* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Assembly factors as a new class of disease
Epigenetics of human development wikipedia , lookup
Genome (book) wikipedia , lookup
Microevolution wikipedia , lookup
Polycomb Group Proteins and Cancer wikipedia , lookup
Oncogenomics wikipedia , lookup
Neuronal ceroid lipofuscinosis wikipedia , lookup
Frameshift mutation wikipedia , lookup
Mitochondrial DNA wikipedia , lookup
Epigenetics of neurodegenerative diseases wikipedia , lookup
Mitochondrial Eve wikipedia , lookup
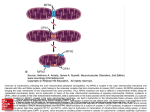
doi:10.1093/brain/awr261 Brain 2012: 135; 12–22 | 12 BRAIN A JOURNAL OF NEUROLOGY REVIEW ARTICLE Assembly factors as a new class of disease genes for mitochondrial complex I deficiency: cause, pathology and treatment options Jessica Nouws, Leo G. J. Nijtmans, Jan A. Smeitink and Rutger O. Vogel Nijmegen Centre for Mitochondrial Disorders at the Department of Paediatrics, Radboud University Nijmegen Medical Centre, 6500 HB, Nijmegen, The Netherlands Correspondence to: Leo G. J. Nijtmans, Department of Paediatrics, Radboud University Nijmegen Medical Centre, Geert Grooteplein 10, PO BOX 9101, 6500 HB, Nijmegen, The Netherlands E-mail: [email protected] Complex I deficiency is the most frequent cause of oxidative phosphorylation disorders. The disease features a large diversity of clinical symptoms often leading to progressive encephalomyopathies with a fatal outcome. There is currently no cure, and although disease-causing mutations have been found in the genes encoding complex I subunits, half of the cases remain unexplained. However, in the past 5 years a new class of complex I disease genes has emerged with the finding of specific assembly factors. So far nine such genes have been described and it is believed that in the near future more will be found. In this review, we will address whether the functions of these chaperones point towards a general molecular mechanism of disease and whether this enables us to design a treatment for complex I deficiency. Keywords: complex I deficiency; assembly factors; treatment Abbreviations: NADH = nicotinamide adenine dinucleotide; OXPHOS = oxidative phosphorylation Introduction Mitochondrial complex I [nicotinamide adenine dinucleotide (NADH) : ubiquinone oxidoreductase; EC 1.6.5.3] is vital to the energy supply in the body. It is the first enzyme in oxidative phosphorylation (OXPHOS), the process in which breakdown of organic nutrients is coupled to ATP production. Disturbances in complex I function can result in complex I deficiency (OMIM 252 010), which is the most common biochemical defect of the OXPHOS system. It is estimated that OXPHOS disorders occur once in every 5000 newborns (Skladal et al., 2003), of which complex I deficiency underlies 25–35% (Loeffen et al., 2000; Bugiani et al., 2004; Scaglia et al., 2004; Thorburn, 2004). It typically features a severe multisystem decline with a poor prognosis, and currently lacks a cure. Although complex I dysfunction initially attracted attention in the context of inherited metabolic disorders, it is now increasingly implicated in diabetes and neurodegenerative disorders such as Parkinson’s disease and Alzheimer’s disease (Mootha et al., 2003; Eckert et al., 2010; Winklhofer and Haass, 2010). This makes a better understanding of complex I deficiency of relevance for the general population. Complex I is the product of seven mitochondrial and 38 nuclear genes (Carroll et al., 2006). During the past two decades only 33% of the complex I deficiencies could be explained by Received May 13, 2011. Revised July 4, 2011. Accepted July 11, 2011. Advance Access publication October 27, 2011 ß The Author (2011). Published by Oxford University Press on behalf of the Guarantors of Brain. All rights reserved. For Permissions, please email: [email protected] A new class of complex I disease genes mutations in these genes (Calvo et al., 2010). To explain most of the remaining cases it was inferred that complex I assembly factors must exist analogous to the 20 or more found essential to complex IV assembly. Indeed, in 2002, the first complex I assembly factor was found (Janssen et al., 2002), and in 2005 the first factor was implicated in complex I deficiency (Ogilvie et al., 2005). Since then genetic, bioinformatic and proteomic analyses have led to the identification of no less than nine disease-causing assembly factors in only half a decade. Seven of these were found in the past 3 years, promising great growth in the field for the coming years. In this review, we will address whether these individual discoveries share similarities in terms of function or disease pathology. Furthermore, we will investigate the putative pathological distinction of complex I deficiency caused by mutations in assembly factors versus structural subunits, and highlight therapeutic approaches that may prove particularly effective for assembly disturbances. Complex I function and deficiency Complex I is embedded in the mitochondrial inner membrane where it oxidizes the NADH produced during glycolysis, fatty Brain 2012: 135; 12–22 | 13 acid oxidation and the Krebs cycle. In more detail, electrons extracted from NADH are funnelled to the electron carrier ubiquinone via a chain of iron-sulphur clusters, resulting in conformational changes that allow proton translocation across the mitochondrial inner membrane (Efremov et al., 2010). This proton translocation, also performed by complexes III and IV, results in a mitochondrial membrane potential used by complex V (ATP synthase) to generate ATP from ADP and inorganic phosphate (Fig. 1). Disturbances in the function of complex I can have various physiological consequences, such as disturbed ATP production, oxygen consumption and calcium homeostasis. In addition, it can cause accumulation of reactive oxygen species (Distelmaier et al., 2009) and lactic acid (Robinson, 2006), and induce apoptosis (Perier et al., 2005). Although there is no obvious genotype–phenotype correlation (Distelmaier et al., 2009), several disease phenotypes for complex I deficiency can be distinguished based on inheritance. Mitochondria have their own circular genome, which in humans measures 16 569 bp. In 1988, it first became clear that mitochondrial disorders can be caused by a point mutation or deletion in the mitochondrial genome and that the cell can harbour a mixture of healthy and mutated mitochondrial DNA, called heteroplasmy (Holt et al., 1988; Wallace et al., 1988). The thousands of copies of mitochondrial DNA are inherited via the mother and randomly Figure 1 The molecular basis and pathology of complex I deficiency. Left: Complex I is part of a system of five enzyme complexes (CI–CV) embedded in the mitochondrial inner membrane, which together perform oxidative phosphorylation. In this system, complex I oxidizes nicotinamide adenine dinucleotide (NADH) to transfer electrons to acceptor ubiquinone via a series of iron-sulphur (FeS) clusters. In turn, this leads to proton translocation across the mitochondrial inner membrane to maintain a proton gradient required for complex V to produce ATP. Complex I is assembled from nuclear subunits translated by cytosolic ribosomes (Ribo) and mitochondrial subunits translated by the mitochondrial ribosome (MitoRibo). Disturbances in the assembly and/or stability of the complex can result in reduced conversion of NADH to NAD + , reduced proton translocation, increased release of reactive oxygen species (ROS), and can ultimately lead to reduced ATP production and the accumulation of lactate. Deficiency of complex I can lead to various cellular abnormalities and apoptosis, which translates into a heterogeneous disease phenotype (right). Affected organs are primarily those with energy-demanding tissue, such as the nervous system, muscle, liver and kidneys. Complex I deficiency is generally an early onset, progressive multisystem disorder featuring severe neurological and muscular problems. 14 | Brain 2012: 135; 12–22 distributed to daughter cells during development in a process called segregation. These characteristics of mitochondrial DNA explain why disorders caused by mutations in the mitochondrial DNA generally feature a high prevalence of mitochondrial symptoms within one family and a high variability in clinical course. In contrast, mitochondrial deficiencies caused by nuclear DNA mutations generally have a much more severe phenotype with early onset. Mammalian complex I has seven mitochondrial genes (ND1–6 and ND4L) and 38 nuclear genes (Carroll et al., 2006). Mutations in mitochondrial genes are associated with maternally inherited complex I deficiency. The most prevalent pathologies associated with mutations in mitochondrial complex I genes are Leber’s hereditary optic neuropathy (OMIM 535 000), mitochondrial myopathy, encephalopathy, lactic acidosis and stroke-like episodes (OMIM 540 000) and Leigh syndrome (OMIM 256 000) (Mitchell et al., 2006). Leber’s hereditary optic neuropathy involves degeneration of retinal ganglion cells and their axons resulting in acute loss of vision. Age of onset is generally between the ages of 15 and 30 years, with males being affected five times more than females (Harding et al., 1995; Yu-Wai-Man et al., 2009). Mitochondrial myopathy, encephalopathy, lactic acidosis and stroke-like episodes is a clinically and genetically heterogeneous phenotype of a mostly maternally inherited neurological syndrome. It is characterized by epilepsy or dementia, often with additional neurological symptoms such as migraine or psychiatric problems, lactic acidosis (present in 94% of patients; Hirano and Pavlakis, 1994), and stroke-like episodes (hemianopia, hemiparesis, aphasia and hemineglect, etc.), associated with additional symptoms such as epileptic seizures, ataxia, migraine-like headaches, impaired vision or hearing, or disturbances in consciousness (Finsterer, 2009). Leigh syndrome is a devastating neurodegenerative disease (OMIM 256 000; Loeffen et al., 2000). Most of the cases typically present within the first 2 years of life with psychomotor retardation in combination with signs of brainstem or extrapyramidal dysfunction and lactic acidaemia, usually in a period of increased stress, such as infection (Rahman et al., 1996; Finsterer, 2008). Other symptoms include neurological symptoms (ophthalmoparesis, optic atrophy, ataxia, dysphagia, cranial nerve palsies, muscle weakness, hypotonia, dystonia, respiratory impairment, lethargy and polyneuropathy) whether or not in combination with dysmorphic features, endocrine abnormalities, hypertrichosis, short stature, cardiac abnormalities (hypertrophic or dilated cardiomyopathy) or gastrointestinal problems (diarrhoea), diabetes, vomiting, anaemia or renal problems. Death usually occurs within the first years of life as a consequence of respiratory failure caused by ongoing brainstem dysfunction, which can be accompanied by increasing muscle weakness (Finsterer, 2008). Mutations in nuclear genes show Mendelian inheritance. The majority (26%) of patients with mutations in nuclear complex I genes present with Leigh syndrome. Other phenotypes associated with mutations in nuclear complex I genes include neonatal cardiomyopathy with lactic acidosis, leucoencephalopathy and other undefined progressive or stable encephalomyopathies. Neonatal cardiomyopathy with lactic acidosis involves a relatively common early onset, progressive hypertrophic cardiomyopathy leading to death usually within the first year of life (Loeffen et al., 2000; Bugiani et al., 2004). Leucoencephalopathy has been described J. Nouws et al. with a progressive occurrence of large cavitations in subcortical white matter, accompanied by ventricular enlargement and macrocephaly. The neurological condition comprises involuntary movements and signs of brainstem involvement, developmental regression, failure to thrive and spasticity (Bugiani et al., 2004; Hoefs et al., 2010). Complex I assembly factors: a novel cause for disease Sequencing of the seven mitochondrial DNA-encoded and 38 nuclear DNA-encoded complex I genes could provide a genetic explanation for 550% of the patients. This made clear that the cause of many disease cases must be sought outside the structure of complex I. Prime suspects were complex I assembly factors, analogous to those identified for complex IV in the yeast model organism (Fontanesi et al., 2006). Assembly factors aid assembly of a complex without being part of the final structure. Although the lack of complex I in yeast initially hampered their identification, pioneering work in the fungus Neurospora crassa delivered the first two complex I assembly factors, called CIA30 and CIA84 (Kuffner et al., 1998). The human orthologue of CIA30, NDUFAF1, proved essential to human complex I assembly and mutations in the gene were linked to complex I deficiency (Vogel et al., 2005; Dunning et al., 2007). Lacking additional genetic pointers to go on, homozygosity mapping in consanguineous families was key to finding human complex I assembly factors. Some new factors were found simply by sequencing all candidate genes in homozygous regions (e.g. C20orf7 and NDUFAF4) (Sugiana et al., 2008; Saada et al., 2008). Additional clues for identifying new complex I disease genes have come from recent developments in high-throughput analysis of gene and protein function. One example is proteomics. A liquid chromatography–mass spectrometry-based method to profile protein interactions with complex I assembly intermediates delivered NDUFAF3 (Wessels et al., 2009), and simultaneous homozygosity mapping followed by sequencing implicated the NDUFAF3 gene in complex I deficiency (Saada et al., 2009). Additional proteomic strategies, such as blue native-polyacrylamide gel electrophoresis and tandem affinity purification, illustrated binding of NDUFAF3 with previously identified assembly factor NDUFAF4 from early to late stages of complex I assembly (Saada et al., 2009). Tandem affinity purification was combined with mass spectrometric analysis to find proteins binding to NDUFAF1, which provided the ECSIT and ACAD9 assembly factors (Vogel et al., 2007c; Nouws et al., 2010). Both factors were previously implicated in other cellular processes than OXPHOS (Kopp et al., 1999; Zhang et al., 2002; Xiao et al., 2003). ACAD9 mutations turn out to be an important cause for complex I deficiency, as recently three research groups identified pathogenic mutations in the ACAD9 gene in 10 patients (Haack et al., 2010; Nouws et al., 2010; Gerards et al., 2011). The examples above show the strength of combining homozygosity mapping with proteomic approaches to verify or direct identification of new assembly factors. A new class of complex I disease genes Another example is bioinformatics. Benefiting from the fact that yeast does not have complex I and other organisms do, subtractive genome analysis provided assembly factor NDUFAF2 (Ogilvie et al., 2005). This protein is a paralogue of complex I subunit NDUFA12 and is associated with a late-stage assembly intermediate. The NDUFAF2 gene proved an important source of disease-causing mutations associated with complex I deficiency (Ogilvie et al., 2005; Barghuti et al., 2008; Hoefs et al., 2009; Janssen et al., 2009; Calvo et al., 2010; Herzer et al., 2010). Innovations in the computation of large data sets allowed for more expansive, genome-wide bioinformatic approaches. Pagliarini et al. (2008) combined in-depth protein mass spectrometry, microscopy and machine learning to generate a compendium of 1098 mitochondrial genes, which was further used in conjunction with phylogenetic profiling to develop a list of 19 putative complex I disease-causing genes. A pathogenic mutation in C8orf38 was found after subsequent homozygosity mapping. High-throughput pooled sequencing in a complex I-deficient patient cohort identified mutations in both FOXRED1 and NUBPL (Calvo et al., 2010). NUBPL, also known as huInd1, plays a role in iron-sulphur cluster incorporation during early complex I assembly (Sheftel et al., 2009). A second patient harbouring mutations in FOXRED1 was reported shortly after (Fassone et al., 2010), but the exact function of the protein remains unclear. The role of assembly factors during complex I assembly Human complex I assembly has primarily been studied by investigating the accumulation of assembly intermediates either in patient cell lines or after inhibition of mitochondrial translation, and by tracing 35S or epitope labelled complex I subunits during the assembly process (Antonicka et al., 2003; Ugalde et al., 2004; Lazarou et al., 2007; Vogel et al., 2007a; Perales-Clemente et al., 2010). This has led to the identification of multiple assembly intermediates. For example, tracing the NDUFS3 subunit during assembly revealed at least six assembly intermediates (Vogel et al., 2007b). In addition, at least five entry points were recently identified for mitochondrial DNA-encoded subunits (PeralesClemente et al., 2010). Based on the temporal order of appearance and the composition of reported assembly intermediates a basic assembly scheme can be devised (Fig. 2, subcomplex numbers based on Vogel et al., 2007b). Briefly summarized, a complex of several core nuclear DNA-encoded subunits is formed and tethered to the mitochondrial membrane during early assembly (Fig. 2, subcomplexes 1, 2 and 3). In parallel, hydrophobic membrane complexes are formed and incorporated into the maturing complex (Fig. 2, at subcomplexes 4 and 5). Subsequent expansion of the complex includes addition of subunits from the dehydrogenase module (Fig. 2, subcomplex 6), resulting in fully assembled complex I (Fig. 2, complex 7). Altogether, nine assembly factors have been implicated in complex I deficiency in a short period of time (Fig. 2). Currently, the precise mechanism of action of most complex I assembly factors is unclear. An exception is NUBPL, which is required for the Brain 2012: 135; 12–22 | 15 incorporation of iron-sulphur clusters (Sheftel et al., 2009), present in six subunits (NDUFV1, NDUFV2, NDUFS1, NDUFS2, NDUFS7 and NDUFS8). Despite the lack of mechanistic data, the stages in which the other assembly factors operate can be derived from the accumulation of assembly intermediates upon their mutation or knockdown, and by examining their protein–protein interactions by affinity purification. The proposed involvement of each factor during assembly is summarized in the scheme in Fig. 2. 35S labelling of mitochondrial protein showed that mutations in C20orf7 lead to the accumulation of early membrane subcomplexes, suggesting that C20orf7 acts in early assembly (Sugiana et al., 2008). However, as C20orf7 mutations have also been implicated in combined complex I/complex IV deficiency, its role may not be exclusive to complex I assembly (Saada et al., 2011). NDUFAF1 and ACAD9 have been found in conjunction with assembly factor ECSIT, and NDUFAF1 was reported to associate with a number of complex I subunits (Dunning et al., 2007; Vogel et al., 2007c; Nouws et al., 2010). Knockdown of any of these assembly factors results in accumulation of subcomplexes 4 and 5 (Fig. 2), hinting towards a role in the incorporation of membrane subunits. Epitope tagging of assembly factors NDUFAF3 and NDUFAF4 revealed their association with each other and with assembly stages 3, 4, 5 and 6, indicating a role from early to late complex I assembly (Saada et al., 2009). NDUFAF2 is typically observed in an accumulated near holocomplex upon mutation of subunits NDUFV1 or NDUFS4 (Ogilvie et al., 2005, Vogel et al., 2007a), indicating that it is involved in late assembly or complex I stability. Putative associations of assembly factors C8orf38 and FOXRED1 with complex I subunits have not been studied. An additional protein, apoptosis inducing factor, has been implicated in complex I deficiency in mouse studies (Vahsen et al., 2004; Joza et al., 2005), but as mutations in human patients resulted in a combined complex III/IV deficiency and mitochondrial DNA depletion, its requirement for complex I assembly is as yet, ambiguous (Ghezzi et al., 2010). In summary, most identified assembly factors are involved in early assembly, more specifically the incorporation of hydrophobic membrane subunits (NDUFAF1—possibly in combination with ACAD9 and ECSIT, NDUFAF3 and NDUFAF4 and C20orf7). Apparently this is a process that requires careful coordination, akin to the incorporation of prosthetic groups during complex IV assembly (Fontanesi et al., 2006). The pathology of assembly factors Do mutations in complex I assembly factors result in a unique pathology? At first glance the symptoms listed in Table 1 are not distinct from what is observed for previously reported complex I deficiencies. It should be noted that making a distinction based on symptoms is complicated by possible differences in their classification between different case reports. In addition, the same mutation can lead to different clinical outcomes. For example, reported consanguineous siblings carrying ACAD9 and NDUFAF3 mutations may have had a similar age of onset and symptoms, 16 | Brain 2012: 135; 12–22 J. Nouws et al. Figure 2 The dawn of complex I assembly factors. The histogram (top) gives a historical overview of the cumulative number of unique mutations associated with complex I deficiency in nuclear DNA-encoded subunit genes (nDNA subunits), mitochondrial DNA-encoded subunit genes (mtDNA subunits) and assembly factors. Mitochondrial DNA mutations were included when the mutations were scored 510 by use of the Mitchell scoring table (Mitchell et al., 2006). The more recently published mutations were included in the chart when these were proven to be pathogenic by the creation of cybrids or they had to fulfil three of the four following criteria: (i) absence of the mutation in 5100 controls; (ii) presence of heteroplasmy; (iii) a highly conserved amino acid was changed; and (iv) the mutation segregated with disease. The mutations and the corresponding references are listed in Supplementary Table 1. Bottom: The proposed involvement of each disease-implicated assembly factor in the assembly process is indicated with arrows. Numbers of subcomplexes refer to those described in Vogel et al. (2007b). but siblings with the same NDUFAF4 mutation had a considerable difference in the development of symptoms. Also, mutations in the same gene can lead to different clinical outcomes. For example, one patient carrying a mutation in C20orf7 died after 7 days of high blood lactate level. Two siblings harbouring another mutation in C20orf7 are both in their 20s and diagnosed with Leigh syndrome. After puberty the progression of the disease stopped. A notable observation is the vanishing white matter reported for almost all patients with NDUFAF2 mutations. This brain anomaly has previously been reported for a mutation in a structural complex I subunit that is incorporated late in the assembly pathway (Pagniez-Mammeri et al., 2010), the stage in which NDUFAF2 is also active. Other gene–pathology relationships are less transparent. ACAD9 and NDUFAF1 were shown to be co-dependent and to be active in the same assembly stages. Mutations in either factor are associated with a high incidence of exercise intolerance and cardiomyopathy. In contrast, two other proteins known to interact in the assembly pathway are NDUFAF3 and NDUFAF4, Reported mutations N N Homozygous c.103delA (DT67) Homozygous c.103delA (DT68) Homozygous c.221G 4 A, exon skipping (DT16) Calvo, 2010 ND Homozygous c.749G 4 T; Gly250Val (5) Saada, 2009 NDUFAF4 ND less ND Homozygous c.194T 4 C; Leu65Pro (F511) Homozygous c.194T 4 C; Leu65Pro (F334) Homozygous c.194T 4 C; Leu65Pro (F528) ND ND Homozygous c.749G 4 T; Gly250Val (4) Homozygous c.296A 4 G; Gln99Arg (sibling) ND Homozygous c.749G 4 T; Gly250Val (3) ND ND Homozygous c.749G 4 T; Gly250Val (2) Pagliarini, 2008 Homozygous c.296A 4 G; Gln99Arg C8orf38 ND Homozygous c.592C 4 T; Leu159Phe (IV-7) Homozygous c.749G 4 T; Gly250Val (1) ND Homozygous c.592C 4 T; Leu159Phe (IV-11) Gerards, 2010 Saada, 2011 ND Homozygous c.719T 4 C; Leu229Pro ND ND Sugiana, 2008 C20orf7 N Homozygous c.9G 4 A:Trp3X Herzer, 2010 N Deletion of full sequence Janssen, 2009 N Homozygous c.1A 4 T:Met1Leu (Patient 2) Homozygous c.114C 4 G; p.Tyr38X N Homozygous c.1A 4 T:Met1Leu (Patient 1) Barghuti, 2008 Hoefs, 2009 N Homozygous c.182C 4 T; Arg45X 1 N N F F M M F M F F F M M M M M M F M F F M F F M 43% 67% 14% 14% 25% 32% 32% 26% 41% 45% 23% 53% ND 520%# 36% 14% 6% 36% 25% 26% 48% 36% 25% 38% 12% 24% 36% 40%# Term Term Term ND ND ND ND ND ND 36 ND ND 35 ND ND ND Term 38 Term ND ND Term ND Birth Birth Birth 7m 10m ND ND ND ND 12m 3y 3y 1d 4m 3m 6m 14m Birth 3m 8m 20m 12m 11m % Res Pregnancy Age of Protein Sex % CI activity duration onset detected Res CI activity in in muscle (weeks) fibroblasts Ogilvie, 2005 NDUFAF2 Dunning, 2007 CH: c.1001A 4 C;Thr207Pro, c.1140 A 4 G; Lys253Arg NDUFAF1 Publication 5d N7Y 18m N22m 34m N2,5y N6y N4,5y N7y 5y10m N29y N23y 7d 15m 14m 17m 27m 14m 12m 21m 2y 13y7m N20y Age of death Brain abnormalities Neurological symptoms Failure to thrive Symptoms Table 1 Clinical phenotypes of patients with mutations in complex I assembly factors Elevated alanine level 2 Exercise intolerance Motor development delay (continued) Lethargy Developmental delay Other Hepatomology Renal problems Hyperthrophic cardiomyopathy Other organ failure Respiratory disturbance Cyanotic Apneic Tachhypnea Respiratory problems Elevated CSF lactate level Elevated blood lactate level Metabolite levels Optic atrophy Hearing loss Ataxia Spasticity Hypotonia Dystonia Seizures Microcephaly Abnormal eye movements ND Homozygous c.365G 4 C; Arg122Pro (II-1) CH: c.2T 4 C;Met1Thr, ND c.365G 4 C; Arg122Pro (III-1) ND ND ND ND CH: c.130T 4 A; Phe44Ile; c.797G 4 A; Arg266Gln (I:B) CH: c.797G 4 A; Arg266Gln; c.1249C 4 T; Arg417Cys (II) CH: c.976G 4 A; Ala326Pro; c.1594C 4 T: Arg532Trp (III) F CH: c.380G 4 A; Arg127Gln, ND c.1405C 4 T; Arg469Trp (CV) CH: c.130T 4 A; Phe44Ile; c.797G 4 A; Arg266Gln (I:A) F ND Homozygous c.1594C 4 T; Arg532Trp (VII-11) F F M F M ND Homozygous c.1594C 4 T; Arg532Trp (VII-8) F ND F CH: c.187G 4 T; Glu63X, N c.1237G 4 A;Glu413Lys (II-1) Homozygous c.1594C 4 T; Arg532Trp (VII-6) F M M Y ND ND M M 38% 32% 50% 40% 38% 58% 53% 70% 9% 19% 33% 18% 39% 26% 13% 14% 9% 61% 7% 9% 37% 26% 40% 32% ND ND ND 39 w + 6d ND ND ND ND 35 Term Term 31 Term Term Term 34–38 34–38 34–38 N40y N38y N31y 6m N18y N10y N22y N8y 6m 4m 3m 3m 3m Birth Birth Birth 24h 2y 12y N5Y 46d Early CH N27y 4y 4y 4y 4m 8m Birth Birth 2y 3m 3w 1–3d 1–3d 1–3d Age of death Exercise intolerance Motor development delay Developmental delay Other Hepatomology Renal problems Hyperthrophic cardiomyopathy Other organ failure Respiratory disturbance Cyanotic Apneic Tachhypnea Respiratory problems Elevated alanine level Elevated CSF lactate level Elevated blood lactate level Metabolite levels Optic atrophy Hearing loss Ataxia Spasticity Hypotonia Dystonia Seizures Microcephaly Abnormal eye movements Brain abnormalities Neurological symptoms Failure to thrive Symptoms This table encompasses all published case reports. Boxes in black indicate the symptom was reported in the original article; white boxes indicate the symptom was absent or not tested in the original article. CI = complex 1; CH = compound heterozygous. ND = not determined; Residual CI activity in fibroblasts = complex I activity normalized for COX activity, percentage of lowest control value (values in bold are normalized to citrate synthase); Yellow box = percentage of control mean. Residual CI activity in muscle = complex I activity normalized for citrate synthase activity, percentage of lowest control value; # = determined by in gel activity; d = days; w = weeks; m = months; y = years. Brain abnormalities = on MRI or CT and/or diagnosed brain dysfunction. N = not dead, age at report date. 1 = Hemizygous for c.182C 4 T mutation, probably the other allele was deleted. Elevated alanine level = in blood; except for 2 = in urine. The patient number, as mentioned in the case report, is given in brackets. Haack, 2010 Gerards, 2011 Nouws, 2010 Homozygous c.1553G 4 A; Arg518His (I-1) Homozygous c.1054C 4 T;Arg352Trp Fassone, 2010 ACAD9 CH: c.694C 4 T; Gln232X, c.1289A 4 G; Asn430Ser ND F ND Homozygous c.229G 4 C; Gly77Arg (I-3) CH:Del exon 1-4 and c.166G 4 A; Gly56Arg, c.815-27T 4 C M ND Homozygous c.229G 4 C; Gly77Arg (I-2) F ND F Pregnancy Age of % Res Protein Sex % onset CI activity duration detected Res CI activity in in muscle (weeks) fibroblasts Homozygous c.229G 4 C; Gly77Arg (I-1) Reported mutations Calvo, 2010 FOXRED1 Calvo, 2010 NUBPL Saada, 2008 NDUFAF3 Publication Table 1. Continued Lethargy A new class of complex I disease genes Brain 2012: 135; 12–22 | 19 Figure 3 Age at onset and survival of complex I-deficient patients harbouring mutations in nuclear-encoded subunits and assembly factors. (A) Kaplan–Meier graph showing age of onset as percentage of patients affected, for patients harbouring mutations in nuclear-encoded subunits and assembly factors (subunits n = 82, assembly factors n = 45). (B) Kaplan–Meier survival analysis for patients harbouring mutations in nuclear-encoded subunits and assembly factors (subunits n = 89; assembly factors, n = 49). The mutations and corresponding references are listed in Supplementary Table 2. AF = assembly factors. yet apart from high lactate levels the symptoms deviate. Despite NUBPL’s seemingly crucial role in complex assembly, the patient carrying a mutation in the gene is 8 years old and suffering from encephalopathy but no other organs are affected. In summary, given the small number of mutations found it is not yet possible to relate an individual assembly factor gene to a specific clinical phenotype, nor to make a clear distinction from mutations in nuclear subunit genes. However, when we analyse mutations in assembly factor genes as a separate class we noted that disorders caused by mutations in assembly factors (versus nuclear complex I subunit genes) generally result in a significantly later age of death, which becomes prominent after 12 months of life (Fig. 3). Although the age of onset is reported to differ between complex I deficiency caused by mutation in nuclear versus mitochondrial complex I genes (Swalwell et al., 2011), we found no apparent difference in the age of onset between complex I deficiency caused by mutations in complex I nuclear subunit genes versus complex I assembly genes (Fig. 3). Clinical perspectives Current therapeutic strategies for complex I deficiency can relieve symptoms, but are unable to cure or even delay the progress of the disease. General approaches include administration of vitamins and cofactors, such as different forms of ubiquinone (Q10), even though beneficial effects are unclear because proper clinical trials are scarce (Chinnery et al., 2006; Glover et al., 2010; Kerr, 2010). Fortunately several encouraging new approaches are being developed, some of which may prove particularly useful for the treatment of complex I deficiency caused by disturbances in the assembly process. The assembly process can be viewed as a multistep reaction that involves input of subunits, catalysis by assembly factors and output of a holoenzyme. Mutations in assembly factors generally slow down or halt the reaction even though the subunits are without error. With this notion in mind, to restore assembly, one could either improve the function of any residual mutated assembly factor or increase the flow of substrates into the 20 | Brain 2012: 135; 12–22 assembly ‘reaction’. Of note, the success of such strategies will depend on the relative contribution of the assembly factor to the assembly process and the functional impact of the mutation. Stabilization of assembly factors can be achieved by targeted administration of cofactors. For example, a high dosage (300 mg/day) of riboflavin increased complex I activity and improved the clinical condition of patients with the ACAD9 mutation (Gerards et al., 2011). Furthermore, riboflavin was reported to stabilize the FAD group in complex I assembly protein, apoptosis inducing factor (Ghezzi et al., 2010). Likewise, this strategy has been reported to work for destabilized subunits, as the effects of a mutation of NDUFV1 could be alleviated by riboflavin supplementation (Benit et al., 2001). Increasing the amount of substrate (the subunits) to partly restore assembly is another promising strategy. Activation of PPAR (peroxisome proliferator-activated receptor) and PGC-1 transcriptional pathways led to increased mitochondrial biogenesis and improved mitochondrial physiology in cellular models for OXPHOS deficiency (Srivastava et al., 2007). More importantly, PGC-1 overexpression led to a significant improvement in endurance and healthy life span of a mouse knockout of complex IV assembly factor COX10 (Wenz et al., 2008). Administration of PPAR panagonist bezafibrate to the diet of these mice had a similar effect. As another example, overexpression of transcriptional activator NF-Y could partially rescue complex IV deficiency caused by mutation in assembly factor SURF1 by increasing complex IV expression (Fontanesi et al., 2008). Metabolic sensor kinases such as metabolic sensor kinase mTOR can also induce mitochondrial biogenesis (Cunningham et al., 2007). Recently, D’Antona et al. (2010) showed that mTOR stimulation with branched chain amino acids elevated mitochondrial biogenesis in middle-aged mice and up-regulated the reactive oxygen species defence mechanism. The quality control system, which includes molecular chaperones such as heat shock proteins and the ubiquitin proteasome, plays a key role in certain neurodegenerative diseases and cancer. Prevention of aggregation of misfolded proteins via small molecular regulators, chemical chaperones or neutraceuticals provides therapeutic options for treatment of Alzheimer’s disease and Parkinson’s disease (Wisniewski and Sadowski, 2008; Ali et al., 2010; Rose et al., 2011). Likewise, a similar approach to prevent aggregation of assembly intermediates may prove a useful tool to treat mitochondrial diseases caused by mutations in assembly factors. A direct link between protein aggregation and disease pathology has not yet been established for complex I deficiency. However, disturbances in mitochondrial protein quality control have been implicated in respiratory deficiency. For example, mutations in the m-AAA protease component AFG3L2 lead to respiratory deficiency and spastic paraplegia (Di Bella et al., 2010). Conclusion The rapid emergence of complex I assembly factors has had several implications. It provided a genetic solution for part of the thus far unexplained disease cases, aiding diagnosis and prevention. The recent identification of multiple assembly factors working in similar assembly stages has helped to direct future research J. Nouws et al. into the molecular basis of disease. By analogy to complex IV for which 420 assembly factors aid assembly of a 13 subunit complex, 10–20 new complex I assembly factors are expected to be found in the next couple of years. This search is greatly facilitated by implementation of technical novelties, such as high-throughput bioinformatic screening and whole genome sequencing. Although highly desirable, the clinical heterogeneity of complex I deficiency may preclude a general therapeutic approach. Most likely tailored combinations of approaches will provide the most effective personalized medicine. Several therapeutic options are being developed to alleviate disturbed complex I biogenesis. A prerequisite to further develop these approaches is detailed mechanistic knowledge of the molecular basis of disease. Therefore, it is of the utmost importance to accompany the association of new mutations with disease by detailed functional analysis of the involved assembly factor. Acknowledgements The authors would like to thank Thatjana Gardeitchik for her help with statistical analysis. Funding Netherlands Organization for Scientific Research (863.10.018 to R.O.V.). Supplementary material Supplementary material is available at Brain online. References Antonicka H, Ogilvie I, Taivassalo T, Anitori RP, Haller RG, Vissing J, et al. Identification and characterization of a common set of complex I assembly intermediates in mitochondria from patients with complex I deficiency. J Biol Chem 2003; 278: 43081–8. Ali YO, Kitay BM, Zhai RG. Dealing with misfolded proteins: examining the neuroprotective role of molecular chaperones in neurodegeneration. Molecules 2010; 15: 6859–87. D’Antona G, Ragni M, Cardile A, Tedesco L, Dossena M, Bruttini F, et al. Branched-chain amino acid supplementation promotes survival and supports cardiac and skeletal muscle mitochondrial biogenesis in middle-aged mice. Cell Metab 2010; 12: 362–72. Barghuti F, Elian K, Gomori JM, Shaag A, Edvardson S, Saada A, et al. The unique neuroradiology of complex I deficiency due to NDUFA12L defect. Mol Genet Metab 2008; 94: 78–82. Benit P, Chretien D, Kadhom N, de Lonlay-Debeney P, Cormier-Daire V, Cabral A, et al. Large-scale deletion and point mutations of the nuclear NDUFV1 and NDUFS1 genes in mitochondrial complex I deficiency. Am J Hum Genet 2001; 68: 1344–52. Bugiani M, Invernizzi F, Alberio S, Briem E, Lamantea E, Carrara F, et al. Clinical and molecular findings in children with complex I deficiency. Biochim Biophys Acta 2004; 1659: 136–47. Calvo SE, Tucker EJ, Compton AG, Kirby DM, Crawford G, Burtt NP, et al. High-throughput, pooled sequencing identifies mutations in A new class of complex I disease genes NUBPL and FOXRED1 in human complex I deficiency. Nat Genet 2010; 42: 851–8. Carroll J, Fearnley IM, Skehel JM, Shannon RJ, Hirst J, Walker JE. Bovine complex I is a complex of forty-five different subunits. J Biol Chem 2006; 281: 32724–27. Chinnery P, Majamaa K, Turnbull D, Thorburn D. Treatment for mitochondrial disorders. Cochrane Database Syst Rev 2006, Issue 1. Art. No.: CD004426. doi:10.1002/14651858.CD004426.pub2. Cunningham JT, Rodgers JT, Arlow DH, Vazquez F, Mootha VK, Puigserver P. mTOR controls mitochondrial oxidative function through a YY1-PGC-1alpha transcriptional complex. Nature 2007; 450: 736–40. Di Bella D, Lazzaro F, Brusco A, Plumari M, Battaglia G, Pastore A, et al. Mutations in the mitochondrial protease gene AFG3L2 cause dominant hereditary ataxia SCA28. Nat Genet 2010; 42: 313–21. Distelmaier F, Koopman WJ, van den Heuvel LP, Rodenburg RJ, Mayatepek E, Willems PH, et al. Mitochondrial complex I deficiency: from organelle dysfunction to clinical disease. Brain 2009; 132: 833–42. Dunning CJ, McKenzie M, Sugiana C, Lazarou M, Silke J, Connelly A, et al. Human CIA30 is involved in the early assembly of mitochondrial complex I and mutations in its gene cause disease. EMBO J 2007; 26: 3227–37. Eckert A, Schulz KL, Rhein V, Gotz J. Convergence of amyloid-beta and tau pathologies on mitochondria in vivo. Mol Neurobiol 2010; 41: 107–14. Efremov RG, Baradaran R, Sazanov LA. The architecture of respiratory complex I. Nature 2010; 465: 441–45. Fassone E, Duncan AJ, Taanman JW, Pagnamenta AT, Sadowski MI, Holand T, et al. FOXRED1, encoding a FAD-dependent oxidoreductase complex-I specific molecular chaperone, is mutated in infantileonset mitochondrial encephalopathy. Hum Mol Genet 2010; 19: 4837–47. Finsterer J. Leigh and Leigh-like syndrome in children and adults. Pediatr Neurol 2008; 39: 223–35. Finsterer J. Management of mitochondrial stroke-like-episodes. Eur J Neurol 2009; 16: 1178–84. Fontanesi F, Jin C, Tzagoloff A, Barrientos A. Transcriptional activators HAP/NF-Y rescue a cytochrome c oxidase defect in yeast and human cells. Hum Mol Genet 2008; 17: 775–88. Fontanesi F, Soto IC, Horn D, Barrientos A. Assembly of mitochondrial cytochrome c-oxidase, a complicated and highly regulated cellular process. Am J Physiol Cell Physiol 2006; 291: C1129–47. Gerards M, van den Bosch BJ, Danhauser K, Serre V, van Weeghel M, Wanders RJ, et al. Riboflavin-responsive oxidative phosphorylation complex I deficiency caused by defective ACAD9: new function for an old gene. Brain 2011; 134: 210–9. Gerards M, Sluiter W, van den Bosch BJ, de Wit LE, Calis CM, Frentzen M, et al. Defective complex I assembly due to C20orf7 mutations as a new cause of Leigh syndrome. J Med Genet 2010; 47: 507–12. Ghezzi D, Sevrioukova I, Invernizzi F, Lamperti C, Mora M, D’Adamo P, et al. Severe X-linked mitochondrial encephalomyopathy associated with a mutation in apoptosis-inducing factor. Am J Hum Genet 2010; 86: 639–49. Glover EI, Martin J, Maher A, Thornhill RE, Moran GR, Tarnopolsky MA. A randomized trial of coenzyme Q10 in mitochondrial disorders. Muscle Nerve 2010; 42: 739–48. Haack TB, Danhauser K, Haberberger B, Hoser J, Strecker V, Boehm D, et al. Exome sequencing identifies ACAD9 mutations as a cause of complex I deficiency. Nat Genet 2010; 42: 1131–4. Harding AE, Sweeney MG, Govan GG, Riordan-Eva P. Pedigree analysis in Leber hereditary optic neuropathy families with a pathogenic mtDNA mutation. Am J Hum Genet 1995; 57: 77–86. Herzer M, Koch J, Prokisch H, Rodenburg R, Rauscher C, Radauer W, et al. Leigh disease with brainstem involvement in complex I deficiency due to assembly factor NDUFAF2 defect. Neuropediatrics 2010; 41: 30–4. Brain 2012: 135; 12–22 | 21 Hirano M, Pavlakis SG. Mitochondrial myopathy, encephalopathy, lactic acidosis, and strokelike episodes (MELAS): current concepts. J Child Neurol 1994; 9: 4–13. Hoefs SJ, Dieteren CE, Rodenburg RJ, Naess K, Bruhn H, Wibom R, et al. Baculovirus complementation restores a novel NDUFAF2 mutation causing complex I deficiency. Hum Mutat 2009; 30: E728–36. Hoefs SJ, Skjeldal OH, Rodenburg RJ, Nedregaard B, van Kaauwen EP, Spiekerkotter U, et al. Novel mutations in the NDUFS1 gene cause low residual activities in human complex I deficiencies. Mol Genet Metab 2010; 100: 251–6. Holt IJ, Harding AE, Morgan-Hughes JA. Deletions of muscle mitochondrial DNA in patients with mitochondrial myopathies. Nature 1988; 331: 717–9. Janssen RJ, Distelmaier F, Smeets R, Wijnhoven T, Ostergaard E, Jaspers NG, et al. Contiguous gene deletion of ELOVL7, ERCC8 and NDUFAF2 in a patient with a fatal multisystem disorder. Hum Mol Genet 2009; 18: 3365–74. Janssen R, Smeitink J, Smeets R, van Den Heuvel L. CIA30 complex I assembly factor: a candidate for human complex I deficiency? Hum Genet 2002; 110: 264–70. Joza N, Oudit GY, Brown D, Bénit P, Kassiri Z, Vahsen N, et al. Muscle-specific loss of apoptosis- inducing factor leads to mitochondrial dysfunction, skeletal muscle atrophy, and dilated cardiomyopathy. Mol Cell Biol 2005; 25: 10261–72. Kerr DS. Treatment of mitochondrial electron transport chain disorders: a review of clinical trials over the past decade. Mol Genet Metab 2010; 99: 246–55. Kopp E, Medzhitov R, Carothers J, Xiao C, Douglas I, Janeway CA, et al. ECSIT is an evolutionarily conserved intermediate in the Toll/IL-1 signal transduction pathway. Genes Dev 1999; 13: 2059–71. Kuffner R, Rohr A, Schmiede A, Krull C, Schulte U. Involvement of two novel chaperones in the assembly of mitochondrial NADH: Ubiquinone oxidoreductase (complex I). J Mol Biol 1998; 283: 409–17. Lazarou M, McKenzie M, Ohtake A, Thorburn DR, Ryan MT. Analysis of the assembly profiles for mitochondrial- and nuclear-DNA-encoded subunits into complex I. Mol Cell Biol 2007; 27: 4228–37. Loeffen JL, Smeitink JA, Trijbels JM, Janssen AJ, Triepels RH, Sengers RC, et al. Isolated complex I deficiency in children: clinical, biochemical and genetic aspects. Hum Mutat 2000; 15: 123–34. Mitchell AL, Elson JL, Howell N, Taylor RW, Turnbull DM. Sequence variation in mitochondrial complex I genes: mutation or polymorphism? J Med Genet 2006; 43: 175–9. Mootha VK, Lindgren CM, Eriksson KF, Subramanian A, Sihag S, Lehar J, et al. PGC-1alpha-responsive genes involved in oxidative phosphorylation are coordinately downregulated in human diabetes. Nat Genet 2003; 34: 267–73. Nouws J, Nijtmans L, Houten SM, van den Brand M, Huynen M, Venselaar H, et al. Acyl-CoA dehydrogenase 9 is required for the biogenesis of oxidative phosphorylation complex I. Cell Metab 2010; 12: 283–94. Ogilvie I, Kennaway NG, Shoubridge EA. A molecular chaperone for mitochondrial complex I assembly is mutated in a progressive encephalopathy. J Clin Invest 2005; 115: 2784–92. Pagliarini DJ, Calvo SE, Chang B, Sheth SA, Vafai SB, Ong SE, et al. A mitochondrial protein compendium elucidates complex I disease biology. Cell 2008; 134: 112–23. Pagniez-Mammeri H, Landrieu P, Legrand A, Slama A. Leukoencephalopathy with vanishing white matter caused by compound heterozygous mutations in mitochondrial complex I NDUFS1 subunit. Mol Genet Metab 2010; 101: 297–8. Perales-Clemente E, Fernández-Vizarra E, Acı́n-Pérez R, Movilla N, Bayona-Bafaluy MP, Moreno-Loshuertos R, et al. Five entry points of the mitochondrially encoded subunits in mammalian complex I assembly. Mol Cell Biol 2010; 30: 3038–47. Perier C, Tieu K, Guegan C, Caspersen C, Jackson-Lewis V, Carelli V, et al. Complex I deficiency primes Bax-dependent neuronal apoptosis 22 | Brain 2012: 135; 12–22 through mitochondrial oxidative damage. Proc Natl Acad Sci USA 2005; 102: 19126–31. Rahman S, Blok RB, Dahl HH, Danks DM, Kirby DM, Chow CW, et al. Leigh syndrome: clinical features and biochemical and DNA abnormalities. Ann Neurol 1996; 39: 343–51. Robinson BH. Lactic acidemia and mitochondrial disease. Mol Genet Metab 2006; 89: 3–13. Rose JM, Novoselov SS, Robinson PA, Cheetham ME. Molecular chaperone-mediated rescue of mitophagy by a Parkin RING1 domain mutant. Hum Mol Genet 2011; 20: 16–27. Saada A, Edvardson S, Rapoport M, Shaag A, Amry K, Miller C, et al. C6ORF66 is an assembly factor of mitochondrial complex I. Am J Hum Genet 2008; 82: 32–8. Saada A, Edvardson S, Shaag A, Chung WK, Segel R, Miller C, et al. Combined OXPHOS complex I and IV defect, due to mutated complex I assembly factor C20ORF7. J Inherit Metab Dis 2011, Advance Access published on May 24, 2011, doi: 10.1007/s10545-011-9348-y. Saada A, Vogel RO, Hoefs SJ, van den Brand MA, Wessels HJ, Willems PH, et al. Mutations in NDUFAF3 (C3ORF60), encoding an NDUFAF4 (C6ORF66)-interacting complex I assembly protein, cause fatal neonatal mitochondrial disease. Am J Hum Genet 2009; 84: 718–27. Scaglia F, Towbin JA, Craigen WJ, Belmont JW, Smith EO, Neish SR, et al. Clinical spectrum, morbidity, and mortality in 113 pediatric patients with mitochondrial disease. Pediatrics 2004; 114: 925–31. Sheftel AD, Stehling O, Pierik AJ, Netz DJ, Kerscher S, Elsasser HP, et al. Human ind1, an iron-sulfur cluster assembly factor for respiratory complex I. Mol Cell Biol 2009; 29: 6059–73. Skladal D, Halliday J, Thorburn DR. Minimum birth prevalence of mitochondrial respiratory chain disorders in children. Brain 2003; 126: 1905–12. Srivastava S, Barrett JN, Moraes CT. PGC-1alpha/beta upregulation is associated with improved oxidative phosphorylation in cells harboring nonsense mtDNA mutations. Hum Mol Genet 2007; 16: 993–1005. Sugiana C, Pagliarini DJ, McKenzie M, Kirby DM, Salemi R, buAmero KK, et al. Mutation of C20orf7 disrupts complex I assembly and causes lethal neonatal mitochondrial disease. Am J Hum Genet 2008; 83: 468–78. Swalwell H, Kirby DM, Blakely EL, Mitchell A, Salemi R, Sugiana C, et al. Respiratory chain complex I deficiency caused by mitochondrial DNA mutations. Eur J Hum Genet 2011; 19: 769–75. Thorburn DR. Mitochondrial disorders: prevalence, myths and advances. J Inherit Metab Dis 2004; 27: 349–62. Ugalde C, Vogel R, Huijbens R, Van Den Heuvel B, Smeitink J, Nijtmans L. Human mitochondrial complex I assembles through the J. Nouws et al. combination of evolutionary conserved modules: a framework to interpret complex I deficiencies. Hum Mol Genet 2004; 13: 2461–72. Vahsen N, Candé C, Brière JJ, Bénit P, Joza N, Larochette N, et al. AIF deficiency compromises oxidative phosphorylation. EMBO J 2004; 23: 4679–89. Vogel RO, van den Brand MA, Rodenburg RJ, van den Heuvel LP, Tsuneoka M, Smeitink JA, et al. Investigation of the complex I assembly chaperones B17.2L and NDUFAF1 in a cohort of CI deficient patients. Mol Genet Metab 2007a; 91: 176–82. Vogel RO, Dieteren CE, van den Heuvel LP, Willems PH, Smeitink JA, Koopman WJ, et al. Identification of mitochondrial complex I assembly intermediates by tracing tagged NDUFS3 demonstrates the entry point of mitochondrial subunits. J Biol Chem 2007b; 282: 7582–90. Vogel RO, Janssen RJ, van den Brand MA, Dieteren CE, Verkaart S, Koopman WJ, et al. Cytosolic signaling protein Ecsit also localizes to mitochondria where it interacts with chaperone NDUFAF1 and functions in complex I assembly. Genes Dev 2007c; 21: 615–24. Vogel RO, Janssen RJ, Ugalde C, Grovenstein M, Huijbens RJ, Visch HJ, et al. Human mitochondrial complex I assembly is mediated by NDUFAF1. FEBS J 2005; 272: 5317–26. Wallace DC, Singh G, Lott MT, Hodge JA, Schurr TG, Lezza AM, et al. Mitochondrial DNA mutation associated with Leber’s hereditary optic neuropathy. Science 1988; 242: 1427–30. Wenz T, Diaz F, Spiegelman BM, Moraes CT. Activation of the PPAR/ PGC-1alpha pathway prevents a bioenergetic deficit and effectively improves a mitochondrial myopathy phenotype. Cell Metab 2008; 8: 249–56. Wessels HJ, Vogel RO, van den Heuvel L, Smeitink JA, Rodenburg RJ, Nijtmans LG, et al. LC-MS/MS as an alternative for SDS-PAGE in blue native analysis of protein complexes. Proteomics 2009; 9: 4221–8. Winklhofer KF, Haass C. Mitochondrial dysfunction in Parkinson’s disease. Biochim Biophys Acta 2010; 1802: 29–44. Wisniewski T, Sadowski M. Preventing beta-amyloid fibrillization and deposition: beta-sheet breakers and pathological chaperone inhibitors. BMC Neurosci 2008; 9 (Suppl. 2): S5. Xiao C, Shim JH, Kluppel M, Zhang SS, Dong C, Flavell RA, et al. Ecsit is required for Bmp signaling and mesoderm formation during mouse embryogenesis. Genes Dev 2003; 17: 2933–49. Yu-Wai-Man P, Griffiths PG, Hudson G, Chinnery PF. Inherited mitochondrial optic neuropathies. J Med Genet 2009; 46: 145–58. Zhang J, Zhang W, Zou D, Chen G, Wan T, Zhang M, et al. Cloning and functional characterization of ACAD-9, a novel member of human acyl-CoA dehydrogenase family. Biochem Biophys Res Commun 2002; 297: 1033–42.