* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Influence of Mutation Type and Location on Phenotype
Population genetics wikipedia , lookup
Pharmacogenomics wikipedia , lookup
No-SCAR (Scarless Cas9 Assisted Recombineering) Genome Editing wikipedia , lookup
Saethre–Chotzen syndrome wikipedia , lookup
Koinophilia wikipedia , lookup
Neuronal ceroid lipofuscinosis wikipedia , lookup
Microevolution wikipedia , lookup
Epigenetics of neurodegenerative diseases wikipedia , lookup
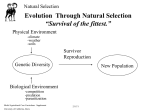
Oncogenomics wikipedia , lookup
P. Huppke1 M. Held1 F. Hanefeld1 W. Engel2 F. Laccone2 Influence of Mutation Type and Location on Phenotype in 123 Patients with Rett Syndrome Introduction Rett syndrome (RTT) is a neurodevelopmental disorder that almost exclusively affects girls. It is caused by mutations in the MECP2 gene that encodes the methyl-CpG-binding protein 2 (MeCP2). In this study we correlated mutation type and location with the severity of the phenotype in 123 girls with RTT. The ability to sit, walk, speak, hand function, head growth, occurrence of epilepsy and a combined severity score were assessed in all girls at 5 years of age and then statistically correlated with the results of the molecular genetic tests. We found that patients who carry either missense mutations or deletions located within the hotspot for deletions, an area between the base pairs (bp) 1030 and 1207 of the MECP2 gene, present with a milder phenotype than other patients. We correlated the location of the mutations with the phenotype and found that all mutations that lead to either a complete or partial truncation of the region coding for the nuclear localisation signal (NLS) are associated with a more severe phenotype than other truncating mutations (p = 0.001). We did not find a significant difference between the patients with mutations in the methyl-CpG-binding domain (MBD) and those with mutations in the transcriptional repression domain (TRD). We conclude that mutation type and location correlate with the phenotype in Rett syndrome. All mutations that impair the nuclear localisation signal (NLS) are associated with more severe phenotypes. Rett syndrome (RTT) is, with an incidence of 1/10 000 to 1/ 15 000, one of the most common causes of severe mental retardation in females [14]. It is characterized by a period of normal development that lasts 8 to 18 months followed by neurologic regression affecting both motor and mental abilities. Coinciding with the loss of purposeful use of the hands is the appearance of stereotypic hand movements. In most girls head growth decelerates long before the onset of other symptoms [15]. Key words Rett Syndrome ± Genotype and Phenotype Correlation ± RTT Severity Score 1 In 1999 Amir et al were the first to describe mutations in the MECP2 gene as a cause of RTT [2]. The MECP2 gene encodes the methyl-CpG binding protein 2 (MeCP2), one of four methyl-CpG binding proteins that are known so far [12, 22, 23]. MeCP2 binds to methylated CpG dinucleotides and interacts with the Sin3 A/ histone co-repressor complex and histone deacetylases [19, 34]. Deacetylation of core histones converts the chromatin structure into an inactive state [33]. MeCP2 is involved in the long-term silencing of genes in mammalian cells [28]. Two functional domains have been identified:1) the methyl-CpG-binding domain (MBD) that binds to the methylated DNA, and 2) the transcriptional repression domain (TRD) that interacts with the corepressor Sin3 A and the histone deacetylases [26, 27]. A nuclear localisation signal (NLS) that mediates the transport of MeCP2 into the nucleus is located within the TRD (27). It has been found that mutations in MECP2 account for 70 ± 80 % of RTT cases [1, 3, 5 ± 8,10,17,18, 21, 29, 31, 35, 37]. Two different genetic factors are likely to influence the phenotype in RTT: X inactivation and the type and location of the mutations. In three cases of familial RTT, skewed X inactivation was Affiliation Abteilung Kinderheilkunde, Schwerpunkt Neuropädiatrie, Georg-August-Universität Göttingen, Göttingen, Germany 2 Institut für Humangenetik, Georg-August-Universität Göttingen, Göttingen, Germany Correspondence Dr. P. Huppke ´ Department of Neuropaediatrics, Georg-August-University of Göttingen ´ Robert-Koch-Straûe 40 ´ 37075 Göttingen ´ Germany ´ E-mail: [email protected] Received: November 8, 2001 ´ Accepted after Revision: January 25, 2002 Bibliography Neuropediatrics 2002; 33: 63 ± 68 Georg Thieme Verlag Stuttgart ´ New York ´ ISSN 0174-304X Original Article Abstract 63 found on maternal investigation. The mothers were either clinically normal or exhibited only minor neurological symptoms [32, 35]. Amir et al described one patient with skewed X inactivation and a milder phenotype, while the skewed X inactivation found by Auranen et al in two females did not contribute to the severity of the phenotype [3, 5]. Furthermore, several studies have demonstrated normal X inactivation patterns in the majority of RTT cases [3 ± 5, 9, 20, 24, 36, 38]. Original Article 64 Five studies have been performed so far addressing the influence of mutation type and location. Amir et al included 57 patients and compared 13 clinical characteristics, electrophysiological studies and cerebrospinal fluid neurochemistry between patients with missense mutations and patients carrying truncating mutations [3]. They found that awake respiratory dysfunction was more frequent in patients with truncating mutations and that missense mutations were associated with the presence of scoliosis. However, no correlation was seen between a Composite Clinical Severity Score and the type of mutation. Cheadle et al included 44 patients in their study [10]. They used a severity score that assessed the abilities of hand use, speech, and walking. They found that truncating mutations were associated with more severe phenotypes than missense mutations and that late truncating mutations produced milder phenotypes than early truncating mutations. Huppke et al also assessed the ability to sit, walk and speak at age 5 years in 31 patients with RTT and found no correlation between severity of the phenotype and mutation type or location [18]. Auranen et al and Nielsen et al have performed the most recent studies on 39 patients and 26 patients respectively [5, 29]; both found no significant correlation between the clinical course and the mutation type. This study was performed to analyse genotype/phenotype correlation with respect to type and location of mutations. We did not study X inactivation because other studies have shown that it is only an important factor in a minority of patients. Methods Subjects and clinical evaluation We evaluated the clinical data of 123 females with the diagnosis of RTT and mutations in MECP2. Half of the patients (n = 67) were examined by us in the Neuropaediatric Department in Göttingen. For the remaining 68 females the data were obtained by questionnaire and complemented by telephone interviews. Because the clinical pattern of regression seen in Rett syndrome occurs over a variable time period [15], we decided to evaluate the clinical status at 5 years of age in order to obtain comparable data. At this age most girls with Rett syndrome are in a relatively stable phase (pseudostationary stage) [15]. The following clinical features were included in our study: ability to sit, walk and talk (more than 10 words), hand function (being able to finger feed), Sitting Walking Speech Hand function Head growth Epilepsy Sitting unsupported at age 5 years 1 Loss of ability to sit 2 Never learned to sit 3 Walking unsupported at age 5 years 1 Loss of ability to walk 2 Never learned to walk 3 More than ten words at age 5 years 1 Loss of ability to speak 2 Never spoken 3 Good hand function at age 5 years 1 Loss of hand function 2 Never had good hand function 3 Normal head growth at age 5 years 1 Deceleration of head growth 2 Microcephaly 3 Epilepsy at age 5 years 1 No epilepsy at age 5 years 2 head growth and epilepsy at age 5. We tried to keep the severity grading of the selected features as simple as possible to avoid unreliable results (Table 1). Each clinical feature was graded from 1 to 3 except for epilepsy, which was only graded out of 2 reflecting the yes/no recording of this finding. A cumulative total of the 6 grades was calculated to create a clinical severity score ranging from 6, representing the mildest phenotype, to 17 representing the most severe phenotype. The data gathered concerning some features of RTT (breathing abnormalities, stereotypic hand movements, autistic behaviour, onset of first symptoms, onset of regression) were not reliable enough to be included in this study. Girls with RTT are difficult to examine because they often react negatively to an unfamiliar environment. Furthermore, data cannot be reliably obtained from non-medical persons. Genotype-phenotype correlation analysis The type and location of the mutations were correlated with the clinical data. The types of mutations were divided into three different groups: 1) Truncating mutations that include nonsense mutations, deletions (excluding patients with deletions between bp 1030 and 1207 of the genes), insertions and splice site mutations; 2) Missense mutations; 3) Deletions between bp 1030 and 1207 of the gene. This third group of patients represents deletions within the hotspot for deletions at the 3¢ end of the gene and was considered separately from other patients with truncating mutations because we observed on neurological examination that these patients are distinctly more mildly affected than most other patients. The locations of the mutations were also divided into three groups: 1) mutations in the MBD, 2) mutations in the TRD, and 3) mutations in the NLS. The NLS is located within the TRD. Females with mutations in the NLS were not part of the TRD group. Huppke P et al. Influence of Mutation ¼ Neuropediatrics 2002; 33: 63 ± 68 Mutation analysis The entire coding region and flanking intron sequences were sequenced using the method described earlier [18]. A detailed report on the results of the mutation analysis has been published elsewhere [18, 21]. The sequence analysis of all patients were performed in the laboratory of one of us (F.L.). Table 1 Severity grading of the clinical features The association between each group and the individual characteristics as well as the severity score was calculated using the Mann-Whitney U-test. A p value below 0.05 was considered significant. Phenotype In 8 % of all patients no deceleration of head growth occurred. 39% showed a deceleration of head growth but no microcephaly and 53% were microcephalic at age 5. Epilepsy was present in 40 % of all patients at 5 years of age. 85% of the girls were still able to sit unsupported while 7 % had lost this ability and 8% had never achieved this milestone. 50 % were walking unsupported at age 5, 3 % had lost the ability and 47 % had never learned to walk. 15 % showed preserved hand function, 65 % had lost their hand function and 20 % have never had good hand function. Assessment of the ability to speak showed that 12 % were able to say more than 10 words, 53% had lost this ability and 35% have never had it. Genotype The detailed results of the mutational analysis have been published earlier by Huppke et al (11 patients) and Laccone et al (94 patients) [18, 21]. 18 new patients were included in this study (Table 2). Among the 123 girls we found 19 deletions, 2 splice site mutations, 2 insertion, 50 missense mutations and 50 nonsense mutations. 40 girls carry mutations in the MBD, 29 in the TRD and 23 in the NLS (Fig. 1). Patients (n) Domain Mutation Nucleotide change 1 MBD R106 W 316 C > T [3] 2 MBD D156E 468 C > G [17] 2 MBD T158 M 473 C > T [3] 1 Reference 531 delA 1 TRD 3 TRD 1 TRD 1 NLS 1 TRD 635 ± 655 del P225 R 674 C > G [17] Original Article Results Table 2 Results of the molecular genetic analysis of 18 patients that were not presented previously. Nucleotides numbered from the ATG initiator codon 753 delC R270 X 808 C > T [17] 880 ± 884 del 1 1098 ± 1117 del 1 1121 ± 1191 del 1 1157 ± 1188 del 1 1163 ± 1188 del 1 1167 ± 1200 del 16 14 Patients (n) Because we found that patients who carry mutations in the NLS are more severely affected than the others, we performed a second analysis to see if other mutations that lead to a truncated protein of the NLS lead to more severe phenotypes as well. We therefore divided the patients into two groups: 1) girls with truncating mutations located either before or within the NLS, 2) all other patients with truncating mutations. 12 10 8 6 4 2 0 0 200 400 600 800 1000 1200 1400 bp Transcriptional repression domain TRD Nuclear localisation signal NLS Methyl CpG binding domain MBD Huppke P et al. Influence of Mutation ¼ Neuropediatrics 2002; 33: 63 ± 68 Genotype-phenotype correlation Type of mutation: Patients with truncating mutations are more likely to exhibit decelerated head growth (p = 0.00 003) and be unable to walk at age 5 (p = 0.031) than patients who carry missense mutations. No significant difference was found when we tested for epilepsy (p = 0.3413), hand function (p = 0.928) and ability to sit (p = 0.624) and speak (p = 0.596) at 5 years of age. Patients with truncating mutations are more likely to present with a deceleration of head growth (p = 0.007), walk less frequently (p = 0.006) and are more likely to lose their hand function (p = 0.008) than those who carry deletions between bp 1030 and 1207 (the hotspot for deletions). The ability to sit (p = 0.134) and speak (p = 0.795) and the occurrence of epilepsy (p = 0.277) were not significantly different between these groups. Comparison of patients with missense mutations with those carrying deletions within the hotspot showed that the patients with deletions were more likely to have preserved hand function (p = 0.008). No significant difference was found when we tested for deceleration of head growth (p = 0.434), epilepsy (p = 0.584) Fig. 1 Type and location of the mutations that were detected in the RTT patients. Squares represent missense mutations, triangles deletions in the deletion hot spot and diamonds the other truncating mutations. and ability to sit (p = 0.192), walk (p = 0.113) and speak (p = 0.992) at age 5. Patients with truncating mutations (mean score = 11.8) had higher severity scores than both patients with missense mutations (mean score = 10.3) (p = 0.002) and patients with deletions within the hotspot (mean score = 9.7) (p = 0.004). The difference between patients with missense mutations and deletions within the hotspot was not significant (p = 0.331). Location of mutations: Patients who carry mutations in the TRD do not differ significantly from the group with mutations in the MBD. The group with mutations in the NLS were more likely to present with deceleration of head growth (p = 0.018), an inability to walk 65 Table 3 Results of the statistical analysis. The groups with the higher scores are placed on the left. P values under 0.05 were considered significant Groups Sitting p (n) Walking p (n) Hand function p (n) Speech p (n) Epilepsy p (n) Head growth p (n) Severity score p (n) Truncating/missense 0.624 (62/50) 0.031 (62/50) 0.928 (62/49) 0.596 (60/51) 0.341 (60/50) 0.00003 (62/50) 0.002 (58/50) Truncating/deletions 0.133 (62/11) 0.006 (62/11) 0.007 (62/11) 0.794 (60/11) 0.277 (60/11) 0.007 (62/11) 0.004 (58/11) Missense/deletions 0.192 (50/11) 0.113 (50/11) 0.018 (49/11) 0.992 (51/11) 0.584 (50/11) 0.436 (50/11) 0.330 (50/11) MBD/TRD 0.067 (40/29) 0.312 (40/29) 0.0004 (40/28) 0.394 (40/29) 0.971 (40/29) 0.363 (40/29) 0.454 (40/28) NLS/TRD 0.063 (23/29) 0.049 (23/29) 0.005 (23/28) 0.424 (22/29) 0.741 (21/29) 0.018 (23/29) 0.004 (21/28) Original Article NLS/MBD 0.974 (23/40) 0.225 (23/40) 0.650 (23/40) 0.881 (22/40) 0.749 (21/40) 0.002 (23/40) 0.034 (21/40) Truncating NLS/ Truncating after NLS 0.010 (48/25) 0.012 (48/25) 0.0001 (48/23) 0.945 (47/24) 0.872 (46/25) 0.0006 (48/25) 0.001 (45/23) Truncating NLS/rest TRD 0.012 (48/24) 0.021 (48/24) 0.0001 (48/23) 0.332 (47/24) 0.718 (46/24) 0.0003 (48/24) 0.0006 (46/22) (p = 0.049) and loss of hand function (p = 0.005) than patients who carry mutations in the TRD. No significant difference was found when comparing sitting (p = 0.063), speech (p = 0.424) and occurrence of epilepsy (p = 0.741). The only significant difference between patients with mutations in the NLS and those with mutations in the MBD is that they were more likely to present with a deceleration of head growth (p = 0.002). Patients with mutations in the NLS (mean score = 12) had higher severity scores than both those with mutations in the MBD (mean score = 10.8) (p = 0.034) and those with mutations in the TRD (mean score = 10.1) (p = 0.004), while the MBD and the TRD group did not differ significantly. 66 Discussion Phenotype We present the largest study published to date correlating the phenotype of RTT patients with type and location of mutations in the MECP2 gene. We assessed 6 clinical features of RTT patients at the age of 5 years, during the pseudostationary period, in order to obtain comparable data [15]. We found that the majority was microcephalic at the age of 5 years with only 8% exhibiting no deceleration of head growth. Epilepsy was present in 40 % of the patients. This figure is less than recently reported, Genotype-phenotype correlation In the studies published so far, conflicting results have been found as to whether the type of mutation influences the phenotype. Amir et al found no correlation between their Composite Clinical Severity Score and the type of mutation [3]. The same result was found by Huppke et al, Auranen et al and Nielsen et al [5,18, 29]. However, Cheadle et al in their study of 44 patients found that girls with truncating mutations present with higher severity scores [10]. They excluded 2 patients with late truncating mutations from their study because they represented outliers in terms of their clinical presentation. We also found that the group of girls with deletions within the deletion hotspot (bp 1030 to 1207) of the MECP2 gene present with a milder phenotype and therefore decided to place them in an individual group. Our clinical impression was confirmed by statistical analysis. The group with deletions within the hotspot for deletions had significantly lower severity scores than the group that included all other patients with truncating mutations. We also found that the group with missense mutations had lower severity scores than the patients with truncating mutations. Most likely Amir et al, Huppke et al, Auranen et al and Nielsen et al did not find this correlation because the patients with deletions within the hotspot region were included in the truncating group [3, 5,18, 29]. Huppke P et al. Influence of Mutation ¼ Neuropediatrics 2002; 33: 63 ± 68 Mutations truncating the NLS: When compared with other truncating mutations, we found that mutations that lead to a truncated NLS were more likely to present clinically with deceleration of head growth (p = 0.0006), inability to walk (p = 0.012) and loss of hand function (p = 0.0001). The severity scores found in the group with mutations that lead to a partial or complete truncation of the NLS were significantly higher than in the group with truncating mutations localised after the NLS (p = 0.001). The group with mutations that lead to a partial or complete truncation of the NLS also had higher severity scores than those patients with mutations in the remaining segment of the TRD downstream of the NLS (p = 0.0006). The frequency of deceleration of head growth (p = 0.0003), inability to sit (p = 0.012) and walk (p = 0.021) and loss of hand function (p = 0.0001) was higher (Table 3). most likely because the first presentation of epilepsy can occur later in life [30]. The majority (85%) of all patients learned to sit unsupported which is in accordance with the fact that this developmental milestone is often acquired before the appearance of the rapid phase of regression which normally presents between 12 to 18 months. Walking unsupported was only achieved and maintained by 50 % of the girls while 47% never learned to walk. Because only very few (3%) of the children lost the ability to walk the determining factor might be whether or not they had achieved this milestone before the onset of regression. Loss of hand function is one of the diagnostic criteria in RTT [14]. However, we found that 20 % of our patients never had normal hand function. 65% of the patients learned to speak but only 12 % maintained this ability to a certain extent. It seems that abilities that require higher brain functions like language and hand function are more prone to be lost during the phase of regression than gross motor skills like walking and sitting which once learned appear to be maintained. Type and location of mutations do not influence all features of RTT in the same way. We found no significant correlation between the occurrence of epilepsy and the ability to speak. Hand function in patients with deletion within the hotspot was significantly more preserved than in other patients. Head growth, on the other hand, was more likely to be decelerated in patients with truncating mutations than in those with missense mutations while the latter group did not differ from the patients with deletions within the hotspot region. Too little is known about the function of MeCP2 to interpret these findings. Huppke P et al. Influence of Mutation ¼ Neuropediatrics 2002; 33: 63 ± 68 Genotype/phenotype correlations provide valuable information necessary for genetic counselling. We think our study contributes useful information towards this purpose. Finally, it is important to mention that although a severity score might reflect the biological severity of the disease it does not necessarily reflect the social severity. We found that very mildly affected girls often create problems within their families, which more severely affected ones do not. They are more mobile, restless and some of them exhibit aggressive behaviour. This must be kept in mind during consultations with the parents concerning the future development of their children. Acknowledgments The authors would like to thank those families who participated in our study. We also acknowledge the help of the Elternhilfe für Kinder mit Rett-Syndrom (Parent Support Group for Children with RTT) and the physicians who answered the questionnaires. We thank N. Dankenbrink, S. Herlt, K. Rücker and U. Lenz for their technical help. References 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 Amano K, Nomura Y, Segawa M et al. Mutational analysis of the MECP2 gene in Japanese patients with Rett syndrome. J Hum Genet 2000; 45: 231 ± 236 Amir RE, Van den Veyver IB, Wan M et al. Rett syndrome is caused by mutations in X-linked MECP2, encoding methyl- CpG-binding protein 2. Nat Genet 1999; 23: 185 ± 188 Amir RE, Van den Veyver IB, Schultz R et al. Influence of mutation type and X chromosome inactivation on Rett syndrome phenotypes. Ann Neurol 2000; 47: 670 ± 679 Anvret M, Wahlstrom J. Rett syndrome: random X chromosome inactivation. Clin Genet 1994; 45: 274 ± 275 Auranen M, Vanhala R, Vosman M et al. MECP2 gene analysis in classical Rett syndrome and in patients with Rett-like features. Neurology 2001; 56: 611 ± 617 Bienvenu T, Carrie A, de Roux N et al. MECP2 mutations account for most cases of typical forms of Rett syndrome. Hum Mol Genet 2000; 9: 1377 ± 1384 Bourdon V, Philippe C, Labrune O et al. A detailed analysis of the MECP2 gene: prevalence of recurrent mutations and gross DNA rearrangements in Rett syndrome patients. Hum Genet 2001; 108: 43 ± 50 Buyse IM, Fang P, Hoon KT et al. Diagnostic testing for Rett syndrome by DHPLC and direct sequencing analysis of the MECP2 gene: identification of several novel mutations and polymorphisms. Am J Hum Genet 2000; 67: 1428 ± 1436 Camus P, Abbadi N, Perrier MC et al. X chromosome inactivation in 30 girls with Rett syndrome: analysis using the probe. Hum Genet 1996; 97: 247 ± 250 Cheadle JP, Gill H, Fleming N et al. Long-read sequence analysis of the MECP2 gene in Rett syndrome patients: correlation of disease severity with mutation type and location. Hum Mol Genet 2000; 9: 1119 ± 1129 Chen RZ, Akbarian S, Tudor M et al. Deficiency of methyl-CpG binding protein-2 in CNS neurons results in a Rett-like phenotype in mice. Nat Genet 2001; 27: 327 ± 331 DEsposito M, Quaderi NA, Ciccodicola A et al. Isolation, physical mapping, and Northern analysis of the X-linked human gene encoding methyl CpG-binding protein, MECP2. Mamm Genome 1996; 7: 533 ± 535 Guy J, Hendrich B, Holmes M et al. A mouse MeCP2-null mutation causes neurological symptoms that mimic Rett syndrome. Nat Genet 2001; 27: 322 ± 326 Hagberg B. Retts syndrome: prevalence and impact on progressive mental retardation in girls. Acta Pediatr Scand 1985; 74: 405 ± 408 Hagberg BA. Rett syndrome: clinical peculiarities, diagnostic approach, and possible cause. Pediatr Neurol 1985; 5: 75 ± 83 Hagberg G, Stenbom Y, Witt Engerstrom I. Head growth in Rett syndrome. Acta Paediatr 2000; 89: 198 ± 202 Hampson K, Woods CG, Latif F et al. Mutations in the MECP2 gene in a cohort of girls with Rett syndrome. J Med Genet 2000; 37: 610 ± 612 Huppke P, Laccone F, Kramer N et al. Rett syndrome: analysis of MECP2 and clinical characterization of 31 patients. Hum Mol Genet 2000; 9: 1369 ± 1375 Jones PL, Veenstra GJ, Wade PA et al. Methylated DNA and MeCP2 recruit histone deacetylase to repress transcription. Nat Genet 1998; 19: 187 ± 191 Kormann-Bortolotto MH, Woods CG, Green SH et al. X-inactivation in girls with Rett syndrome. Clin Genet 1992; 42: 296 ± 301 Laccone F, Huppke P, Hanefeld F et al. Mutation spectrum in patients with Rett syndrome in the German population: Evidence of hot spot regions. Hum Mutat 2001; 17: 183 ± 90 Lewis JD, Meehan RR, Henzel WJ et al. Purification, sequence, and cellular localization of a novel chromosomal protein that binds to methylated DNA. Cell 1992; 69: 905 ± 914 Meehan RR, Lewis JD, Bird AP. Characterization of MeCP2, a vertebrate DNA binding protein with affinity for methylated DNA. Nucleic Acids Res 1992; 20: 5085 ± 5092 Migeon BR, Dunn MA, Thomas G et al. Studies of X inactivation and isodisomy in twins provide further evidence that the X chromosome is not involved in Rett syndrome. Am J Hum Genet 1995; 56: 647 ± 653 Nan X, Campoy FJ, Bird A. MeCP2 is a transcriptional repressor with abundant binding sites in genomic chromatin. Cell 1997; 88: 471 ± 481 Original Article Cheadle et al, Huppke et al and Amano et al studied the influence of the location of the mutations on the phenotype [1,10,18]. Cheadle et al found that early truncating mutations were associated with a more severe phenotype than late truncating mutations and that there was no difference in severity between missense mutations in the TRD and the MBD [10]. Amano et al found that mutations in the MBD were associated with a more severe phenotype, while Huppke et al found no correlation [1,18]. In our study there was no difference between the severity scores of patients with missense mutations in the MBD and the TRD (data not shown). We found that mutations that lead to a complete or partial truncation of the region that codes for the nuclear localisation signal (NLS) lead to a more severe phenotype than other mutations in the TRD and truncating mutations located downstream of the NLS. Nan et al found that the NLS is essential for the nuclear localisation of MeCP2 [27]. Therefore, mutations that lead to a truncation of the NLS produce proteins that will remain in the cytoplasm. In accordance with these findings recent experiments with mice lacking MeCP2 have indicated that many patients with RTT have null mutations [11,13]. The milder phenotype seen in patients with missense mutations and truncating mutations downstream of the NLS is therefore likely to be due to the presence of residual protein function. 67 26 27 28 29 30 31 Original Article 32 Nan X, Meehan RR, Bird A. Dissection of the methyl-CpG binding domain from the chromosomal protein MeCP2. Nucleic Acids Res 1993; 21: 4886 ± 4892 Nan X, Tate P, Li E et al. DNA methylation specifies chromosomal localization of MeCP2. Mol Cell Biol 1996; 16: 414 ± 421 Ng HH, Zhang Y, Hendrich B et al. MBD2 is a transcriptional repressor belonging to the MeCP1 histone deacetylase complex. Nat Genet 1999; 23: 58 ± 61 Nielsen JB, Henriksen KF, Hansen C et al. MECP2 mutations in Danish patients with Rett syndrome: High frequency of mutations but no consistent correlations with clinical severity or with the X chromosome inactivation pattern. Eur J Hum Genet 2001; 9: 178 ± 184 Steffenburg U, Hagberg G, Hagberg B. Epilepsy in a representative series of Rett syndrome. Acta Paediatr 2001; 90: 34 ± 39 Vacca M, Filippini F, Budillon A et al. Mutation analysis of the MECP2 gene in British and Italian Rett syndrome females. J Mol Med 2001; 78: 648 ± 655 Villard L, Kpebe A, Cardoso AK et al. Two affected boys in a Rett syndrome family: clinical and molecular findings. Neurology 2000; 55: 1188 ± 1193 33 34 35 36 37 38 Wade PA, Jones PL, Vermaak D et al. Histone deacetylase directs the dominant silencing of transcription in chromatin: association with MeCP2 and the Mi-2 chromodomain SWI/SNF ATPase. Cold Spring Harb Symp Quant Biol 1998; 63: 435 ± 445 Wade PA, Gegonne A, Jones PL et al. Mi-2 complex couples DNA methylation to chromatin remodelling and histone deacetylation. Nat Genet 1999; 23: 62 ± 66 Wan M, Lee SS, Zhang X et al. Rett syndrome and beyond: recurrent spontaneous and familial MECP2 mutations at CpG hotspots. Am J Hum Genet 1999; 65: 1520 ± 1529 Webb T, Watkiss E. A comparative study of X-inactivation in Rett syndrome probands and control subjects. Clin Genet 1996; 49: 189 ± 195 Xiang F, Buervenich S, Nicolao P et al. Mutation screening in Rett syndrome patients. J Med Genet 2000; 37: 250 ± 255 Zoghbi HY, Percy AK, Schultz RJ et al. Patterns of X chromosome inactivation in the Rett syndrome. Brain Dev 1990; 12: 131 ± 135 68 Huppke P et al. Influence of Mutation ¼ Neuropediatrics 2002; 33: 63 ± 68