25 10.75 10 13.5 17 14.79 6.5 AD, Alzheimer disease; F, female; M, male; NCI, no cognitive impairment. 509 Copyright @ 2009 by the American Association of Neuropathologists, Inc. Unauthorized reproduction of this article is prohibited. Perreault et al J Neuropathol Exp Neurol Volume 68, Number 5, May 2009 FIGURE 4. Immunoblot analysis of subfractions isolated from control and Alzheimer disease (AD) brains. An antibody directed against the endoplasmic reticulum (ER) marker, calnexin, reveals the enrichment of ER membranes in the rough microsome (RM) subfraction. The Golgi proteins are found in the interface I1, I2, and I3 subfractions as revealed by an antibody directed against the KDEL receptor (KDELR). The distribution of total tau is visualized using the monoclonal anti-tau antibody HT7. The distribution of hyperphosphorylated tau is revealed using the antibodies PHF-1, AT-8, CP13, CP9, and PG-5; the distribution of unphosphorylated tau is shown using the antibody Tau-1. In control brain, tau is concentrated in the I1 and I2 subfractions, whereas in AD brains, tau is enriched in the RM subfraction. E, cytoplasmic extract; P, total membrane extract; S, cytosolic fraction. concentrated in the I1 subfraction. A similar distribution was noted in the AD brains. Several antibodies directed against phosphorylated tau were used to examine the distribution of this population of tau protein (PHF-1, AT8, CP-9, CP-13, and PG-5). All of these antibodies revealed that hyperphosphorylated tau was predominantly found in the RM subfraction in AD brain. No staining was detected with the phospho-dependent anti-tau antibodies in the subfractions prepared from control brain in these experiments. The previous observations indicated that hyperphosphorylated tau could be associated with RER membranes in the RM subfraction. To examine this point, preembedding immunogold labeling of the RM subfraction was performed using the anti-tau antibody PHF-1 (Fig. 5). In the RM subfraction isolated from control brain, weak staining was present on vesicles (Figs. 5AYC). In the RM subfraction 510 prepared from the AD brain, PHF-1Ypositive filaments were attached to vesicles (Figs. 5DYF). To confirm the presence of tau on ER membranes, the RM subfraction isolated from AD brain was double labeled with an anti-calnexin antibody and the PHF-1 antibody (Fig. 6). The PHF-1Ypositive tau filaments associated with calnexin-positive vesicles were found in this RM subfraction. This observation corroborated a previous observation reporting the association of tau filaments with ER-like membranes in intact AD tissue (25). DISCUSSION We examined the ultrastructural alterations at the early stage of the somatodendritic accumulation of tau in motor neurons of the spinal cord in JNPL3 mice that overexpress the mutant human tau P301L. The most intriguing initial Ó 2009 American Association of Neuropathologists, Inc. Copyright @ 2009 by the American Association of Neuropathologists, Inc. Unauthorized reproduction of this article is prohibited. J Neuropathol Exp Neurol Volume 68, Number 5, May 2009 RER/Mitochondria Association in Mutant Tau Mice FIGURE 5. Immunogold labeling of tau with 10-nm gold particles in the rough microsome (RM) subfraction isolated from control (AYC) and Alzheimer disease (AD) (DYF) brains. The antibody recognizing tau hyperphosphorylated at S396/S404, PHF-1 was used. In the RM subfraction isolated from control brain, some tau immunogold labeling was found at the surface of vesicles (AYC). In the RM subfraction prepared from AD brains, PHF-1Ypositive filaments were associated with vesicles (DYF). Scale bar = 100 nm. observation was that there were more numerous contacts between RER membranes and mitochondria in JNPL3 mice than in wild-type mice. Tau immunogold labeling indicated that this increased number of contacts might result from the preferential association of tau with RER membranes. The association of tau with ER membranes was also demonstrated in AD brains. Hyperphosphorylation of tau seemed to favor this association in both JNPL3 mice and AD brains. In normal conditions, approximately 20% of the mitochondrial surface is in direct contact with the ER membranes (50), and mitochondria have been shown to interact with both smooth and rough ER membranes (51, 52). The molecular link between ER and mitochondria remains poorly characterized, but a recent study reported that mitofusin 2, a protein known to stabilize the interactions between mitochondria, is also found at the surface of ER membrane where it is responsible for the tethering of ER and mitochondria by establishing homotypic and heterotypic interactions with mitofusin 1 or 2 located at the surface of mitochondria (53). Interestingly, mutations of mitofusin 2 in humans induce Charcot-Marie-Tooth Type IIa, a peripheral sensorimotor neuropathy (54). The interaction between mitochondria and RER membranes has important physiological roles, such as homeostasis FIGURE 6. Double immunogold labeling of the rough microsome subfraction isolated from Alzheimer disease brain with the antitau antibody PHF-1 and an anti-calnexin antibody. (AYC) The PHF-1 antibody and the anti-calnexin antibody were revealed using a secondary anti-mouse antibody conjugated to 10-nm colloidal gold particles and a secondary anti-rabbit conjugated to 5-nm colloidal gold particles, respectively. Tau immunogold labeling was present on calnexin-positive vesicles either as individual gold particles (B) or as several gold particles attached to tau filaments (A, C). Scale bar = 100 nm. Ó 2009 American Association of Neuropathologists, Inc. 511 Copyright @ 2009 by the American Association of Neuropathologists, Inc. Unauthorized reproduction of this article is prohibited. Perreault et al J Neuropathol Exp Neurol Volume 68, Number 5, May 2009 of intracellular calcium, metabolic flow, protein transport, and apoptosis (51, 52). Contacts between mitochondria and ER membranes are also necessary for the biosynthesis of mitochondrial lipids. This biosynthesis occurs at mitochondria-associated membranes, which correspond to patches of ER membranes bound to mitochondria that contain several phospholipids and glycosphingolipid biosynthetic enzymes (55). Furthermore, Ca2+-sensing ER chaperones are enriched at mitochondria-associated membranes where they stabilize Ca2+-handling proteins and thereby regulate signaling of mitochondrial Ca2+ (56). Mitochondria and ER communicate by transfer of Ca2+ from 1 organelle to the other (52, 57). Mitochondria play an important role in regulating intracellular Ca2+ levels by rapidly sequestering Ca2+ released from the ER (52), and a stable interaction between these organelles is necessary for Ca2+ uptake by mitochondria from ER (58). This uptake regulates diverse processes such as aerobic metabolism, release of caspase cofactors, and feedback control of neighboring ER and plasma membrane Ca2+ channels (52). In stress conditions, an excessive uptake of Ca2+ by mitochondria can trigger apoptosis by leading to a decrease of adenosine triphosphate production, an increase in reactive oxygen species formation, induction of mitochondrial permeability transition pore, and a release of small proteins such as cytochrome c and apoptosis-inducing factor from the mitochondria to the cytosol (52). In neuronal cultures, phosphorylation of tau on T231 by CDK5 led to its release from microtubules and a concomitant increase of the retrograde transport of mitochondria and ER membranes, resulting in their closer apposition around the centrosome, transfer of Ca2+ from the ER to mitochondria, release of cytochrome c, caspase activation, and apoptosis (59). In JNPL3 mice, tau becomes hyperphosphorylated at several sites including T231 in motor neurons of the spinal cord (19). We did not observe any difference between the numbers of mitochondria per micrometer of RER membrane in the soma of motor neurons in JNPL3 mice. Moreover, although a decrease of adenosine triphosphate and an increase of reactive oxygen species production were observed in mice that overexpress P301L, no apoptotic cell death has been detected in these mice (28, 44). Interestingly, in a recent proteomic study in transgenic mice and Drosophila that overexpress P301L, it was reported that the protein levels of Bcl-2, an antiapoptotic protein, was increased in regions such as the cerebellum, which is not affected by tau pathology (60). The mechanisms that regulate the interaction between mitochondria and ER are poorly characterized. High levels of free cytosolic Ca2+ facilitate the interactions between mitochondria and ER membranes (42), and overexpression of either normal or mutated tau was accompanied by an elevation of intracellular Ca2+ levels in neuronal and nonneuronal cells. SH-SY5Y human neuroblastoma cells transfected with the tau mutants, N279K and V337M, display higher levels of intracellular Ca2+ induced by serum withdrawal than nontransfected cells (61). In the same cells, a depolarization-induced increase in intracellular Ca2+ was significantly enhanced by the expression of V337M (62). Coexpression of AA42 and tau cooperatively elevated basal levels of myoplasmic-free Ca2+, an effect that was accompanied by depolarization of the plasma membrane (63). These observations suggest that the overexpression of P301L in transgenic mice could lead to an increase of contacts between mitochondria and RER membranes by increasing intracellular Ca2+ levels. The amount of tau on RER membranes was significantly higher in JNPL3 mice than in control mice. As previously reported in neuronal and nonneuronal cells, at the contact region between RER and mitochondria, no ribosome was found at the surface of RER membranes in motor neurons (41, 42). This results in a close apposition of the RER membrane with the outer mitochondrial membrane, an event that seems to be necessary for efficient communication between these membranes. We speculate that accumulation of tau at the surface of RER could prevent the binding of ribosomes to RER membranes and thereby favor the formation of additional contacts between RER and mitochondria. Indeed, ribosomes are located in the cytosol at the initial stage of protein synthesis before binding to ER membranes for the completion of the translation process. With respect to mitochondria, the amount of tau was only increased in 1 JNPL3 mouse, suggesting that the association of tau with mitochondria is not necessarily involved in an enhanced interaction between RER and mitochondria. The inconsistency of the amount of tau found at the surface of mitochondria might indicate that tau has a higher affinity for binding to RER, Golgi, and the nuclear membrane than to mitochondria. Tau would then only begin to accumulate at the surface of mitochondria when its expression reaches a certain level. This level was not attained in the other transgenic mouse examined. Taken together, these observations suggest that the increased association of tau with RER membranes might be responsible for the formation of higher numbers of contacts between RER and mitochondria in JNPL3 mice. The accumulation of tau on RER membranes could contribute to the alteration of their function leading to neurodegeneration. The ER is involved in protein synthesis, protein folding and trafficking, cellular responses to stress, and Ca2+ homeostasis (57). The ER presents stress-signaling pathways that enable it to adapt to a panoply of stress factors. For example, the accumulation of misfolded proteins in the ER lumen induces an unfolded protein response, which switches off protein synthesis and upregulates the production of new chaperones to reestablish ER homeostasis (57). If ER stress is maintained for too long and ER homeostasis is not reestablished, the unfolded protein response triggers the activation of caspases and ultimately apoptosis. Indeed, ER stressYmediated apoptotic signal pathways may contribute to the pathogenesis of AD (64). It remains to be determined, however, whether the accumulation of tau on ER membranes does contribute to this pathway in AD. The fragmentation of the Golgi observed in transgenic mice and in primary neuronal cultures overexpressing either normal or mutated tau could indicate that the trafficking of protein from the ER to Golgi is compromised (28). This could result in an accumulation of proteins in the ER. Another possibility is that the attachment of tau to ER membranes could modify 512 Ó 2009 American Association of Neuropathologists, Inc. Copyright @ 2009 by the American Association of Neuropathologists, Inc. Unauthorized reproduction of this article is prohibited. J Neuropathol Exp Neurol Volume 68, Number 5, May 2009 RER/Mitochondria Association in Mutant Tau Mice their biophysical properties and thereby hinder protein trafficking and exit from these membranes. The association of tau with the nuclear membranes composed of RER membranes was increased before the formation of tau filaments in JNPL3 mice. This is consistent with previous observations indicating that tau filaments are in close proximity to the nuclear membranes and pores in AD brains (27). These membranes could serve as nucleating structures for tau filaments. It remains unclear, however, whether the association of tau with the nuclear membrane can compromise the communication between the nucleus and the cytoplasm. In a recent study, nuclear transport factor 2 was found to accumulate in the cytoplasm in a subset of hippocampal neurons with and without NFTs in AD brains (65). The overexpression of P301L tau results in an increase of its phosphorylation state in JNPL3 mice (19). We found that phosphorylated tau at S396/S404 was increased in the RM subfraction, where the RER marker ribophorin was enriched. In AD brains, hyperphosphorylated tau was exclusively found in the RM subfraction enriched in ER membranes. These results corroborate previous observations indicating that hyperphosphorylated tau was present on RER membranes in AD brain (66, 67). Although we cannot exclude the possibility that hyperphosphorylated tau was associated with more than 1 membranous element in this subfraction, its binding to ER membranes was confirmed by double immunogold labeling. Tau phosphorylated at T231 was also found to be associated with RER membranes in AD brain by immunocytochemistry (68), but we observed no signal in the RM subfraction isolated from the brain of JNPL3 mice using an antibody directed against tau phosphorylated at T231. The absence of signal could be explained by the fact that the RM subfraction was isolated at a very early stage of tau pathology when tau is moderately phosphorylated. Taken together, these observations suggest that hyperphosphorylation of tau might favor its association with RER membranes. It was recently reported that annonacin, a natural mitochondrial complex I inhibitor, induced a depletion of adenosine triphosphate, an increased retrograde transport of mitochondria to the cell soma, and the accumulation of hyperphosphorylated tau in the soma in rat striatal primary cultures (69). These observations indicate that oxidative damage and mitochondrial dysfunction observed at an early stage of AD could trigger the somatodendritic accumulation of hyperphosphorylated tau (70). In the light of our present results, this accumulation could in turn amplify the dysfunction of mitochondria by favoring their interaction with RER membranes. Mitochondrial dysfunction and the somatodendritic accumulation of tau could cooperate to engage a neuron on an irreversible pathway of cell death in AD brain. the anti-ribophorin antibody. The authors also thank Dr Moise Bendayan for helpful discussions. ACKNOWLEDGMENTS The authors thank Dr Virginia Lee (University of Pennsylvania, Philadelphia, PA) for providing the polyclonal anti-tau antibody, Dr Peter Davies (Albert Einstein University, Bronx, NY) for the phospho-dependent anti-tau antibodies, CP9, CP13, PG-5, and PHF-1, and Dr Gert Kreibich (New York University School of Medicine, New York, NY) for Ó 2009 American Association of Neuropathologists, Inc. REFERENCES 1. Chesselet M. Molecular Mechanisms of Neurodegenerative Diseases. Totowa, NJ: Human Press, 2000 2. Alafuzoff I, Iqbal K, Friden H, et al. Histopathological criteria for progressive dementia disorders: Clinical-pathological correlation and classification by multivariate data analysis. Acta Neuropathol 1987:74; 209Y25 3. Arriagada P, Growdon J, Hedley-Whyte ET, et al. Neurofibrillary tangles but not senile plaques parallel duration and severity of Alzheimer’s disease. Neurology 1992:42;631Y39 4. Bierer L, Hof P, Purohit D, et al. Neocortical neurofibrillary tangles correlate with dementia severity in Alzheimer’s disease. Arch Neurol 1995:52;81Y88 5. Braak H, Braak E. Neuropathological staging of Alzheimer-related changes. Acta Neuropathol 1991:82;239Y59 6. Tomlinson BE, Blessed G, Roth M. Observations on the brains of demented old people. J Neurol Sci 1970:11;205Y42 7. Mandell J, Banker G. Microtubule-associated proteins, phosphorylation gradients, and the establishment of neuronal polarity. Perspect Dev Neurobiol 1996:4;125Y35 8. Grundke-Iqbal I, Iqbal K, Quinlan M, et al. Microtubule-associated protein tau. A component of Alzheimer paired helical filaments. J Biol Chem 1986:261;6084Y89 9. Lee V, Goedert M, Trojanowski J. Neurodegenerative tauopathies. Annu Rev Neurosci 2001:24;1121Y59 10. Grundke-Iqbal I, Iqbal K, Tung Y, et al. Abnormal phosphorylation of the microtubule-associated protein tau (tau) in Alzheimer cytoskeletal pathology. Proc Natnl Acad Sci U S A 1986:83;4913Y17 11. Cairns NJ, Bigio EH, Mackenzie IR, et al. Neuropathologic diagnostic and nosologic criteria for frontotemporal lobar degeneration: Consensus of the Consortium for Frontotemporal Lobar Degeneration. Acta Neuropathol 2007:114;5Y22 12. Hutton M, Lendon CL, Rizzu P, et al. Association of missense and 5¶-splice-site mutations in tau with the inherited dementia FTDP-17. Nature 1998:393;702Y5 13. Poorkaj P, Bird TD, Wijsman E, et al. Tau is a candidate gene for chromosome 17 frontotemporal dementia. Ann Neurol 1998:43;815Y25 14. Duff K, Knight H, Refolo L, et al. Characterization of pathology in transgenic mice over-expressing human genomic and cDNA tau transgenes. Neurobiol Dis 2000:7;87Y98 15. Probst A, Götz J, Wiederhold K, et al. Axonopathy and amyotrophy in mice transgenic for human four-repeat tau protein. Acta Neuropathol 2000:99;469Y81 16. Spittaels K, Van den Haute C, Van Dorpe J, et al. Prominent axonopathy in the brain and spinal cord of transgenic mice overexpressing four-repeat human tau protein. Am J Pathol 1999:155;2153Y65 17. Ishihara T, Hong M, Zhang B, et al. Age-dependent emergence and progression of a tauopathy in transgenic mice overexpressing the shortest human tau isoform. Neuron 1999:24;751Y62 18. Tatebayashi Y, Miyasaka T, Chui DH, et al. Tau filament formation and associative memory deficit in aged mice expressing mutant (R406W) human tau. Proc Natl Acad Sci U S A 2002:99;13896Y901 19. Lewis J, McGowan E, Rockwood J, et al. Neurofibrillary tangles, amyotrophy and progressive motor disturbance in mice expressing mutant (P301L) tau protein. Nat Genet 2000:25;402Y5 20. Hutton M. Missense and splice site mutations in tau associated with FTDP-17: Multiple pathogenic mechanisms. Neurology 2001:56; S21Y25 21. Papasozomenos S, Binder L. Phosphorylation determines two distinct species of tau in the central nervous system. Cell Motil Cytoskeleton 1987:8;210Y26 22. de Ancos J, Avila J. Differential distribution in white and grey matter of tau phosphoisoforms containing four tubulin-binding motifs. Biochem J 1993:296(Pt 2);351Y54 23. Farah C, Perreault S, Liazoghli D, et al. Tau interacts with Golgi membranes and mediates their association with microtubules. Cell Motil Cytoskeleton 2006:63;710Y24 513 Copyright @ 2009 by the American Association of Neuropathologists, Inc. Unauthorized reproduction of this article is prohibited. Perreault et al J Neuropathol Exp Neurol Volume 68, Number 5, May 2009 24. Arendt T, Stieler J, Strijkstra A, et al. Reversible paired helical filament-like phosphorylation of tau is an adaptive process associated with neuronal plasticity in hibernating animals. J Neurosci 2003:23; 6972Y81 25. Gray E, Paula-Barbosa M, Roher A. Alzheimer’s disease: Paired helical filaments and cytomembranes. Neuropathol Appl Neurobiol 1987:13; 91Y110 26. Stieber A, Mourelatos Z, Gonatas NK. In Alzheimer’s disease the Golgi apparatus of a population of neurons without neurofibrillary tangles is fragmented and atrophic. Am J Pathol 1996:148;415Y26 27. Metuzals J, Robitaille Y, Houghton S, et al. Paired helical filaments and the cytoplasmic-nuclear interface in Alzheimer’s disease. J Neurocytol 1988:17;827Y33 28. Liazoghli D, Perreault S, Micheva K, et al. Fragmentation of the Golgi apparatus induced by the overexpression of wild-type and mutant human tau forms in neurons. Am J Pathol 2005:166;1499Y514 29. Yoshiyama Y, Higuchi M, Zhang B, et al. Synapse loss and microglial activation precede tangles in a P301S tauopathy mouse model. Neuron 2007:53;337Y51 30. Lin W, Lewis J, Yen S, et al. Ultrastructural neuronal pathology in transgenic mice expressing mutant (P301L) human tau. J Neurocytol 2003:32;1091Y105 31. Hall GF, Chu B, Lee G, et al. Human tau filaments induce microtubule and synapse loss in an in vivo model of neurofibrillary degenerative disease. J Cell Sci 2000:113;1373Y87 32. Wittmann C, Wszolek M, Shulman J, et al. Tauopathy in Drosophila: Neurodegeneration without neurofibrillary tangles. Science 2001:293; 711Y14 33. Santacruz K, Lewis J, Spires T, et al. Tau suppression in a neurodegenerative mouse model improves memory function. Science 2005: 309;476Y81 34. Alonso Adel C, Li B, Grundke-Iqbal I, et al. Polymerization of hyperphosphorylated tau into filaments eliminates its inhibitory activity. Proc Natl Acad Sci U S A 2006:103;8864Y69 35. Li B, Chohan MO, Grundke-Iqbal I, et al. Disruption of microtubule network by Alzheimer abnormally hyperphosphorylated tau. Acta Neuropathol 2007:113;501Y11 36. Micheva K, Vallée A, Beaulieu C, et al. beta-Actin is confined to structures having high capacity of remodelling in developing and adult rat cerebellum. Eur J Neurosci 1998:10;3785Y98 37. Garver TD, Harris KA, Lehman RA, et al. Tau phosphorylation in human, primate, and rat brain: Evidence that a pool of tau is highly phosphorylated in vivo and is rapidly dephosphorylated in vitro. J Neurochem 1994:63;2279Y87 38. Lavoie C, Lanoix J, Kan FW, et al. Cell-free assembly of rough and smooth endoplasmic reticulum. J Cell Sci 1996:109;1415Y25 39. Farah C, Liazoghli D, Perreault S, et al. Interaction of microtubule-associated protein-2 and p63: A new link between microtubules and rough endoplasmic reticulum membranes in neurons. J Biol Chem 2005:280; 9439Y49 40. Baudhuin P, Evrard P, Berthet J. Electron microscopic examination of subcellular fractions. I. The preparation of representative samples from suspensions of particles. J Cell Biol 1967:32;181Y91 41. Perkins G, Renken C, Martone ME, et al. Electron tomography of neuronal mitochondria: Three-dimensional structure and organization of cristae and membrane contacts. J Struct Biol 1997:119;260Y72 42. Wang HJ, Guay G, Pogan L, et al. Calcium regulates the association between mitochondria and a smooth subdomain of the endoplasmic reticulum. J Cell Biol 2000:150;1489Y98 43. Ebneth A, Godemann R, Stamer K, et al. Overexpression of tau protein inhibits kinesin-dependent trafficking of vesicles, mitochondria and endoplasmic reticulum: Implications for Alzheimer’s disease. J Cell Biol 1998:143;777Y94 44. David DC, Hauptmann S, Scherping I, et al. Proteomic and functional analyses reveal a mitochondrial dysfunction in P301L tau transgenic mice. J Biol Chem 2005:280;23802Y14 45. Peters A, Palay S, Webster H. The Fine Structure of the Nervous System: The Neurons and Supporting Cells. Philadelphia, PA: Saunders Company, 1976 46. Rambourg A, Clermont Y. Three-dimensional electron microscopy: Structure of the Golgi apparatus. Eur J Cell Biol 1990:51;189Y200 47. Marsh B, Mastonarde D, Buttle K, et al. Organellar relationships in the Golgi region of the pancreatic beta cell line, HIT-115, visualized by high resolution electron tomography. Proc Natl Acad Sci U S A 2001:98; 2399Y406 48. Bard F, Mazelin L, Pechoux-Longin C, et al. Src regulates Golgi structure and KDEL receptorYdependent retrograde transport to the endoplasmic reticulum. J Biol Chem 2003:278;46601Y6 49. Iqbal K, Grundke-Iqbal I, Zaidi T, et al. Defective brain microtubule assembly in Alzheimer’s disease. Lancet 1986:2;421Y26 50. Rizzuto R, Pinton P, Carrington W, et al. Close contacts with the endoplasmic reticulum as determinants of mitochondrial Ca2+ responses. Science 1998:280;1763Y66 51. Goetz JG, Nabi IR. Interaction of the smooth endoplasmic reticulum and mitochondria. Biochem Soc Trans 2006:34;370Y73 52. Walter L, Hajnoczky G. Mitochondria and endoplasmic reticulum: The lethal interorganelle cross-talk. J Bioenerg Biomembr 2005:37; 191Y206 53. de Brito OM, Scorrano L. Mitofusin 2 tethers endoplasmic reticulum to mitochondria. Nature 2008:456;605Y10 54. Zuchner S, Mersiyanova IV, Muglia M, et al. Mutations in the mitochondrial GTPase mitofusin 2 cause Charcot-Marie-Tooth neuropathy type 2A. Nat Genet 2004:36;449Y51 55. Vance JE. Phospholipid synthesis in a membrane fraction associated with mitochondria. J Biol Chem 1990:265;7248Y56 56. Hayashi T, Su TP. Sigma-1 receptor chaperones at the ER-mitochondrion interface regulate Ca(2+) signaling and cell survival. Cell 2007:131; 596Y610 57. Berridge MJ. The endoplasmic reticulum: A multifunctional signaling organelle. Cell Calcium 2002:32;235Y49 58. Mironov S, Ivannikov M, Johansson M. Ca2+i signaling between mitochondria and endoplasmic reticulum in neurons is regulated by microtubules. J Biol Chem 2005:280;715Y21 59. Darios F, Muriel MP, Khondiker ME, et al. Neurotoxic calcium transfer from endoplasmic reticulum to mitochondria is regulated by cyclin-dependent kinase 5Ydependent phosphorylation of tau. J Neurosci 2005:25; 4159Y68 60. Karsten SL, Sang TK, Gehman LT, et al. A genomic screen for modifiers of tauopathy identifies puromycin-sensitive aminopeptidase as an inhibitor of tau-induced neurodegeneration. Neuron 2006:51; 549Y60 61. Furukawa K, D’Souza I, Crudder CH, et al. Pro-apoptotic effects of tau mutations in chromosome 17 frontotemporal dementia and parkinsonism. Neuroreport 2000:11;57Y60 62. Furukawa K, Wang Y, Yao PJ, et al. Alteration in calcium channel properties is responsible for the neurotoxic action of a familial frontotemporal dementia tau mutation. J Neurochem 2003:87;427Y36 63. Christensen RA, Shtifman A, Allen PD, et al. Calcium dyshomeostasis in beta-amyloid and tau-bearing skeletal myotubes. J Biol Chem 2004: 279;53524Y32 64. Takuma K, Yan SS, Stern DM, et al. Mitochondrial dysfunction, endoplasmic reticulum stress, and apoptosis in Alzheimer’s disease. J Pharmacol Sci 2005:97;312Y16 65. Sheffield LG, Miskiewicz HB, Tannenbaum LB, et al. Nuclear pore complex proteins in Alzheimer disease. J Neuropathol Exp Neurol 2006: 65;45Y54 66. Kopke E, Tung YC, Shaikh S, et al. Microtubule-associated protein tau. Abnormal phosphorylation of a non-paired helical filament pool in Alzheimer disease. J Biol Chem 1993:268;24374Y84 67. Wang JZ, Grundke-Iqbal I, Iqbal K. Glycosylation of microtubule-associated protein tau: An abnormal posttranslational modification in Alzheimer’s disease. Nat Med 1996:2;871Y75 68. Luna-Munoz J, Garcia-Sierra F, Falcon V, et al. Regional conformational change involving phosphorylation of tau protein at the Thr231, precedes the structural change detected by Alz-50 antibody in Alzheimer’s disease. J Alzheimers Dis 2005:8;29Y41 69. Escobar-Khondiker M, Hollerhage M, Muriel MP, et al. Annonacin, a natural mitochondrial complex I inhibitor, causes tau pathology in cultured neurons. J Neurosci 2007:27;7827Y37 70. Moreira PI, Santos MS, Oliveira CR. Alzheimer’s disease: A lesson from mitochondrial dysfunction. Antioxid Redox Signal 2007:9; 1621Y30 514 Ó 2009 American Association of Neuropathologists, Inc. Copyright @ 2009 by the American Association of Neuropathologists, Inc. Unauthorized reproduction of this article is prohibited.