* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Spice/K2 drugs – more than innocent substitutes for marijuana
Polysubstance dependence wikipedia , lookup
Nicotinic agonist wikipedia , lookup
Discovery and development of angiotensin receptor blockers wikipedia , lookup
Pharmaceutical industry wikipedia , lookup
Pharmacokinetics wikipedia , lookup
Prescription costs wikipedia , lookup
Medical cannabis wikipedia , lookup
NK1 receptor antagonist wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Drug interaction wikipedia , lookup
Urban legends about drugs wikipedia , lookup
Drug discovery wikipedia , lookup
Pharmacognosy wikipedia , lookup
Neuropharmacology wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
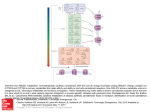
International Journal of Neuropsychopharmacology (2014), 17, 509–525. doi:10.1017/S1461145713001247 © CINP 2013 REVIEW Spice/K2 drugs – more than innocent substitutes for marijuana Jolanta B. Zawilska and Jakub Wojcieszak Department of Pharmacodynamics, Medical University of Lodz, Lodz, Poland Abstract Smokeable herbal mixtures containing synthetic agonists of cannabinoid receptors, known under brand names such as Spice, K2 and Kronic, represent a relatively new type of designer psychoactive drugs that has recently emerged on the recreational drug market. Although the Spice packages are labelled ‘not for human consumption’ or ‘for aromatherapy only’ and declared to be purely herbal, these herbal mixtures produce cannabis-like effects after smoking. This review surveys the current state of knowledge regarding the pharmacological properties of synthetic cannabimimetics and the prevalence and pattern of their use. Special emphasis is given to the negative consequences of using these products, including, among others, hallucinations, psychoses with delusions, seizures, cardiovascular symptoms and acute kidney injury. Received 19 July 2013; Reviewed 16 August 2013; Revised 27 September 2013; Accepted 27 September 2013; First published online 29 October 2013 Key words: Abuse, adverse effects, Spice, synthetic cannabimimetics, THC. Introduction Synthetic agonists of cannabinoid receptors (hereafter ‘synthetic cannabimimetics’) represent a relatively new type of designer psychoactive drugs that has recently emerged on the recreational drug market (Fattore and Fratta, 2011; Zawilska, 2011; Winstock and Barratt, 2013). Smokeable herbal mixtures containing synthetic cannabimimetics are sold under a variety of brand names; the most common are Spice in Europe, K2 in the United States, Kronic in Australia and New Zealand. Around 2004, in various European countries, herbal mixtures of the Spice-type, advertised as meditation potpourris, bath additives, air refreshers or tropical car perfumes (Fattore and Fratta, 2011), became available on the internet and in specialized ‘head shops’, which sell paraphernalia for cannabis users. They gained significant popularity in 2008, and at that time sales of these mixtures dramatically increased in Germany (Dresen et al., 2010). Growing suspicion that synthetic psychoactive compounds could have been added to these herbal mixtures was finally confirmed at the end of 2008 by the detection of two synthetic cannabimimetic agents in Spice, namely the cyclohexylphenol CP 47,497-C8 and the aminoalkylindole JWH-018 (Auwärter et al., 2009; Uchiyama et al., 2010). As compared to traditional illicit psychoactive compounds of abuse, very little information exists in the medical literature concerning new designer recreational drugs, including synthetic cannabimimetics. Spice products are usually sold in metal-foil sachets, typically containing 1–3 g of dried vegetable matter (leaves, flowers, resin) to which one or more synthetic cannabimimetics have been added. They are relatively inexpensive, roughly €9–12 g−1 ($10–20 g−1), and €26–30 for sachets sufficient for around eight joints (EMCDDA, 2009; Johnson et al., 2013). The Spice packages are labelled ‘not for human consumption’ or ‘for aromatherapy only’ and declared to be purely herbal, containing plant ingredients considered inert, and rarely list plants that naturally contain psychoactive compounds, such as wild dagga (Leonotis leonurus) or Indian warrior (Pedicularis densiflora) (Dresen et al., 2010; Zuba et al., 2011). It has to be emphasized that the multicoloured packaging of the Spice-type products is very attractive and highly sophisticated. Many of them have a wide-open-eye imprint and circulate under such exotic names as Bombay Blue, Ex-ses, Experience-Chill, Ice Bud Extra Cold, Herbal Dream, Mojo, Moon Rocks, Red Magic, Space Truckin’, Spice Gold Spirit, Spice Tropical Synergy, SpiceWorld420 and Yucatan Fire (Harris and Brown, 2013). Because of their packaging and very attractive scent, Spice products are not easily identified by non-users as drugs. Synthetic cannabimimetics – the major biologically active components of Spice Address for correspondence: Professor J. B. Zawilska, Department of Pharmacodynamics, Medical University of Lodz, ul. Muszynskiego 1, PL90-151 Lodz, Poland. Tel.: +48-42-6779294 Fax: +48-42-6788398 Email: [email protected] At present, over 150 synthetic cannabimimetics are known, and the list is constantly growing. Some of the first compounds detected in Spice were synthesized and named after John W. Huffman, a medicinal chemist 510 J. B. Zawilska and J. Wojcieszak 0 0 0 N JWH-015 N 0 JWH-018 CI N 0 JWH-081 N JWH-122 O O F I O O N JWH-203 N JWH-250 O O N AM-694 N RCS-4 OH OH H OH H O CP 47,497-C8 HU-210 Fig. 1. Chemical structures of synthetic cannabimimetics. at Clemenson University, USA (Huffman et al., 1994). Notably, JWH-018 (1-pentyl-1H-indol-3-yl)-1naphthalenyl-methanone), the most studied and best characterized synthetic cannabinoid to date, was one of the first compounds to be abused due to its high pharmacological activity and ease of synthesis (Huffman et al., 1994; Atwood et al., 2009; Huffman, 2009). Today, aminoalkylindoles, phenacetylindoles and naphthoylpyrolles designed by J. W. Huffman represent the dominant cannabimimetic compounds detected in the Spice products (Hudson and Ramsey, 2011; Carroll et al., 2012). The other chemically distinct groups of synthetic cannabimimetics include: (1) the cyclohexylphenol (CP) compounds synthesized by Pfizer in the 1970s (e.g. CP 47,497 and its modified version CP 47,497-C8), (2) the HU-compounds, synthesized in the 1960s by Raphael Mechoulam at the Hebrew University (e.g. HU-210) and (3) the benzoylindoles, such as AM-694 and AM-2201 synthesized by Alexandros Makriyannis, or RCS-4 and RCS-8 produced by Research Chemical Suppliers (EMCDDA, 2009; Lindigkeit et al., 2009; Hudson et al., 2010; Uchiyama et al., 2010, 2011a, b; Seely et al., 2011). With the exception of HU-210, synthetic cannabimimetics are structurally distinct from Δ9-tetrahydrocannabinol (Δ9-THC), the primary psychoactive component of natural cannabis (Fig. 1). Spice products can be distinguished by the presence of: (1) pronounced variations in the core structure of synthetic cannabimimetics, (2) considerable inter-and intrabatch variability in smoking mixtures, both in terms of substances present and their quantity and (3) ever changing composition. Once some compounds became regulated, new analogues appeared on the market in order to satisfy demand and at the same time to avoid criminalization (Lindigkeit et al., 2009; Hudson and Ramsey, 2011; Dargan et al., 2011; Simolka et al., 2012; Ernst et al., 2012; Langer et al., 2013; Uchiyama et al., 2013). Despite modifications in the chemical structure, all of the synthetic cannabimimetics are lipid soluble, nonpolar and typically consist of 20 to 26 carbon atoms, which explains why they volatilize readily when smoked. Synthetic cannabimimetics found in the Spice products can be classified into one of the following groups (Zawilska, 2011; Favretto et al., 2013): • So called JWH compounds, at present including 146 members. This group has been divided into five subgroups: – naphthoylindoles, constituting the largest group of 74 compounds (e.g. JWH-015, JWH-018, JWH-019, JWH-073, JWH-122, JWH-200, JWH-210, JWH-387, JWH-398); – naphthylmethylindoles, 9 compounds (e.g. JWH175); – naphthoylpyrroles, 32 compounds (e.g. JWH-147); – naphthylmethylindenes, 3 compounds (e.g. JWH-176); – phenacetylindoles, 28 compounds (e.g. JWH-203, JWH-250, JWH-253). • Cyclohexylphenols (CP 47,497 and its homologues). • Benzoylindoles (e.g. AM-694, AM-2201, AM-679, RCS-4). • Classical cannabinoids (e.g. HU-210). • Other compounds, such as, for example, WIN 55,212-2, UR-144 and TMCP series. Synthetic cannabimimetics as drugs of abuse 511 UR-144 ((1-pentyl-1H-indol-3-yl)(2,2,3,3-tetramethylcyclopropyl)methanone), originally synthesized by Abbot Laboratories, has recently been identified in various herbal products obtained via online vendors in Russia (Kavanagh et al., 2013) and in herbal incense seized for drug trafficking in South Korea (Choi et al., 2013). The TMCP compounds (TMCP-H, TMCP-018, TMCP-020, TMCP-2201, TMCP-200, TMCP-1220 and TMCP-1220-azepane), containing a 2,2,3,3-tetramethylcyclopropanecarbonyl moiety, represent a novel class of synthetic cannabimimetics. They have been identified and detected in smoking mixtures seized in Russia and Belarus (Shevyrin et al., 2012). Interestingly, one of them, TMCP-2201 (1-(5fluoropentyl)-1H-indol-3-yl)-2,2,3,3-tetramethylcyclopropyl) methanone, also known under the name of XLR-11, has been detected in samples of ‘Mr. Happy’, ‘Clown Loyal’ and ‘Lava’ products, while its metabolite was identified in clinical specimens from US patients suffering with acute kidney injury associated with synthetic cannabimimetics use (CDC, 2013). Other identified substances include (Lindigkeit et al., 2009; Zuba et al., 2011): • Amides of fatty acids: oleamide, palmitamide and stearamide, which could mimic the action of natural cannabinoids. • Substances presumably originating from plants, e.g. eugenol, eucalyptol, phytosterole, thymol, squalene, persicol, fatty acids and their esters (ethyl linoleate, linoleic acid, palmitic acid). • Flavours (ethyl vanillin, acetyl vanillin). • Preservatives (benzophenone, benzyl benzoate, hydroxybenzoic acid). In addition, Spice products are supposed to contain up to 15 different vegetal compounds, which gives rise to a wide variety of drug combinations (Dresen et al., 2010; Zuba et al., 2011). Moreover, they have been found to contain large amounts of vitamin E, added to hamper the analysis of the active cannabinoids (Dresen et al., 2010; Zuba et al., 2011). To create the herbal products, synthetic cannabimimetics are dissolved in an organic solvent (e.g. acetone) and the resulting solution is sprayed on plant material. The doped plant material is then dried and smoked in a similar fashion to actual cannabis. Spice products typically have a pleasurable smell and taste, for example honey or vanilla (Fattore and Fratta, 2011). Spice – prevalance, pattern of use, users profile Several factors contribute to the growing popularity of synthetic cannabimimetics, namely the expectation to achieve a more intense high than after cannabis, affordability, easy access, belief in the safety of use and avoidance of detection in standardized drug tests (Fattore and Fratta, 2011). Among adolescents and young adults lifetime use of Spice/K2 products was reported to be around 10% (Hu et al., 2011; Forrester et al., 2012; Vandrey et al., 2012), but the recently published results of a self-reported study that included 14966 participants from different countries around the world revealed lifetime use to be more prevalent (16.8%) (Winstock and Barratt, 2013). In 2011, one-year prevalence of Spice use by 12th grade students in USA was 11.4%. Thus, Spice was the second most popular illicit substance used by this group, behind marijuana (Office of National Drug Control Policy, 2011). Users are primarily male adolescents and young adults, having at least a high school level of education (Hu et al., 2011; Forrester et al., 2012; Vandrey et al., 2012; Winstock and Barratt, 2013). Accumulating evidence demonstrates the increasing popularity of synthetic cannabimimetics amongst soldiers (Loeffler et al., 2012) and athletes (Heltsley et al., 2012). An analysis of 101 serum samples from 80 subjects, provided by several medical and forensic centres in Germany, demonstrated that 56.4% of them were positive for at least one synthetic cannabimimetic. The most prevalent compound was JWH-081 (found in 55% of samples), followed by JWH-250 (47%), JWH-018 (9%) and JWH-073 (6%). Ten serum samples were positive for only one compound, 35 samples contained two, eight samples three, and four samples contained four (Dresen et al., 2011). The primary reasons for the use of synthetic cannabimimetics are: curiosity, enjoyment of the effects, satisfaction, a desire to achieve marijuana-like psychoactive effects while avoiding detection in drug tests and, less frequently, to aid the reduction or cessation of cannabis use (Fattore and Fratta, 2011; Vandrey et al., 2012; Barratt et al., 2013). Spice use was found to occur at a residence, with the users alone or in small groups (Forrester et al., 2012; Vandrey et al., 2012). Smoking as a joint or in a water-pipe were the most common modes of synthetic cannabimimetics administration, while oral consumption as herbal tea was uncommon. The products were obtained from retail vendors such as head shops or gas stations/convenience stores, via the internet or from friends and/or relatives (Vandrey et al., 2012). Data from an anonymous internet-based survey conducted at the beginning of 2011 on 168 respondents demonstrated that the mean number of days of Spice use in the previous year was 67. A subset of respondents endorsed regular use, with 55 and 39% reporting use in the past month and past week, respectively. The mean number of uses per day was four. During an average episode approximately 1 g of product (or 4.5 ‘hits’) was consumed, and the maximum amount consumed in a single episode was reported to be 1.5 g (7.6 ‘hits’). The average duration of subjective intoxication lasted 93 min, while the greatest one lasted 170 min (Vandrey et al., 2012). According to recent users self-reports, synthetic cannabimimetics have a shorter time until peak and shorter duration of action when compared with natural cannabis (Winstock and Barratt, 2013). 512 J. B. Zawilska and J. Wojcieszak Almost all recent synthetic cannabimimetics users admitted to having used natural cannabis. The vast majority of them also consumed alcohol (90.5% of the users in the previous month), tobacco (67.9%) and energy drinks (61.4%). Some of them reported consumption of other psychoactive compounds, mainly MDMA (26.2% in the previous month), benzodiazepines (18.5%), cocaine (14.8%), LSD and hallucinogenic mushrooms (around 12%). Among respondents who recently used both cannabis and synthetic cannabimimetics, almost 80% reported far more frequent use of the former (Winstock and Barratt, 2013). Although data collected from online surveys broaden our knowledge on the use of synthetic cannabimimetics as well as their desired and unwanted effects (see below), they should be interpreted with caution due to several methodological limitations. The most significant limitations include: (1) groups are not representative of the general population (e.g. students from one university, people having access to the internet, willing to complete a survey without compensation), (2) surveys are retrospective, so the data are subject to recall bias, (3) respondents are not certain of the chemical compounds actually contained in the Spice-type products and (4) high levels of poly-drug use and confounding effects from other compounds. Analysis To our knowledge, at present neither synthetic cannabimimetics nor their metabolites can be detected by standard and extended drug tests. Since various synthetic cannabimimetics are controlled in several countries, including Austria, Australia, Belgium, Canada, Denmark, Estonia, Finland, France, Italy, Japan, Latvia, Lithuania, Poland, Romania, Russia, Spain, South Korea, Sweden and the USA (UNODC, 2010; EMCDDA, 2011; National Conference of State Legislatures, 2012), great effort has recently been given to developing testing strategies capable of identifying and quantifying these compounds and their downstream metabolites in suspected products and human biological samples (blood, serum, urine, oral fluids and hair). The applied analytical methods include liquid chromatography tandem mass spectrometry (LC-MS/MS), gas chromatography-mass spectrometry (GC-MS), high mass resolution techniques like matrixassisted laser desorption/ionization-time of flight mass spectrometry (MALDI-TOF) and direct analysis in real time mass spectrometry (DART-MS) (Dresen et al., 2010, 2011; Hudson et al., 2010; Sobolevsky et al., 2010; Teske et al., 2010; Uchiyama et al., 2010, 2011a; Chimalakonda et al., 2011a, b, 2012; Coulter et al., 2011; ElSohly et al., 2011; Grigoryev et al., 2011, 2012, 2013; Möller et al., 2011; Moran et al., 2011; Gottardo et al., 2012; Hutter et al., 2012a, b; Kneisel and Auwäter, 2012; Musah et al., 2012; Denooz et al., 2013; Kavanagh et al., 2013). However, these analytic methods are currently limited to a few laboratories. It has to be emphasized that even with the aid of these highly sophisticated analytical methods, the ever-changing composition of the Spice-type products and their complex metabolism combined with the very limited available information on the chromatographic characteristics and spectral features of the newest compounds and their metabolites, create a major obstacle to effective detection of cannabimimetics, especially in biological samples (Favretto et al., 2013). Synthetic cannabimimetics – mode of action, biodisposition and metabolism Cannabinoids exert their biological effects primarily by interacting with specific membrane bound G proteincoupled cannabinoid receptors, termed CB1 and CB2. Both cannabinoid receptors inhibit adenylyl cyclase and activate a mitogen-activated protein kinase (MAP) cascade by interacting with Gi/o-subtype of G proteins. The CB1 receptor can also activate an A-type and inwardly rectifying potassium channel and inhibit N- and P/ Q-type calcium channels. In addition, the CB1 receptor can be coupled to the Gs protein (Pertwee et al., 2010). Accumulating experimental evidence indicate that the actions of cannabinoids are not restricted to the CB1 and CB2 receptors. Other postulated molecular targets for cannabinoids include additional GPCR (e.g. opioid receptors, muscarinic acetylcholine receptors and the GPR55 receptor), transient receptor potential cation channel receptors, such as transient receptor potential cation channel vanilloid receptors (TRPV), and nuclear perixisome proliferation-activated receptors (PPAR) (Pertwee et al., 2010). Activation of CB1 receptors by endocannabinoids occurs mainly via a retrograde signaling process. CB1 receptors are found on the axon terminals of neurons, where they usually mediate the inhibition of neurotransmitters release (Lovinger, 2008). They are abundantly expressed in brain regions associated with cognition, memory, reward, anxiety, pain sensory perception, food intake, body temperature and motor coordination, such as the cerebral cortex, hippocampus, basal ganglia, cerebellum and hypothalamus. In addition to the central nervous system (CNS), CB1 receptors are also expressed in the peripheral nervous system, both on sensory nerve fibres and in the autonomic nervous system. CB2 receptors are located predominantly in multiple lymphoid organs, such as the spleen, tonsils, thymus and lymphoid nodes, as well as immune cells, including lymphocytes, macrophages, microglia, mast cells and natural killing cells. It has been shown that the psychoactive effects of Δ9-THC are mediated through CB1 receptors in the brain (Howlett et al., 2002). At present, little is known about the detailed pharmacology and toxicology of synthetic cannabimimetics, and no systematic studies on humans have been published. It is widely known that most Spice drugs are endowed Synthetic cannabimimetics as drugs of abuse 513 with potent cannabimimetic activity. Table 1 presents synthetic cannabimimetics with defined receptor profiles most commonly detected in products and biological samples. Behavioural studies performed on animals demonstrate that synthetic cannabimimetics are potent agonists of CB1 and CB2 receptors. CP-47,497 and JWH-018 given intraperitoneally to rats suppressed spontaneous locomotor activity for longer duration and more potently than Δ9-THC (Uchiyama et al., 2012). Nasal exposure of mice to smoke from ‘Buzz’ (containing 2.7 mg JWH-018) resulted in a dose-dependent antinociception, hypothermia, catalepsy and reduced spontaneous locomotor activity (Wiebelhaus et al., 2012). Δ9-THC-like discriminative stimulus effects were observed in mice after administration of JWH-204, JWH-205, JWH-018 and JWH-073 (Vann et al., 2009; Brents et al., 2013), and in monkeys treated with JWH-018 and JWH-073 (Ginsburg et al., 2012). By analogy to Δ9-THC, JWH-018 and JWH-073 dose-dependently attenuated the withdrawal symptoms produced by rimonabant, a CB1 receptor antagonist (Ginsburg et al., 2012). Chronic exposure of mice to JWH-015, a CB2-selective agonist, has been associated with increased vulnerability to drug abuse and depression (Onaivi et al., 2008), while systemic, intranasal administration of another CB2-selective cannabimimetic compound, JWH-133, or its direct injection to the nucleus accumbens, dose-dependently inhibited intravenous cocaine self-administration, cocaine-enhanced locomotion and cocaine-enhanced extracellular dopamine level in the nucleus accumbens (Xi et al., 2011). In electrophysiological studies CP-47,497 and JWH-018 increased the EEG power spectra in the frequency range of 5.0–6.0 Hz, while Δ9-THC decreased the power spectra in the wide range of 7.0–20.0 Hz (Uchiyama et al., 2012). As prolonged cannabis use is associated with immune suppression (Klein and Cabral, 2006; Grotenhermen, 2007), it can be anticipated that the long-term use of Spice drugs containing synthetic cannabimimetics with affinity for CB2 receptors (Huffman, 2009; Uchiyama et al., 2011b: Rajasekaran et al., 2013; see Table 1) may also affect the function of the immune system. The very recent paper by Lewis et al. (2012) demonstrated that both short- and long-term administration to male rats of HU-210 had negative effects on spermatogenesis, being associated with decreased sperm production and a reduced number of Sertoli cells, as well as fragmentation of sperm DNA and reduction in sperm motility. Whether recreational use of synthetic cannabimimetics might affect the fertility of man remains to be elucidated. Our knowledge on the tissue distribution and metabolism of inhaled synthetic cannabimimetics is, at present, limited. Wiebelhaus et al. (2012) analysed biodisposition of JWH-018 in mice exposed (a nose-only exposure) to smoke from 50 mg of the herbal product called ‘Buzz’ containing 5.4% of JWH-018, and found significant JWH-018 levels in blood, brain, heart, lung, liver, kidney and spleen. Furthermore, mice exposed to 20 mg of ‘Buzz’ demonstrated elevated levels of JWH-018 in the heart and lungs. The highest concentrations of JWH-018 were found in tissues associated with absorption (lung), metabolism (liver) and elimination (kidney), while the lowest were found in blood. In another study mice were exposed to smoke from 50 mg ‘Magic Gold’ containing 3.6% JWH-018 and 5.7% JWH-073 and the time course of disposition of these two cannabimimetics in the blood and the brain was evaluated. Concentrations of JWH-018 and JWH-073 increased quickly. Twenty minutes after exposure the mean blood concentration was 88 ng/ml for JWH-018 and 134 ng/ml for JWH-073. At the same time the mean brain concentration was 317 ng/g and 584 ng/g, for JWH-018 and JWH-073, respectively. Within 20 h, blood and brain concentrations of both compounds dropped to very low or undetectable levels (Poklis et al., 2012). Data from animal studies are in accordance with the results published by Teske et al. (2010). In two human subjects who consumed a dose of c.50 μg/kg body mass JWH-018 by smoking, the maximum blood concentrations of the drug were in the range of 10 ng/ml 5 min post-inhalation. Within 3 h, the serum level rapidly dropped, and after 24 h merely trace findings were present. It might be expected that the time course of synthetic cannabimimetics action is similar to that of cannabis, as following inhalation, maximum plasma concentration of Δ9-THC was found to occur within minutes after inhalation, its psychotropic effects start within seconds to a few minutes, reach a maximum after 15–30 min and cease within 2–3 h (Grotenhermen, 2003). It is suggested that both phase I (oxidation, and to a lower extent, carboxylation) and phase II (conjugation with glucuronic acid) processes are involved in the metabolism of synthetic cannabimimetics (Sobolevsky et al., 2010; Wintermeyer et al., 2010; Chimalakonda et al., 2011a; Moran et al., 2011). Final metabolites are predominantly excreted with urine (Gronewold and Skopp, 2011). Monohydroxylation is the major metabolic pathway of compounds containing in their structure the indole ring, such as naphtoylindoles, phenacetylindoles and benzoylindoles. For some of them, metabolites with carboxylated alkyl chains were also identified (Hutter et al., 2012a). It was demonstrated that JWH-018 is metabolized to at least nine monohydroxylated metabolites and one primary carboxy metabolite (Brents et al., 2011). Kinetic studies identified CYP2C9 and CYP1A2 as major isoenzymes involved in the oxidation of JWH-018 and AM-2201 (Chimalakonda et al., 2012), whereas UGT1A1, UGT1A3, UGT1A9, UGT1A10 and UGT2B7 were the major UDP-glucuronosyltransferases responsible for conjugation of hydroxylated metabolites of JWH-018 and JWH-073 (Chimalakonda et al., 2011a). Very recently, it was demonstrated that typical metabolites of JWH-018 and JWH-073 are formed in humans after AM-2201 consumption (Hutter et al., 2013), making a correct identification of synthetic cannabimimetics 514 Substance Chemical name CB1 Ki (nM) CB2 Ki (nM) References Δ9-tetrahydro-cannabinol (Δ9-THC) AM-694 (6aR,10aR)-6,6,9-trimethyl-3-pentyl-6a,7,8,10a-tetrahydro-6H-benzo[c]chromen-1-ol 40.7 36.4 (Showalter et al., 1996) [1-(5-fluoropentyl)-1H-indol-3-yl](2-iodophenyl)-methanone 0.08 1.44 AM-1220 [1-(1-methyl-2-piperidinyl)methyl]-1-naphthaleyl-methanone 3.88 73.4 AM-2201 [1-(5-fluoropentyl)-1H-indol-3-yl]-1-naphthalenyl-methanone 1.00 2.60 CP 47,497-C8 JWH-007 JWH-015 JWH-018 JWH-019 JWH-073 JWH-081 JWH-122 rel-2-[(1S,3R)-3-hydroxycyclohexyl]-5-(2-methylnonan-2-yl)phenol (2-methyl-1-pentyl-1H-indol-3-yl)-1-naphthalenyl-methanone (2-methyl-1-propyl-1H-indol-3-yl)-1-naphthalenyl-methanone (1-pentyl-1H-indol-3-yl)-1-naphthalenyl-methanone (1-hexyl-1H-indol-3-yl)-1-naphthalenyl-methanone (1-butyl-1H-indol-3-yl)-1-naphthalenyl-methanone (4-methoxy-1-naphthalenyl)(1-pentyl-1H-indol-3-yl)-methanone (4-methyl-1-naphthalenyl)(1-pentyl-1H-indol-3-yl)-methanone 0.83 9.50 383 9.50 9.80 8.90 1.20 0.69 2.90 13.8 2.94 5.55 38.0 12.4 1.20 JWH-133 JWH-175 JWH-200 (WIN 55,225) JWH-203 JWH-210 JWH-250 JWH-251 JWH-303 JWH-369 (+)-WIN 55,212-2 (6aR,10aR)-3-(1,1-dimethylbutyl)-6a,7,10,10a-tetrahydro-6,6,9-trimethyl-6H-dibenzo[b,d]pyran 3-(1-naphthalenylmethyl)-1-pentyl-3H-indole [1-[2-(4-morpholinyl)ethyl]-1H-indol-3-yl]-1-naphthalenyl-methanone 2-(2-chlorophenyl)-1-(1-pentyl-1H-indol-3-yl)-ethanone (4-ethyl-1-naphthalenyl)(1-pentyl-1H-indol-3-yl)-methanone 1-(1-pentyl-1H-indol-3-yl)-2-(2-methoxyphenyl)-ethanone 2-(2methylphenyl)-1-(1-pentyl-1H-indol-3-yl)-ethanone [5-(2-fluorophenyl)-1-pentyl-pyrrol-3-yl]-1-naphthalenyl-methanone [5-(2-chlorophenyl)-1-pentyl-1H-pyrrol-3-yl]-1-naphthalenyl-methanone [(3R)-2,3-dihydro-5-methyl-3-(4-morpholinylmethyl)pyrrolo [1,2,3,4-de]-1,4-benzoxazin-6-yl]-1-naphthalenyl-methanone 677 14.0 42.0 8.00 0.46 11.0 29.0 7.7 7.9 62.3 (Makriyannis and Deng, 2001) (Makriyannis and Deng, 2001) (Makriyannis and Deng, 2001) (Melvin et al., 1993) (Aung et al., 2000) (Aung et al., 2000) (Huffman et al., 1994) (Aung et al., 2000) (Aung et al., 2000) (Aung et al., 2000) (Aung et al., 2000; Huffman et al., 2003) (Huffman et al., 1999) (Huffman et al., 2003) (Huffman et al., 2003) (Huffman et al., 2005) (Huffman et al., 2005) (Huffman et al., 2005) (Huffman et al., 2005) (Huffman et al., 2006) (Huffman et al., 2006) (Showalter et al., 1996) 3.4 6.40 7.00 0.69 33.0 146 3.3 5.2 3.30 J. B. Zawilska and J. Wojcieszak Table 1. Affinities of synthetic cannabimimetics most commonly detected in products and biological samples to cannabinoid CB1 and CB2 receptors Synthetic cannabimimetics as drugs of abuse 515 ingested far more difficult than originally thought. CYP2C9, together with CYP3A4, also play a key role in the metabolism of ∆9-THC by human hepatic microsomes (Watanabe et al., 2007). Unlike ∆9-THC metabolites, metabolites of synthetic cannabimimetics retain varying amounts of biologic activity, and can act as full agonists, partial agonists, neutral antagonists or inverse agonists of cannabinoid receptors. Thus, for example, some of the hydroxylated metabolites of JWH-018 and JWH-073 have been demonstrated to bind to CB1 and CB2 receptors with high or intermediate affinity, and potently stimulate G-proteins (Brents et al., 2011, 2012; Rajasekaran et al., 2013). Furthermore, one of them, M1, produced a marked depression of locomotor activity and core body temperature in mice that were blocked by CB1 receptor-preferring antagonists (Brents et al., 2011, 2012). Effects of synthetic cannabimimetics in humans The consumption of cannabis leads to numerous effects within the CNS and peripheral organs. Their spectrum, severity and duration heavily depend on the dose, the individual threshold of the user and psychobiological factors. The most commonly reported CNS effects include feeling of euphoria, relaxation, changes in sensory perception, especially with regard to visual stimuli, altered perception of time, transient hallucination, anxiolysis, sedation, disturbances of short-term memory, lack of coordination and reduction in psychomotor activity. Panic reactions, that occur most often in naïve users or at high doses, and psychotic symptoms have also been described. Physical effects include vasodilation, hyposalivation and dry mouth, decreased respiratory rate and relaxation of muscles (Grotenhermen, 2007). Δ9-THC exerts complex cardiovascular effects in humans. It produces a rapid increase in the heart rate (with a peak occurring 10–30 min after the onset of smoking) that may be accompanied by a modest increase in blood pressure. Marijuana smoking has also been demonstrated to evoke orthostatic hypotension and a chronic use of cannabis may elicit a long lasting decrease in the heart rate and blood pressure (Malinowska et al., 2012). On the contrary, synthetic cannabimimetics have been consistently shown to increase blood pressure (see below). The most frequent side effects observed during clinical trials of Sativex® (multiple sclerosis medication containing cannabis extract) were: fatigue (11.4%), nausea (10.2%), dry mouth (7.8%), application site pain (7.8%), oral pain (6.6%), diarrhea (6%), abnormal taste (4.2%), pharyngitis (3.6%), increased appetite (3.6%), weakness (3.6%), vertigo (3%), mouth ulceration (3%), fall (3%), lethargy (3%), thirst (3%), vomiting (2.4%), cough (2.4%) and sensation of heaviness (2.4%). The main intoxication type reactions included: dizziness (41.6%), somnolence (8.4%), feeling drunk (7.2%), disturbance in attention (6.6%), euphoric mood (5.4%), disorientation (4.8%) and dissociation (3%) (Sativex monograph). Human users of synthetic cannabimimetics report that these products share some but not all of the ‘subjective’ effects of cannabis (Vardakou et al., 2010; Schneir et al., 2011). After smoking a cigarette containing CP 47,497 (Auwärter et al., 2009) or JWH-018 (Teske et al., 2010), healthy volunteers reported sickness, sedation, xerostomia, hot flushes, burning eyes and deterioration of mood and perception. Results from a large anonymous survey indicate that synthetic cannabimimetics produce more negative effects, including hangover and paranoia, than natural cannabis (Winstock and Barratt, 2013). In line with this, emerging evidence accumulated mainly during the last two years shows a wide range of harmful responses to Spice, including hallucinations, psychoses with delusions, agitation, aggressive behaviour, anxiety, panic attacks, seizures, short-term memory deficits, hypertension, acute myocardial infarction, acute kidney injury and respiratory depression (Auwärter et al., 2009; Müller et al., 2010a, b; Vardakou et al., 2010; Vearrier and Osterhoudt, 2010; Benford and Caplan, 2011; Every-Palmer, 2011; Hurst et al., 2011; Lapoint et al., 2011; Mir et al., 2011; Schneir et al., 2011; Simmons et al., 2011; Bebarta et al., 2012; Faircloth et al., 2012; Heath et al., 2012; Hermanns-Clausen et al., 2012, 2013; Jinwala and Gupta, 2012; Pant et al., 2012; Peglow et al., 2012; Schneir and Baumbacher, 2012; Thomas et al., 2012; Tung et al., 2012; Young et al., 2012; Alhadi et al., 2013; Berry-Cabán et al., 2013; Bhanushali et al., 2013; CDC, 2013; Harris and Brown, 2013; McQuade et al., 2013). Treatment of Spice-induced intoxication is mainly supportive, and consists of intravenous application of fluids and, additionally, depending on the type and severity of symptoms, benzodiazepines, non-benzodiazepine sedatives and antipsychotic drugs. Most symptoms resolved themselves within several hours. Case reports of adverse effects of synthetic cannabimimetics are listed in Table 2. According to data from the US National Poison Data Center, collected in 2010 (1898 cases), the most frequently reported adverse effects of synthetic cannabimimetics use were: tachycardia (40%) and hypertension (8.1%), agitation/irritability (23.4%), drowsiness/lethargy (13.5%), confusion (12%), hallucinations or delusions (9.4%) and dizziness (7.3%). Two patients developed status epilepticus (Hoyte et al., 2012). Similar results were obtained by the New Zealand National Poisons Centre (Schep et al., 2011). An analysis of 29 clinical reports on analytically confirmed intoxication with synthetic cannabimimetics selected from the database of the Poisons Information Centre Freiburg, Germany, has shown that the most common adverse effects were symptoms associated with (1) the cardiovascular system, i.e. tachycardia (76%), hypertension (34%), dyspnea (21%) and thoracic pain (10%), (2) the CNS, i.e. restlessness/agitation (41%), changes in perception/hallucinations (38%), vertigo (24%), anxiousness/panic attack (21%), somnolence Male, 25 Male, 21 Symptoms Compound identified Comments References Reddened conjunctivae, increase in pulse rate, xerostomia, alteration in mood and perception. Symptoms lasted up to 6 h. Increased anxiety over the previous month. Paranoid hallucinations, paranoid delusions. Serum samples positive for homolog of CP 47,497. Self-experiment conducted by two of the authors who smoked one cigarette containing 0.3 g of ‘Spice diamond’. Recurrent psychotic episodes for 7 years, long-lasting cannabis use, smoking of ‘Spice’ prior to admission to a hospital. Patient suffered from ADHD. Anxiety resolved after lorazepam. (Auwärter et al., 2009) Female, 20 Panic attacks (for 2 h), irritability, anxiety, fear, blurred vision, unsteady gait, weakness, diaphoresis, palpitations, tachycardia. Visual hallucinations, anxiety, mild increase in blood pressure (135/85 mm Hg), tachycardia (120 beats/ min), occasional muscle fasciculations, mild hypokalemia (2.9 mEq/l). Anxiety. Female, 22 Anxiety, palpitations, tachycardia (126 beats/min). Male, 19 Male, 25 Generalized 1–2 min convulsion while smoking ‘Happy Tiger Incense’. On admission to ED: blood pressure 177/82 mm Hg, heart rate 84 beats/min. Severe anxiety, paranoia, halting speech, avoidance of eye contact, tachycardia, diaphoresis. Generalized seizures, temperature of 37.7 °C, CPK 2649 U/l, mild sinus tachycardia. Tachycardia, acidosis, unresponsiveness. Male, 21 Hypertension, agitation, unresponsiveness. Male, 19 Paranoia, delusions Male, 19 Female, 19 Male, 23 Paranoia, agitation, visual hallucinations. Agitation, sedation, amnesia. Delusions, paranoia. Patient complained of ‘monsters on his back’. Visual hallucinations, chest pain, ‘pounding on chest’, dyspnea on exertion. Initial tachycardia (140 beat/ min) progressed into sinus bradycardia (48 beats/min) with episodes of functional bradycardia at 30 to 40 beats/min. Female, 17 Male, 20 Male, 48 Male, 17 Screening for cannabis (urine, hair) and other drugs (urine) – negative. Identification not conducted. Identification not conducted. JWH-018 and JWH-073 identified in the smoked product. JWH-018 and JWH-073 identified in the smoked product JWH-018, JWH-081, JWH-250 and AM-2201 identified in the smoked product. THC not detected in urine sample. JWH-018 in the ingested powder, JWH-018 metabolite in urine sample. Urine sample positive for JWH-018 metabolite. Urine sample positive for JWH-018 and JWH-073 metabolites. Urine sample positive for JWH-018 and JWH-073 metabolites. Screening of urine sample – negative. Levorphanol in urine sample. Screening of urine sample – negative. JWH-018 and JWH-073 identified in the smoked K9 product. Symptoms resolved 2 h after administration of lorazepam. (Müller et al., 2010b) (Müller et al., 2010a) (Vearrier and Osterhoudt, 2010) (Schneir et al., 2011) (Schneir and Baumbacher, 2012) Patient admitted to smoking ‘Spice’. (Benford and Caplan, 2011) Consumption of an alcohol mixture containing white powder 30 min before seizures. Patient admitted smoking a ‘Spice’ product. Symptoms resolved with benzodiazepines and iv fluids. Symptoms resolved with iv fluids. (Lapoint et al., 2011) Patient was brought to ED 1 h after smoking a ‘Spice’ product. Smoking the ‘Space’ brand of Spice. Smoking the ‘Space’ brand of Spice. (Simmons et al., 2011) (Bebarta et al., 2012) (Young et al., 2012) J. B. Zawilska and J. Wojcieszak Gender, age 516 Table 2. Case reports on the adverse effects of synthetic cannabimimetics Male, 17 Male, 59 Male, 36 Male, 16 Male, 16 Male, 16 Male, 17 Male, 20 Male, 48 Male, 22 Identification not conducted. Patient admitted to smoking K2. (Faircloth et al., 2012) Identification not conducted. Patient admitted to smoking ‘Spice’. (Peglow et al., 2012) Identification not conducted. Mental disturbances after 4 weeks of daily K2 use (Tung et al., 2012) Identification not conducted. Patient admitted to using K2. (Mir et al., 2011) Urine sample negative for cannabis and cocaine. Patient admitted to smoking K2. Urine sample positive for THC. Patient admitted to using K2. Identification not conducted. Patient admitted to smoking K2 an hour prior to admission. Identification not conducted. Patient admitted to smoking K2 an hour prior to admission. Identification not conducted. Symptoms appeared after smoking K2. (Thomas et al., 2012) Urine sample positive for JWH-018 metabolite. Patient confirmed drinking vodka the night before and smoking 3 g of ‘Spice’ before work. (Pant et al., 2012) Identification not conducted. Patient admitted to long-term regular use of Spice. His negative symptoms, disorganized behaviour and speech persisted despite abstinence from Spice for 2 months. (Berry-Cabán et al., 2013) (Heath et al., 2012) Synthetic cannabimimetics as drugs of abuse 517 Male, 15 Dizziness, confusion, emesis (multiple episodes), blood pressure 158/86 mm Hg, sinus tachycardia (132 beats/ min), mild hypokalemia. Three admissions to the hospital due to psychotic symptoms (vivid visual hallucinations and disorganized, bizarre behaviour). Restless, agitation, irritation, irrelevant speech that persisted for 2 wk. At admission to a hospital blood pressure of 150/90 mm Hg, heart rate – 95 beats/min, profuse sweating. Patient presented with a 3 d history of midsternal chest pain. EEG revealed ST-segment elevation in the inferolateral leads; increased troponin level (initially 3 ng/ml, then 25 ng/ml). Diagnosis: acute myocardial infarction. Patient presented with a 1-week history of chest pain, described as approx. 30-min episodes of ‘soreness’. EEG revealed ST-segment elevation in the inferolateral leads; increased troponin level (11.6 ng/ ml). Diagnosis: acute myocardial infarction. Patient presented with a 3 d history of retrosternal and episodic chest pain, lasting for 1–2 h at a time. EEG revealed ST-segment elevation; increased troponin level (initially 7 ng/ml, then 12 ng/ml). Diagnosis: acute myocardial infarction. Faint, generalized muscular tone in extremities, cyanosis, apnea, ocular redness, swelling. Tachycardia (initially 180 beats/min, after 6 mg iv adenosine decreased to 140 beats/min). At the hospital – confused speech, somnolence, complaints of chest and back pain. Lost of consciousness. On admission – sinus tachycardia (172 beats/min), blood pressure of 162/57 mm Hg. Amnesia, mild headache, fatigue. Agitation, confusion, suicidal ideation, self-inflicted trauma, sinus tachycardia. Generalized tonic-clonic seizures. Sinus tachycardia (106 beats/min), blood pressure 140/80 mm Hg, temperature 37.7 °C, myadriasis, diaphoresis, increased creatine phosphokinase level to 1200 U/l Agitation, aggression, attention impairment consistent with delirium, tachycardia (160 beats/min). On the seventh hospital day the patient developed acute psychosis with delusions. 518 Table 2. (cont.) Symptoms Compound identified Comments References Female, 19 Seizure, agitation, altered mental status, blood pressure 153/84 mm Hg, pulse 116 beats/min. The patient was somnolent, hyperreflexic, and periodically repeated ‘Is this real?’ Agitation, dangerous behaviour described as ‘running in and out of traffic’, myoclonic jerking, hallucinations. At admission: sinus tachycardia (134 beats/min), blood pressure 144/68 mm Hg, flushed skin, dilated pupils, hyperflexia without clonus , occasional jerking of the limbs, inappropriate laughter and silence when asked questions. Anxiety, mild hyperreflexia, tachycardia (130 beats/ min). The patient complained of inability to move his limbs. Seizure-like activity, cyanosis, unresponsiveness. Initial pulse 220 beats/min, at admission to a hospital – 180 beats/min. Chest pain, nausea, vomiting, syncope, pulse 95 beats/ min. Mild agitation, hallucinations, pulse at admission to a hospital 104 beats/min. Urine sample negative for cannabis and other drugs of abuse Patient was smoking ‘Bayou Blaster®’ when seizures started. (Harris and Brown, 2013) Urine sample negative for cannabis and other drugs of abuse. Patient was smoking ‘Humboldt Gold’ when symptoms started. He described being in multiple dreams that he could not get out. Identification not conducted. Patient admitted to smoking ‘Space’ several minutes before symptoms occurred. Urine sample positive for THC. Patient admitted to smoking K2 approx. 20 min before symptoms occurred. Identification not conducted. Patient admitted smoking 3 g of K2. Identification not conducted. Nausea and vomiting, flank pain. Diagnosed: acute kidney injury. Nausea and vomiting. Diagnosed: acute kidney injury. Product: XLR-11. Urine: N-pentanoic acid metabolite of XLR-11 Blood: N-pentanoic acid metabolite of XLR-11. Product: XLR-11 and UR-144. Serum: XLR-11; UR-144, N-pentanoic acid metabolite of XLR-11. Product: XLR-11. Patient admitted to smoking K2 herbal for the first time and complained of being in a dream state that he could not get out. Symptoms appeared 2 d after smoking the product. Symptoms appeared 2 d after smoking ‘Phantom Wicked Dreams’. Patient used ‘Mr. Happy’. Male, 17 Male, 17 Male, 19 Male, 24 Male, 22 Male, 18 Male, 30 Male, 26 Nausea and vomiting, abdominal pain/back pain. Diagnosed: acute kidney injury. Male, 17 Nausea and vomiting, flank pain. Diagnosed: acute kidney injury. Nausea and vomiting, abdominal pain. Diagnosed: acute kidney injury. Nausea and vomiting, abdominal pain. Diagnosed: acute kidney injury. Nausea and vomiting, abdominal pain. Diagnosed: acute kidney injury. Male, 18 Male, 18 Male, 15 Symptoms appeared 9 d after smoking ‘Clown Royal’. Symptoms appeared 2 d after smoking ‘Lava’. Product: XLR-11. Urine: N-pentanoic acid metabolite of XLR-11. Not detected Symptoms appeared 2 d after smoking ‘Lava’. Identification not conducted. Patient admitted to smoking ‘Flame 2.0’. (Centers for Disease Control and Prevention, 2013) J. B. Zawilska and J. Wojcieszak Gender, age Male, 20 Male, 23 Male, 26 Male, 30 Male, 17 Male, 17 Male, 20 Male, 19 Male, 21 Male, 20 Identification not conducted. Patient admitted to using Spice for few weeks. (Bhanushali et al., 2013) Identification not conducted. Identification not conducted. Identification not conducted. Blood: MAM-2201, UR-144. Urine: metabolites of JWH-122, UR-144 and JWH-018. Blood: JWH-081. Urine: metabolites of JWH-081, JWH-018 and JWH-073. Patient admitted to using Spice over the last two years. Patient admitted to using Spice over the last year. Patient smoked an herbal mixture ordered via the Internet, assuming that it contained ‘salvia divinorum’. Few minutes after smoking the herbal mixture ‘Jamaican Gold’. patient felt nauseous. Blood: JWH-122. Urine: Metabolites of JWH-122 and JWH-018. Patient smoked the herbal mixture ‘Lava Red’ Blood: JWH-122, JWH-210, JWH-018. Urine: Metabolites of JWH-122, JWH-210, JWH-018, Δ9-THC. Blood: AM-2201, JWH-122, JWH-210. Urine: metabolites of JWH-018 and AM-2201. Patient smoked ‘Bonzai’ two times: in the evening and in the morning. Seizures developed after the second consumption. Patient smoked several Spice products for the last 4 months. Urine: metabolites of AM-2201 Before convulsion patient smoked a ‘Black Mamba’ Spice product. (Hermanns-Clausen et al., 2013) (Alhadi et al., 2013) (McQuade et al., 2013) Synthetic cannabimimetics as drugs of abuse 519 Nausea and vomiting for 2 d. Diagnosed: oliguric acute kidney injury Nausea and vomiting for 2 d. Diagnosed: oliguric acute kidney injury Nausea, vomiting, diarrhea and lower abdominal pain for 2 d. Diagnosed: oliguric acute kidney injury. Nausea, vomiting, diarrhea and lower abdominal pain for 3 d. Diagnosed: acute kidney injury. Sinus tachycardia (160 beats/min), mydriasis, anisocoria, retrograde amnesia, mild somnolence, leukocytosis. Agitation, laugh attacks, panic attacks, massive vomiting, myoclonig jerking, sinus tachycardia (112 beats/min), confusion, somnolence, hypokalemia. Massive vomiting, pale skin, mydriasis, mild tachycardia (100 beats/min), somnolence, mild hypokalemia, leukocytosis, elevation of creatine kinase. Tonic-clinic seizures, repetitive vomiting, no sufficient respiration. The next day: elevated levels of creatine kinase, leukocytosis, trombolysis. Dyspnea, 2-month history of chronic cough, occasional hemoptysis, two episodes of syncope. Chest imaging revealed diffuse, bilateral, subacute lung infiltrates. Suspected: hypersensitivity pneumonitis. Generalized tonic-clonic convulsion lasting for appr. 2–3 min, drowsiness, dry skin. 520 J. B. Zawilska and J. Wojcieszak (17%), confusion, disorientation (14%), (3) the gastrointestinal system, i.e. nausea/vomiting (28%) and dry mouth/ globus sensation (14%) and (4) the eyes – mydriasis (38%) and conjuctive hyperaemia (14%) (Hermanns-Clausen et al., 2012). It should be noted that data collected from Poison Centres reports may not be representative of all synthetic cannabimimetics intoxications. The reported cases are likely to have more severe symptoms than nonreported ones. Furthermore, exposure history and substance/product responsible for the symptoms are mainly based on reports coming from individuals with no or limited qualified knowledge in the field, such as patients, relatives and bystanders (e.g. Hermanns-Clausen et al., 2012; Hoyte et al., 2012). To our knowledge there is only one published report of death following use of a synthetic cannabinoid. The decedent was a 23-year old male, with many blunt and sharp force wounds; the fatal wound was a self-inflicted stab wound to the neck. AM-2201 and its metabolites were found in his blood (Patton et al., 2013). A recent report of Musshoff et al. (2013) presents seven cases of driving under the influence of synthetic cannabimimetics, where the presence of the following compounds was analytically confirmed in sera taken from a total of eight subjects involved: AM-2201(two persons), JWH-018 (three persons), JWH-019 (one person), JWH-122 (five persons), JWH-210 (four persons), JWH-307 (one person). As the physical examination of the subjects revealed a delayed reaction of pupils to light, blurred speech, dizziness, unstable appearance and retarded sequence of movements, it is assumed that the consumptions of synthetic cannabimimetics, like cannabis use (Hartman and Huestis, 2013), can lead to a potentially dangerous impairment of driving skills and cognitive deficits. It is estimated that around 9% of cannabis users develop dependence with a withdrawal response that occurs upon cessation of drug administration. The most common symptoms of cannabis withdrawal are anger, irritability, depressed mood, anxiety, decreased appetite and weight loss, restlessness, disturbances in sleep onset and maintenance and cannabis craving. Symptoms do not occur until about 24 h after the last use, peak in 2–3 d and last about 2–3 wk (Cooper and Haney, 2008; Danovitch and Gorelick, 2012). To our knowledge, there are only three published reports of dependence on synthetic cannabimimetics. Zimmermann et al. (2009) presented the case of a 20 yr-old patient who had developed a tolerance to ‘Spice Gold’. During the abstinence period he suffered from a physical dependence syndrome with profound sweating (especially in the night), internal unrest, tremor, insomnia, nightmares, palpitations, headache, diarrhea, nausea, and vomiting. While being treated in hospital for Spice dependence, he displayed increased heart rate and hypertension for several days. Nacca et al. (2013) described two cases of acute withdrawal syndrome in a 22 yr-old woman and a 20 yr-old man, presumably due to prolonged synthetic cannabimimetics use. The syndrome was characterized by sinus tachycardia and severe anxiety in the absence of any abnormal neurologic findings. The patients also complained of headache, insomnia, sweats and chills and, in the woman’s case, cramping pain in arms and legs, vivid dreams and potent anorexia. The symptoms did not improve with marijuana, but resolved with lorazepam or quetiapine. A severe withdrawal syndrome with similar symptoms lasting for 3–4 d and accompanied by significant craving, was reported in the case of a 23 yr-old man who had consumed ‘Spice Gold’, containing JWH-018 and CP 47,497, on a regular basis (Rominger et al., 2013). At the present state of knowledge it appears that the withdrawal syndrome from synthetic cannabimimetics is similar but more severe than that from natural cannabis (Gorelick et al., 2013). Conclusions Although synthetic cannabimimetics were originally synthesized to study the endocannabinoid system, with the aim of developing therapeutically-effective compounds devoid of the unwanted effects of cannabis, several of them have become drugs of abuse. The experience of recent years clearly shows that synthetic cannabimimetics represent a significant potential hazard to human health. As many of these compounds and their metabolites have been found to possess higher binding affinity and higher efficacy at CB receptors than Δ9-THC, it might be expected that both the acute and chronic effects, including the adverse ones, of synthetic cannabimimetics could be intensified when compared to a similar level of exposure to Δ9-THC. None of these substances has been thoroughly tested for negative side effects. The unknown production practices, composition and purity of the Spice-type products, as well as the concentration of active ingredients, are all associated with risks which are hard to define. Accumulating clinical evidence indicates that intoxication with Spice/K2-like products produces symptoms similar to adverse effects after high doses of cannabis. However, some symptoms, such as pronounced agitation, epileptic seizures, hypokalemia and frequently occurring nausea/vomiting seem to be unique to the synthetic cannabimimetics (Hermanns-Clausen et al., 2012). According to expert opinions, the appearance of myoclonic and generalized tonic-clonic seizures, and cases of acute myocardial infarction after the use of synthetic cannabimimetics are particularly worrying. The growing popularity of Spice/ K2-products as recreational drugs highlights the urgent need to further evaluate the effects of synthetic cannabimimetics in vivo in order to: (1) improve our understanding of how these compounds interact with cannabinoid and non-cannabinoid receptors in the brain as well as in peripheral organs and tissues, (2) better characterize Synthetic cannabimimetics as drugs of abuse 521 their pharmacological, toxicological and pharmacokinetic properties, (3) develop drug-specific treatments for intoxication and (4) create effective education and prevention programmes. Acknowledgments Supported by the Medical University of Lodz (503/3-011-01/503-01). Fruitful discussion with José Miguel Honório from the Faculdade de Farmácia, University of Lisbon, is highly appreciated. Statement of Interest None. References Alhadi S, Tiwari A, Vohra R, Gerona R, Acharya J, Bilello K (2013) High times, low sats: diffuse pulmonary infiltrates associated with chronic synthetic cannabinoid use. J Med Toxicol 9:199–206. Atwood BK, Huffman J, Straiker A, Mackie K (2009) JWH018, common constituent of ‘Spice’ herbal blends, is a potent and efficacious cannabinoid CB receptor agonist. Br J Pharmacol 160:585–593. Aung MM, Griffin G, Huffman JW, Wu M, Keel C, Yang B, Showalter VM, Abood ME, Martin BR (2000) Influence of the N-1 alkyl chain length of cannabimimetic indoles upon CB1 and CB2 receptor binding. Drug Alcohol Depend 60:133–140. Auwärter V, Dresen S, Weinmann W, Müller M, Pütz M, Ferreirós N (2009) ‘Spice’ and other herbal blends: harmless incense or cannabinoid designer drugs? J Mass Spectrom 44:832–837. Barratt MJ, Cakic V, Lenton S (2013) Patterns of synthetic cannabinoid use in Australia. Drug Alcohol Rev 32:141–146. Bebarta VS, Ramirez S, Varney SM (2012) Spice: a new ‘legal’ herbal mixture abused by young active duty military personnel. Subst Abus 33:191–194. Benford DM, Caplan JP (2011) Psychiatric sequelae of Spice, K2, and synthetic cannabinoid receptor agonists. Psychosomatics 52:295. Berry-Cabán CS, Ee J, Ingram V, Berry CE, Kim EH (2013) Synthetic cannabinoid overdose in a 20-year-old male US solder. Subst Abuse 1:70–72. Bhanushali GK, Jain G, Fatima H, Leisch LJ, Thornley-Brown D (2013) AKI associated with synthetic cannabinoids: a case series. Clin J Am Soc Nephrol 8:523–526. Brents LK, Reichard EE, Zimmerman SM, Moran JH, Fantegrossi WE, Prather PL (2011) Phase I hydroxylated metabolites of the K2 synthetic cannabinoid JWH-018 retain in vitro and in vivo cannabinoid 1 receptor affinity and activity. PLoS ONE 6:e21917. doi: 10.1371/journal.pone.0021917. Brents LK, Gallus-Zawada A, Radominska-Pandya A, Vasiljevik T, Prisinzano TE, Fantegrossi WE, Moran JH, Prather PL (2012) Monohydroxylated metabolites of the K2 synthetic cannabinoid JWH-073 retain intermediate to high cannabinoid 1 receptor (CB1R) affinity and exhibit neutral antagonist to partial agonist activity. Biochem Pharmacol 83:952–961. Brents LK, Zimmerman SM, Saffell AR, Prather PL, Fantegrossi WE (2013) Differential drug-drug interactions of the synthetic cannabinoids JWH-018 and JWH-073: implications for drug abuse liability and pain therapy. J Pharmacol Exp Ther 346:350–361. Carroll FI, Lewin AH, Mascarella SW, Seltzman HH, Reddy PA (2012) Designer drugs: a medicinal chemistry perspective. Ann N Y Acad Sci 1248:18–38. CDC (Centers for Disease Control and Prevention) (2013) Acute kidney injury associated with synthetic cannabinoid use – multiple states, 2012. MMWR Morb Mortal Wkly Rep 62:93–98. Chimalakonda KC, Bratton SM, Le VH, Yiew KH, Dineva A, Moran CL, James LP, Moran JH, Radominska-Pandya A (2011a) Conjugation of synthetic cannabinoids JWH-018 and JWH-073, metabolites by human UDP-glucuronosyltransferases. Drug Metab Dispos 39:1967–1976. Chimalakonda KC, Moran CL, Kennedy PD, Endres GW, Uzieblo A, Dobrowolski PJ, Fifer EK, Lapoint J, Nelson LS, Hoffman RS, James LP, Radominska-Pandya A, Moran JH (2011b) Solid-phase extraction and quantitative measurement of omega and omega-1 metabolites of JWH-018 and JWH-073 in human urine. Anal Chem 83:6381–6388. Chimalakonda KC, Seely KA, Bratton SM, Brents LK, Moran CL, Endres GW, James LP, Hollenberg PF, Prather PL, Radominska-Pandya A, Moran JH (2012) Cytochrome P450-mediated oxidative metabolism of abused synthetic cannabinoids found in K2/Spice: identification of novel cannabinoid receptor ligands. Drug Metab Dispos 40:2174–2184. Choi H, Heo S, Choe S, Yang W, Park Y, Kim E, Chung H, Lee J (2013) Simultaneous analysis of synthetic cannabinoids in the materials seized during drug trafficking using GC-MS. Anal Bioanal Chem 405:3937–3944. Cooper ZD, Haney M (2008) Cannabis reinforcement and dependence. Addict Biol 13:188–195. Coulter C, Garnier M, Moore C (2011) Synthetic cannabinoids in oral fluid. J Anal Toxicol 35:424–430. Danovitch I, Gorelick DA (2012) State of art treatments for cannabis dependence. Psychiatr Clin North Am 35:309–326. Dargan PI, Hudson S, Ramsey J, Wood DM (2011) The impact of changes in UK classification of the synthetic cannabinoid receptor agonists in ‘Spice’. Int J Drug Policy 22:274–277. Denooz R, Vanheugen JC, Frederich M, de Tullio P, Charlier C (2013) Identification and structural elucidation of four cannabimimetic compounds (RCS-4, AM-2201, JWH-203 and JWH-210) in seized products. J Anal Toxicol 37:56–63. Dresen S, Ferreirós N, Pütz M, Westphal F, Zimmermann R, Auwärter V (2010) Monitoring of herbal mixtures potentially containing synthetic cannabinoids as psychoactive compounds. J Mass Spectrom 45:1186–1194. Dresen S, Kneisel S, Weinmann W, Zimmermann R, Auwärter V (2011) Development and validation of a liquid chromatography-tandem mass spectrometry method for the quantitation of synthetic cannabinoids of the aminoalkylindole type and methanandamide in serum and its application to forensic samples. J Mass Spectrom 46:163–171. ElSohly MA, Gul W, ElSohly KM, Murphy TP, Madgula VL, Khan SI (2011) Liquid chromatography-tandem mass spectrometry analysis of urine specimens for K2 (JWH-018) metabolites. J Anal Toxicol 35:487–495. 522 J. B. Zawilska and J. Wojcieszak EMCDDA (European Monitoring Centre for Drugs and Drug Addiction) (2009) Understanding the ‘Spice’ phenomenon. Available at: http://www.emcdda.europa.eu/attachements. cfm/att_80086_EN_Spice%20Thematic%20paper%20—% 20final%20version.pdf (accessed 7 October 2013). EMCDDA (European Monitoring Centre for Drugs and Drug Addiction) (2011) Synthetic cannabinoids and ‘Spice’. Available at: http://www.emcdda.europa.eu/publications/ drug-profiles/synthetic-cannabinoids (accessed 15 January 2013). Ernst L, Krüger K, Lindigkeit R, Schiebel HM, Beuerle T (2012) Synthetic cannabinoids in ‘spice-like’ herbal blends: first appearance of JWH-307 and recurrence of JWH-018 on the German market. Forensic Sci Int 222:216–222. Every-Palmer S (2011) Synthetic cannabinoid JWH-018 and psychosis: an explorative study. Drug Alcohol Depend 117:152–157. Faircloth J, Khandheria B, Shum S (2012) Case report: adverse reaction to synthetic marijuana. Am J Addict 21:289–290. Fattore L, Fratta W (2011) Beyond THC: the new generation of cannabinoid designer dugs. Front Behav Neurosci 5:60. Favretto D, Pascali JP, Tagliaro F (2013) New challenges and innovation in forensic toxicology. focus on the ‘New Psychoactive Substances’. J Chromatogr A 1287:84–95. Forrester MB, Kleinschmidt K, Schwarz E, Young A (2012) Synthetic cannabinoid and marijuana exposures reported to poison centers. Hum Exp Toxicol 31:1006–1011. Ginsburg BC, Schulze DR, Hruba L, McMahon LR (2012) JWH-018 and JWH-073: Δ9-tetrahydrocannabinol-like discriminative stimulus effects in monkeys. J Pharmacol Exp Ther 340:37–45. Gorelick DA, Goodwin RS, Schwilke E, Schwope DM, Darwin WD, Kelly DL, McMahon RP, Liu F, Ortemann-Renon C, Bonnet D, Huestis MA (2013) Tolerance to effects of effects of high-dose oral δ9-tetrahydrocannabinol and plasma cannabinoid concentrations in male daily cannabis smokers. J Anal Toxicol 37:11–16. Gottardo R, Chiarini A, Dal Prà I, Seri C, Rimondo C, Serpelloni G, Armato U, Tagliaro F (2012) Direct screening of herbal blends for new synthetic cannabinoids by MALDI-TOF MS. J Mass Spectrom 47:141–146. Grigoryev A, Savchuk S, Melnik A, Moskaleva N, Dzhurko J, Ershov M, Nosyrev A, Vedenin A, Izotov B, Zabirova I, Rozhanets V (2011) Chromatography-mass spectrometry studies on the metabolism of synthetic cannabinoids JWH-018 and JWH-073, psychoactive components of smoking mixtures. J Chromatogr B Analyt Technol Biomed Life Sci 879:1126–1136. Grigoryev A, Kavanagh P, Melnik A (2012) The detection of the urinary metabolites of 3-[(adamantan-1-yl)carbonyl]-1pentylindole (AB-001), a novel cannabimimetic, by gas chromatography-mass spectrometry. Drug Test Anal 4:519–524. Grigoryev A, Kavanagh P, Melnik A (2013) The detection of the urinary metabolites of 1-[(5-fluoropentyl)-1H-indol-3yl]-(2-iodophenyl)methanone (AM-694), a high affinity cannabimimetic, by gas chromatography – mass spectrometry. Drug Test Anal 5:110–115. Gronewold A, Skopp G (2011) A preliminary investigation on the distribution of cannabinoids in man. Forensic Sci Int 210(1–3): e7–e11. Grotenhermen F (2003) Pharmacokinetics and pharmacodynamics of cannabinoids. Clin Pharmacokinet 42:327–360. Grotenhermen F (2007) The toxicology of cannabis and cannabis prohibition. Chem Biodivers 4:1744–1769. Harris CR, Brown A (2013) Synthetic cannabinoid intoxication: a case series and review. J Emerg Med 44:360–366. Hartman RL, Huestis MA (2013) Cannabis effects on driving skills. Clin Chem 59:478–492. Heath TS, Burroughs Z, Thompson AJ, Tecklenburg FW (2012) Acute intoxication caused by a synthetic cannabinoid in two adolescents. J Pediatr Pharmacol Ther 17:177–181. Heltsley R, Shelby MK, Crouch DJ, Black DL, Robert TA, Marshall L, Bender CL, DePriest AZ, Colello MA (2012) Prevalence of synthetic cannabinoids in US athletes: initial findings. J Anal Toxicol 36:588–593. Hermanns-Clausen M, Kneisel S, Szabo B, Auwärter V (2012) Acute toxicity due to the confirmed consumption of synthetic cannabinoids: clinical and laboratory findings. Addiction 108:534–544. Hermanns-Clausen M, Kneisel S, Hutter M, Szabo B, Auwärter V (2013) Acute intoxication by synthetic cannabinoids – four case reports. Drug Test Anal. doi: 10.1002/dta.1483. Howlett AC, Barth F, Bonner TI, Cabral G, Casellas P, Devane WA, Felder CC, Herkenham M, Mackie K, Martin BR, Mechoulam R, Pertwee RG (2002) International Union of Pharmacology. XXVII. Classification of cannabinoid receptors. Pharmacol Rev 54:161–202. Hoyte CO, Jacob J, Monte AA, Al-Jumaan M, Bronstein AC, Heard KJ (2012) A characterization of synthetic cannabinoid exposures reported to the National Poison Data System in 2010. Ann Emerg Med 60:435–438. Hu X, Primack BA, Barnett TE, Cook RL (2011) College students and use of K2: an emerging drug of abuse in young persons. Subst Abuse Treat Prev Policy 6:16. Hudson S, Ramsey J (2011) The emergence and analysis of synthetic cannabinoids. Drug Test Anal 3:466–478. Hudson S, Ramsey J, King L, Timbers S, Maynard S, Dargan PI, Wood DM (2010) Use of high-resolution accurate mass spectrometry to detect reported and previously unreported cannabinomimetics in ‘herbal high’ products. J Anal Toxicol 34:252–260. Huffman JW (2009) Cannabinomimetic indoles, pyrroles and indenes: structure-activity relationships and receptor interactions. In: The cannabinoid receptors (Regio PH, ed), Vol. 1, pp49–94. New York: Humana Press. Huffman JW, Dai D, Martin BR (1994) Design, synthesis and pharmacology of cannabinomimetic indoles. Bioorg Med Chem Lett 4:563–566. Huffman JW, Liddle J, Yu S, Aung MM, Abood ME, Wiley JL, Martin BR (1999) 3-(1′,1′-Dimethylbutyl)-1-deoxy-Δ8-THC and related compounds: synthesis of selective ligands for the CB2 receptor. Bioorg Med Chem Lett 7:2905–2914. Huffman JW, Mabon R, Wu MJ, Lu J, Hart R, Hurst DP, Reggio PH, Wiley JL, Martin BR (2003) 3-Indolyl-1-naphthylmethanes: new cannabimimetic indoles provide evidence for aromatic stacking interactions with the CB1 cannabinoid receptor. Bioorg Med Chem 11:539–549. Huffman JW, Szklennik PV, Almond A, Bushell K, Selley DE, He H, Cassidy MP, Wiley JL, Martin BR (2005) 1-Pentyl-3-phenylacetylindoles, a new class of cannabimimetic indoles. Bioorg Med Chem Lett 15:4110–4113. Synthetic cannabimimetics as drugs of abuse 523 Huffman JW, Padgett LW, Isherwood ML, Wiley JL, Martin BR (2006) 1-Alkyl-2-aryl-4-(1-naphthoyl)pyrroles: new high affinity ligands for the cannabinoid CB1 and CB2 receptors. Bioorg Med Chem Lett 16:5432–5435. Hurst D, Loeffler G, McLay R (2011) Psychosis associated with synthetic cannabinoid agonists: a case series. Am J Psychiatry 168:1119. Hutter M, Broecker S, Kneisel S, Auwärter V (2012a) Identification of the major urinary metabolites in man of seven synthetic cannabinoids of the aminoalkylindole type present as adulterants in ‘herbal mixtures’ using LC-MS/MS techniques. J Mass Spectrom 47:54–65. Hutter M, Kneisel S, Auwärter V, Neukamm MA (2012b) Determination of 22 synthetic cannabinoids in human hair by liquid chromatography-tandem mass spectrometry. J Chromatogr B Analyt Technol Biomed Life Sci 903:95–101. Hutter M, Moosmann B, Kneiseel S, Auwärter V (2013) Characterization of the designer drug and synthetic cannabinoid receptor agonist AM-2201 regarding its chemistry and metabolism. J Mass Spectrom 48:885–894. Jinwala FN, Gupta M (2012) Synthetic cannabis and respiratory depression. Child Adolesc Psychopharmacol 22:459–462. Johnson LA, Johnson RL, Portier RB (2013) Current ‘Legal highs’. J Emerg Med 44:1108–1115. Kavanagh P, Grigoryev A, Savchuk S, Mikhura I, Formanovsky A (2013) UR-144 in products sold via the internet: identification of related compounds and characterization of pyrolysis products. Drug Test Anal 5:683–692. Klein TW, Cabral GA (2006) Cannabinoid-induced immune suppression and modulation of antigen-presenting cells. J Neuroimmune Pharmacol 1:50–64. Kneisel S, Auwärter V (2012) Analysis of 30 synthetic cannabinoids in serum by liquid chromatography-electrospray ionization tandem mass spectrometry after liquid-liquid extraction. J Mass Spectrom 47:825–835. Langer N, Lindigkeit R, Schiebel HM, Ernst L, Beuerle T (2013) Identification and quantification of synthetic cannabinoids in ‘spice-like’ herbal mixtures: a snapshot of the German situation in the autumn of 2012. Drug Test Anal. doi: 10.1002/ dta.1499. Lapoint J, James LP, Moran CL, Nelson LS, Hoffman RS, Moran JH (2011) Severe toxicity following synthetic cannabinoid ingestion. Clin Toxicol (Phila) 49:760–764. Lewis SE, Paro R, Borriello L, Simon L, Robinson L, Dincer Z, Riedel G, Battista N, Maccarrone M (2012) Long-term use of HU210 adversely affects spermatogenesis in rats by modulating the endocannabinoid system. Int J Androl 35:731–740. Lindigkeit R, Boehme A, Eiserloh I, Luebbecke M, Wiggermann M, Ernst L, Beuerle T (2009) Spice: a never ending story? Forensic Sci Int 191:58–63. Loeffler G, Hurst D, Penn A, Yung K (2012) Spice, bath salts, and the U.S. military: the emergence of synthetic cannabinoid receptor agonists and cathinones in the U.S. Armed Forces. Mil Med 177:1041–1048. Lovinger DM (2008) Presynaptic modulation by endocannabinoids. Handb Exp Pharmacol 184:435–477. Makriyannis A, Deng H (2001) Cannabinomimetic indole derivatives. WO patent 200128557. Malinowska B, Baranowska-Kuczko M, Schlicker E (2012) Triphasic blood pressure responses to cannabinoids: do we understand the mechanism? Br J Pharmacol 165:2073–2088. McQuade D, Hudson S, Dargan PI, Wood DM (2013) First European case of convulsions related to analytically confirmed use of the synthetic cannabinoid receptor agonist AM-2201. Eur J Clin Pharmacol 69:373–376. Melvin LS, Milne GM, Johnson MR, Subramaniam B, Wilken GH, Howlett AC (1993) Structure-activity relationships for cannabinoid receptor-binding and analgesic activity: studies of bicyclic cannabinoid analogs. Mol Pharmacol 44:1008–1015. Mir A, Obafemi A, Young A, Kane C (2011) Myocardial infarction associated with use of the synthetic cannabinoid K2. Pediatrics 128:e1622–e1627. Möller I, Wintermeyer A, Bender K, Jübner M, Thomas A, Krug O, Schänzer W, Thevis M (2011) Screening for the synthetic cannabinoid JWH-018 and its major metabolites in human doping controls. Drug Test Anal 3:609–620. Moran CL, Le VH, Chimalakonda KC, Smedley AL, Lackey FD, Owen SN, Kennedy PD, Endres GW, Ciske FL, Kramer JB, Kornilov AM, Bratton LD, Dobrowolski PJ, Wessinger WD, Fantegrossi WE, Prather PL, James LP, Radominska-Pandya A, Moran JH (2011) Quantitative measurement of JWH-018 and JWH-073 metabolites excreted in human urine. Anal Chem 83:4228–4236. Musah RA, Domin MA, Walling MA, Shepard JR (2012) Rapid identification of synthetic cannabinoids in herbal samples via direct analysis in real time mass spectrometry. Rapid Commun Mass Spectrom 26:1109–1114. Musshoff F, Madea B, Kernbach-Wighton G, Bicker W, Kneisel S, Hutter M, Auwärter V (2013) Driving under the influence of synthetic cannabinoids (‘Spice’): a case series. Int J Legal Med. doi: 10.1007/s00414-013-0864-1. Müller H, Huttner HB, Köhrmann M, Wielopolski JE, Kornhuber J, Sperling W (2010a) Panic attack after spice abuse in a patient with ADHD. Pharmacopsychiatry 43:152–153. Müller H, Sperling W, Köhrmann M, Huttner HB, Kornhuber J, Maler JM (2010b) The synthetic cannabinoid Spice as a trigger for an acute exacerbation of cannabis induced recurrent psychotic episodes. Schizophr Res 118:309–310. Nacca N, Vatti D, Sullivan R, Sud P, Su M, Maraffa J (2013) The synthetic cannabinoids withdrawal syndrome. J Addict Med 7:296–298. National Conference of State Legislatures (2012). Synthetic Cannabinoids (a.k.a. ‘K2’/’Spice’) Enactments. Available at: http://www.ncsl.org/issues-research/justice/syntheticcannabinoids-enactments.aspx(accessed 7 October 2013). Office of National Drug Control Policy (2011) Monitoring the future study. Highlights. Available at: http://www.whitehouse.gov/sites/default/files/ondcp/Blog/2011_monitoring_ the_future.pdf (accessed 7 October 2013). Onaivi ES, Carpio O, Ishiguro H, Schanz N, Uhl GR, Benno R (2008) Behavioural effects of CB2 cannabinoid receptor activation and its influence on food and alcohol consumption. Ann N Y Acad Sci 1139:426–433. Pant S, Deshmukh A, Dholaria B, Kaur V, Ramavaram S, Ukor M, Teran GA (2012) Spicy seizure. Am J Med Sci 344:67–68. Patton AL, Chimalakonda KC, Moran CL, McCain KR, Radominska-Pandya A, James LP, Kokes C, Moran JH (2013) K2 toxicity: fatal case of psychiatric complocations following AM2201 exposure. J Forensic Sci. doi: 10.1111/ 1556-4029.12216. 524 J. B. Zawilska and J. Wojcieszak Peglow S, Buchner J, Briscoe G (2012) Synthetic cannabinoid induced psychosis in a previously nonpsychotic patient. Am J Addict 21:287–288. Pertwee RG, Howlett AC, Abood ME, Alexander SP, Di Marzo V, Elphick MR, Greasley PJ, Hansen HS, Kunos G, Mackie K, Mechoulam R, Ross RA (2010) International Union of Basic and Clinical Pharmacology. LXXIX. Cannabinoid receptors and their ligands: beyond CB1 and CB2. Pharmacol Rev 62:588–631. Poklis JL, Amira D, Wise LE, Wiebelhaus JM, Haggerty BJ, Poklis A (2012) Detection and disposition of JWH-018 and JWH-073 in mice after exposure to ‘Magic Gold’ smoke. Forensic Sci Int 220:91–96. Rajasekaran M, Brents LK, Franks LN, Moran JH, Prather PL (2013) Human metabolites of synthetic cannabinoids JWH-018 and JWH-073 bind with high affinity and act as potent agonists at cannabinoid type-2 receptors. Toxicol Appl Pharmacol 269:100–108. Rominger A, Cumming P, Xiong G, Koller G, Förster S, Zwergal A, Karamatskos E, Bartenstein P, La Fougère C, Pogarell O (2013) Effects of acute detoxification of the herbal blend ‘Spice Gold’ on dopamine D2/3 receptor availability: a [18F]fallypride PET study. Eur Neuropsychopharmacol. doi:pii: S0924-977X(13)00048-5. Sativex monograph. Available at: http://www.ukcia.org/research/SativexMonograph.pdf (accessed 21 August 2013). Schep LJ, Slaughter RJ, Temple WA (2011) Synthetic cannabinoid use in New Zealand: a brief evaluation of inquiries to the New Zealand National Poisons Centre. N Z Med J 124:99–101. Schneir AB, Baumbacher T (2012) Convulsions associated with the use of a synthetic cannabinoid product. J Med Toxicol 8:62–64. Schneir AB, Cullen J, Ly BT (2011) ‘Spice’ girls: synthetic cannabinoid intoxication. J Emerg Med 40:296–299. Seely KA, Prather PL, James LP, Moran JH (2011) Marijuana-based drugs: innovative therapeutics or designer drugs of abuse? Mol Interv 11:36–51. Shevyrin V, Melkozerov V, Nevero A, Eltsov O, Morzherin Y, Shafran Y (2012) Identification and analytical properties of new synthetic cannabimimetics bearing 2,2,3,3-tetramethylcyclopropanecarbonyl moiety. Foren Sci Int 226:62–73. Showalter VM, Compton DR, Martin BR, Abood ME (1996) Evaluation of binding in a transfected cell line expressing a peripheral cannabinoid receptor (CB2): identification of cannabinoid receptor subtype selective ligands. J Pharmacol Exp Ther 278:989–999. Simmons J, Cookman L, Kang C, Skinner C (2011) Three cases of ‘spice’ exposure. Clin Toxicol (Phila) 49:431–433. Simolka K, Lindigkeit R, Schiebel HM, Papke U, Ernst L, Beuerle T (2012) Analysis of synthetic cannabinoids in ‘spice-like’ herbal highs: snapshot of the German market in summer 2011. Anal Bioanal Chem 404:157–171. Sobolevsky T, Prasolov I, Rodchenkov G (2010) Detection of JWH-018 metabolites in smoking mixture post-administration urine. Forensic Sci Int 200:141–147. Teske J, Weller JP, Fieguth A, Rothämel T, Schulz Y, Tröger HD (2010) Sensitive and rapid quantification of the cannabinoid receptor agonist naphthalen-1-yl-(1-pentylindol-3-yl)methanone (JWH-018) in human serum by liquid chromatographytandem mass spectrometry. J Chromatogr B Analyt Technol Biomed Life Sci 878:2659–2663. Thomas S, Bliss S, Malik M (2012) Suicidal ideation and self-harm following K2 use. J Okla State Med Ossoc 105:430–433. Tung CK, Chiang TP, Lam M (2012) Acute mental disturbance caused by synthetic cannabinoid: a potential emerging substance of abuse in Hong Kong. East Asian Arch Psychiatry 22:31–33. Uchiyama N, Kikura-Hanajiri R, Ogata J, Goda Y (2010) Chemical analysis of synthetic cannabinoids as designer drugs in herbal products. Forensic Sci Int 198:1–8. Uchiyama N, Kawamura M, Kikura-Hanajiri R, Goda Y (2011a) Identification and quantitative analyses of two cannabinomimetic phenacetylindoles, JWH-251 and JHW-250, and four cannabinomimetic naphtoylindoles, JWH-081, JWH-015, JWH-200 and JW-073, as designer drugs in illegal products. Forensic Toxic 29:25–37. Uchiyama N, Kikura-Hanajiri R, Goda Y (2011b) Identification of a novel cannabinomimetic phenylacetylindole, cannabipiperididiethanone, as a designer drug in a herbal product and its affinity for CB1 and CB2 receptors. Chem Pharm Bull 59:1203–1205. Uchiyama N, Kikura-Hanajiri R, Matsumoto N, Huang Z-L, Goda Y, Urade Y (2012) Effects of synthetic cannabinoids on electroencephalogram power spectra in rats. Forensic Sci Int 215:179–183. Uchiyama N, Kawamura M, Kikura-Hanajiri R, Goda Y (2013) URB-754: a new class of designer drug and 12 synthetic cannabinoids detected in illegal products. Forensic Sci Int 227:21–32. UNODC (United Nations Office on Drugs and Crime) (2010). Synthetic cannabinoids in herbal products. Available at: http:// www.unodc.org/documents/scientific/ Synthetic_Cannabinoids.pdf (accessed 24 April 2013). Vandrey R, Dunn KE, Fry JA, Girling ER (2012) A survey study to characterize use of Spice products (synthetic cannabinoids). Drug Alcohol Depend 120:238–241. Vann RE, Warner JA, Bushell K, Huffman JW, Martin BR, Wiley JL (2009) Discriminative stimulus properties of Δ9-tetrahydrocannabinol (THC) in C57Bl/6J mice. Eur J Pharmacol 615:102–107. Vardakou I, Pistos C, Spiliopoulou C (2010) Spice drugs as a new trend: mode of action, identification and legislation. Toxicol Lett 197:157–162. Vearrier D, Osterhoudt KC (2010) A teenager with agitation: higher than she should have climbed. Pediatr Emerg Care 26:462–465. Watanabe K, Yamaori S, Funahashi T, Kimura T, Yamamoto I (2007) Cytochrome P450 enzymes involved in the metabolism of tetrahydrocannabinols and cannabinol by human hepatic microsomes. Life Sci 80:1415–1419. Wiebelhaus JM, Poklis JL, Poklis A, Vann RE, Lichtman AH, Wise LE (2012) Inhalation exposure to smoke from synthetic “marijuana” produces potent cannabimimetic effects in mice. Drug Alcohol Depend 126:316–323. Winstock AR, Barratt MJ (2013) Synthetic cannabis: a comparison of patterns of use and effect profile with natural cannabis in a large global sample. Drug Alcohol Depend 131:106–111. Wintermeyer A, Möller I, Thevis M, Jübner M, Beike J, Rothschild MA, Bender K (2010) In vitro phase I metabolism of the synthetic cannabimimetic JWH-018. Anal Bioanal Chem 398:2141–2153. Synthetic cannabimimetics as drugs of abuse 525 Xi ZX, Peng XQ, Li X, Song R, Zhang HY, Liu QR, Yang HJ, Bi GH, Li J, Gardner EL (2011) Brain cannabinoid CB2 receptors modulate cocaine’s actions in mice. Nat Neurosci 14:1160–1166. Young AC, Schwarz E, Medina G, Obafemi A, Feng SY, Kane C, Kleinschmidt K (2012) Cardiotoxicity associated with the synthetic cannabinoid, K9, with laboratory confirmation. Am J Emerg Med 30:1320.e5–e7. Zawilska JB (2011) ‘Legal highs’ – new players in the old drama. Curr Drug Abuse Rev 4:122–130. Zimmermann US, Winkelmann PR, Pilhatsch M, Nees JA, Spanagel R, Schulz K (2009) Withdrawal phenomena and dependence syndrome after the consumption of ‘spice gold’. Dtsch Arztebl Int 106:464–467. Zuba D, Byrska B, Maciow M (2011) Comparison of ‘herbal highs’ composition. Anal Bioanal Chem 400:119–126.