* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download 1 Lecture Pharmacology Dr. nahlah Pharmacology of the Autonomic
Survey
Document related concepts
Discovery and development of proton pump inhibitors wikipedia , lookup
Cannabinoid receptor antagonist wikipedia , lookup
Discovery and development of beta-blockers wikipedia , lookup
Discovery and development of angiotensin receptor blockers wikipedia , lookup
NK1 receptor antagonist wikipedia , lookup
Pharmaceutical industry wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Prescription costs wikipedia , lookup
Pharmacognosy wikipedia , lookup
Drug interaction wikipedia , lookup
Neuropharmacology wikipedia , lookup
Nicotinic agonist wikipedia , lookup
Transcript
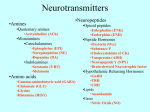
1 Lecture Pharmacology Pharmacology of the Autonomic Nervous System Lecture Outline Dr. nahlah 16-10-2016 I. Introduction II. Anatomy III. Biochemistry a. Neurotransmitters b. Synthesis and storage c. Release of acetylcholine d. Termination of action of acetylcholine IV. Acetylcholine Receptors a. Muscarinic receptors b. Nicotinic receptor V. Cholinergic Agonists a. Direct-acting cholinergic agonists. b. Indirect-acting cholinergic agonists VI. Cholinergic Antagonists VII. Skeletal Muscle Relaxants Learning Objectives: 1) An understanding of the clinical physiology of the cholinergic nervous system a. Neurotransmitters involved in major central and peripheral neuronal pathways b. Synthesis and metabolism of acetylcholine (Ach) 2) An understanding of muscarinic agonists and antagonists, and cholinesterase inhibitors 3) An understanding of agents that stimulate or relax skeletal muscle, including the cholinergic neuromuscular agonists and antagonists. I. Introduction The nervous system controls all the major functions of the body. It is divided into central and peripheral nervous systems. The peripheral nervous system includes the somatic and autonomic nervous systems which control voluntary and involuntary functions respectively. The ANS controls the vegetative functions of the body. These include functions like circulation, respiration, digestion and the maintenance of body temperature. Organization of the nervous system. 2 II. Anatomy Parasympathetic neurons: The parasympathetic preganglionic fibers arise from cranial nerves III (oculomotor), VII (facial), IX (glossopharyngeal), and X (vagus), as well as from the sacral region (S2 to S4) of the spinal cord and synapse in ganglia near or on the effector organs. [Note: The vagus nerve accounts for 90% of preganglionic parasympathetic fibers in the body. Postganglionic neurons from this nerve innervate most of the organs in the thoracic and abdominal cavity. Schematic diagram of the sympathetic and parasympathetic divisions of the peripheral autonomic nervous system III. Biochemistry a. Neurotransmitters Acetylcholine (ACh) is the primary transmitter in all autonomic ganglia and at the synapses between parasympathetic postganglionic neurons and their effector cells. It is the transmitter at postganglionic sympathetic neurons to the thermoregulatory sweat glands. It is also the primary transmitter at the somatic (voluntary) skeletal muscle neuromuscular junction. 3 Simplified summary of parasympathetic, sympathetic somatic innervations b. Synthesis and storage Acetylcholine is synthesized in the nerve terminal by the enzyme choline acetyltransferase (ChAT) from acetyl-CoA and choline ( rate-limiting step). ACh is actively transported into its vesicles for storage. c. Release of acetylcholine—Release of transmitter stores from vesicles requires the entry of calcium through calcium channels This interaction results in fusion of the membranes of the vesicles with the nerve-ending membranes, the opening of a pore to the extracellular space, and the release of the stored transmitter. d. Termination of action of acetylcholine— The action of acetylcholine in the synapse is normally terminated by metabolism to acetate and choline by the enzyme acetylcholinesterase in the synaptic cleft. Inhibition of acetylcholinesterase is an important therapeutic (and potentially toxic) effect of several drugs. Characteristics of transmitter synthesis, storage, release, and termination of action at cholinergic nerve terminals IV. Acetylcholine Receptors(cholinergic) The most important classification depends on their responsiveness to the agonist drugs, muscarine and nicotine. a. Muscarinic receptors(M) There are at least 5 subtypes of muscarinic receptors, referred to as M1, M2, M3, M4 and M5. However, only M1, M2, and M3 receptors have been functionally characterized They mediate their effects through G proteins coupled to phospholipase C,or to potassium channels. b. Nicotinic receptor(N) There are at least two subtypes of nicotinic receptors, referred to as NM and NN. The NM receptor mediates skeletal muscle stimulation, while the NN receptor mediates 4 stimulation of the ganglia of the autonomic nervous system.The nicotinic receptor functions as a ligand-gated ion channel. Actions of sympathetic and parasympathetic nervous systems on effector organs V. Cholinergic Agonists Drugs with acetylcholine-like effects (cholinomimetics) consist of 2 major subgroups on the basis of their mode of action (ie, whether they act directly at the acetylcholine receptor or indirectly through inhibition of cholinesterase). Drugs in the direct-acting subgroup are further subdivided on the basis of their spectrum of action (ie, whether they act on muscarinic or nicotinic cholinoceptors). Subgroups of cholinomimetic drugs. a. Direct-acting cholinergic agonists. Cholinergic agonists mimic the effects of ACh by binding directly to cholinoceptors (muscarinic or nicotinic). These agents may be broadly classified into two groups: 1) Choline esters, which include ACh and synthetic esters of choline, such as carbachol and bethanechol. 2) naturally occurring alkaloids, such as nicotineand pilocarpine 5 1) Choline esters Acetylcholine may be considered the prototype that acts directly at both muscarinic and nicotinic receptors. . it lacks therapeutic importance because of its multiplicity of actions (leading to diffuse effects) and its rapid inactivation by the cholinesterases. ACh has both muscarinic and nicotinic activity The pharmacological effects of acetylcholine. Bethanechol Is structurally related to ACh. It is not hydrolyzed by AChE due to the esterification of carbamic acid. It lacks nicotinic actions but does have strong muscarinic activity. It has about a 1-hour duration of action. Therapeutic applications: 1) In urologic treatment, to stimulate the atonic bladder, particularly in postpartum or postoperative, nonobstructive urinary retention. 2) Bethanechol may also be used to treat neurogenic atony as well as megacolon. Adverse effects: Bethanechol causes the effects of generalized cholinergic stimulation These include sweating, salivation, flushing, decreased blood pressure, nausea, abdominal pain, diarrhea, and bronchospasm. Carbachol (carbamylcholine) Is an ester of carbamic acid Has both muscarinic and nicotinic actions. It is poor substrate for AChE. It is biotransformed by other esterases, but at a much slower rate. Therapeutic uses: Because of its high potency, receptor nonselectivity, and relatively long duration of action, carbacholis rarely used therapeutically except in the eye as a miotic agent to treat glaucoma by causing pupillary contraction and a decrease in intraocular pressure. Adverse effects: At doses used ophthalmologically, little or no side effects occur due to lack of systemic penetration (quaternary amine) 2) naturally occurring alkaloids: Pilocarpine The alkaloid pilocarpineis a tertiary amine and is stable to hydrolysis by AChE. Compared with ACh and its derivatives, it is far less potent but is uncharged and can penetrate the CNS at therapeutic doses. It exhibits muscarinic activity 6 Therapeutic uses: 1- In glaucoma: - Pilocarpine is the drug of choice in the emergency lowering of intraocular pressure of both narrow-angle and wide-angle glaucoma. 2- Pilocarpine available as tablet used for treatment of xerostomia (dry mouth), a- After irradiation of head & neck. b- Sjogren's syndrome. Actions of pilocarpine and atropine on the iris and ciliary muscle of the eye. Adverse effects: blurred vision night blindness brow ache. Poisoning with this agent is characterized by exaggeration of various parasympathetic effects, including profuse sweating (diaphoresis) and salivation. Parenteral atropine, at doses that can cross the blood–brain barrier, is administered to counteract the toxicity of pilocarpine b. Indirect-acting cholinergic agonists (Anticholinesterase Agents) AChE is an enzyme that specifically cleaves ACh to acetate and choline. Inhibitors of AChE (anticholinesterase agents or cholinesterase inhibitors) indirectly provide a cholinergic action by preventing the degradation of ACh. This results in an accumulation of ACh in the synaptic space. 7 a- Indirect acting Cholinesterase inhibitor, Reversible: 1- Short acting: Edrophonium: Used parentrally ( by injection). - Short duration of action (10-20 minutes). Therapeutic uses: 1- Drug of choice for diagnosing Myasthenia gravis (MG). 2- Used to differentiate M.G (which is weakness due to sever disease or inadequate anticholinesterase treatment) from cholinergic crisis (which is weakness due to over treatment with anticholinesterase). 2- Intermediate & long acting: Physostigmine Its duration of action is about 30 minutes to 2 hours, and it is considered an intermediate-acting agent. Physostigminecan enter and stimulate the cholinergic sites in the CNS. Therapeutic uses: 1) The drug increases intestinal and bladder motility, which serves as its therapeutic action in atony of either organ. 2) Physostigmineis also used in the treatment of overdoses of drugs with anticholinergic actions, such as atropine. Adverse effects: on the CNS may lead to convulsions when high doses are used. Bradycardia and a fall in cardiac output may also occur. Inhibition of AChE at the skeletal NMJ causes the accumulation of ACh and, ultimately, results in paralysis of skeletal muscle. Neostigmine It is more polar, is absorbed poorly from the GI tract, and does not enter the CNS. Its effect on skeletal muscle is greater than that of physostigmine. Therapeutic uses: 1) To stimulate the bladder and GI tract. 2) Antidote for competitive neuromuscular-blocking agents. 3) To manage symptoms of myasthenia gravis. Adverse effects: salivation, flushing, decreased blood pressure nausea, abdominal pain, diarrhea Bronchospasm Neostigmineis contraindicated when intestinal or urinary bladder obstruction is present. Pyridostigmine and ambenonium Used in the chronic management of myasthenia gravis. Their durations of action are intermediate (3 to 6 hours and 4 to 8 hours, respectively) 8 - Indirect acting Cholinesterase inhibitor, Reversible used to treat Alzheimer’s disease : Patients with Alzheimer’s disease have a deficiency of cholinergic neurons in the CNS. This observation led to the development of anticholinesterases as possible remedies for the loss of cognitive function. Tacrine was the first to become available, but it has been replaced by others because of its hepatotoxicity. Donepezi, Rivastigmine, and galantamine: Despite the ability to delay the progression of Alzheimer’s disease, none can stop its progression. adverse effect: GI distress. b- Indirect acting Cholinesterase inhibitor, Irreversible (Very long acting): Isoflurophate & Echothiophate - These drugs are used topically in the eye for the chronic treatment of open-angle glaucoma. The effects may last for up to one week after a single administration. A number of synthetic organophosphate compounds. Used in agriculture or pesticides & insecticides. Many of these drugs are extremely toxic & were developed by the military as nerve gases. Of these substances GA (Tabun); GB (Sarin) and GD (Soman) called Nerve gases, although they are volatile liquids. Poisoning with Cholinesterase inhibitors (Organophosphorous poisoning) Mechanism of action: - An organophosphate that covalently binds to a serine-OH at the active site of Achesterase. Once this occurs, the enzyme is permanently inactivated, and restoration of Achesterase activity (recovery) requires the synthesis of new enzyme molecules, this process may take weeks, although clinical recovery is usually evident within days. Clinical Features of Organophosphorous poisoning: 1- Excessive salivation, nausea, vomiting. abdominal cramps, diarrhea & lacrimation. 2. Excessive bronchial secretion, bronchoconstriction, cough, wheezing and dyspnea. 3. Bradycardia. 4. Involuntary micturation. 5. Sweating . 6. Muscle weakness, twitching. 7. Meiosis (small size pupil) , anxiety, headache, convulsion, respiration failure. - Death is due to actions on CNS, paralysis of respiratory m. and excessive bronchial secretion & constriction. 9 Treatment of Organophosphorous poisoning: 1. Maintenance of vital respiration sings . 2. Decontamination to prevent further absorption by removal of the clothes , washing of the skin . 3. Atropine (antimuscarinic drug) parenterally in large doses (atropine dose is l-2mg I.V. every 15-60 min , until sings of effect appear: (dry mouth & heart rate in excess of' 70 beats/min). 4. Because atropine has antimuscarinic effect only, so not block N-M junction which has nicotinic receptors, therefore Mechanical ventilation may be needed to assist respiratory muscle. 5. Diazepam for convulsions if present. 6. Atropine eye drops may relieve headache caused by meiosis. 7. Reactivation of acetylcholinesterase: - Pralidoxime (PAM) this can reactivate the inhibited Achesterase, because it has a very high affinity for the phosphorus atom, that allows it to displace the organophosphate ( so it hydrolyze the phosphorylated Achesterase enzyme) and regenerates the this enzyme. -These substances hasten the destruction of accumulated Ach and unlike atropine, they have both antimuscarinic and antinicotinic effects. - The best result obtained if received within 12 hours of the poisoning, but muscle power may improve within 30 minutes. VI. Cholinergic Antagonists Classifications of Anticholinergic Drugs; Antimuscarinic Drugs: They are divided into: I- Tertiary amine: Alkaloid esters of tropic acid. 1- Atropine (hyoscyamine) is found in the plant (Atropa belladonna). prototype. 2- Hemoatropine: Semi synthetic. 3- Scopolamine. II- quaternary amine: Semi synthetic & synthetic. - They have been developed to produce more peripheral effects with decrease CNS effect. Include: Propantheline , Ipratropium , Clidinium bromide. 10 Pharmacokinetic of antimuscarinic drugs: - It is absorbed from GIT, mucus membrane , skin and eye . Belladonna alkaloid cross blood brain barrier (BBB) . - Scopolamine has greater effect on CNS & eye than atropine. - Atropine has greater effect on heart, intestine, bronchi and urinary tissue than scopolamine when absorbed. Mechanism of Action of Atropine: - Atropine has a high affinity for muscarinic receptors, where it binds competitively & reversiblely, preventing Ach from binding to that site. - It is stimulating or depressing depend on target organs and dose. Also depend on disease. - Atropine is both a central and peripheral muscarinic blocker. - Its general actions last about 4 hours except when placed topically in the eye, where the action may last for days. Actions of Atropine: 1- CNS: - Normal dose has minimal stimulant effect and slow sedation. Notes: - Atropine opposes the effects of all cholinergic drug on the CNS, at postganglionic cholinergic N-endings & on the peripheral blood vessels. - It does not oppose cholinergic effects at the N-m junction or significantly at the autonomic ganglia. a- Mydriasis (dilated pupil): By blocking the MR in papillary muscle. b- Cycloplegia: By weakening the contraction of ciliary M loss of ability to accommodate for near vision. c- Reduction of lachrymal secretion (dry or sandy eyes). d- Increase intraocular pressure (IOP) ? due to dilated iris blocking drainage of IO fluid from angle of anterior chamber (serious in elderly). 3- On CVS : - Atropine produces divergent effects on the CVS, depending on the dose. a- At low doses the predominant effect is a decreased cardiac rate (bradycardia) due to central vagal nerve activation. b- At higher doses, the cardiac receptors on the SA node are blocked, and the cardiac rate increases modestly (tachycardia). Note: Atropine has no significant effect on peripheral blood vessels in therapeutic dose but with poisoning, there is marked vasodilatation. 4- On Respiratory : bronchial dilatation , decrease secretion. 5- Gastrointestinal (GlT): a- Antispasmodic to reduce activity of the GlT. b- Block salivary gland leading to drying of oral mucosa (xerostomia). 6- On GUT: smooth muscle of ureter , bladder wall are relaxed and urination is slowed. 7- Exocrine glands secretions: All decrease (except Milk), causing dry mouth, dry eyes, dry skin (inhibit sweating), bronchial secretion decrease & become viscid. 11 Poisoning with Atropine: Features: - Dry mouth with dysphasia. - Mydriasis, blurred vision. - Hot flushes , dry skin with hyperthermia (CNS effect - absence of sweating). - Restlessness ,anxiety, excitement hallucinations, delirium, mania. - The cerebral excitation is followed by depression and coma. Treatment: - By giving activated charcoal to adsorb the drug, diazepam for excitement. Clinical uses of antimuscarinic agents: 1. On CNS: a- Benzhexol ,orpheradrine, against rigidity and tremor in parkinsonism. b- Hyoscine, promethazine, as antiemetic. c- Hyoscine prevent or reduce motion sickness. 2. Ophthalmologic disorders: - Antimuscarinic used in cases that need mydriasis with cycloplagia or prolonged action (Atropine, Homotropine, and Cyclopentolate) . -Tropicamide is the short acting mydriatic drug. 3. Respiratory disorder: a. Preoperative: To decrease bronchial secretion & spasm by preanesthetic injection of atropine or scopolamine (scopolamine cause amnesia for events associated with surgery). b- Ipratropium is useful in the treatment of asthma and COAD in patients unable to take adrenergic agonists. - New drug (Tiotropium) a long acting quaternary aerosol (by inhalation) antimuscarinic drug. 4. CVS disorders: a. Atropine used parenterally in Myocardial infarction (MI) because it block reflex vagal stimulation (bradycardia) accompany pain (of inferior MI) . b. Atropine used to treat sinus bradycardia and particularly useful when the arrhythmias result from anesthetic , cholinesters and succinyl choline. 5. GIT disturbances: a. Antispasmodic for treatment of spastic condition of the GIT because it lead to relaxation of smooth muscle, propantheline, - Hyosine butyl bromide (Buscopan) effective relaxant of the sm.m . b- Peptic ulcer : M1 inhibitor (Pirenzepine, Telenzepine). c- In preanesthesia they reduce salivation and gastric secretion. d- Hyoscine, promethazine, as antiemetic. 6. Urinary disorders: - Flavoxate, propantheline & oxybutynin, are used to relievesmooth muscle-spasm accompanying infection in cystitis and for detrusor instability. 12 7. Atropine used as antidotes to cholinergic and anticholinesterase agent, it is drug of choice to treat poisoning from organophosphate pesticides. - Its also used to block muscarinic effects due to cholinergic drugs such a Neostigmine are used. II- quaternary amine: Semi synthetic & synthetic drugs. - They have been developed to produce more peripheral effects with decrease CNS effect. 1- Clidinium bromide: It is derivative of belladonna alkaloid used in treatment of gastric disorders. - Sometimes combine with chlordiazepoxide (librax). 2- Propantheline (Duspataline): a. Used to relief from symptoms in patients with irritable bowel syndrome (IBS), pancreatitis, gastritis, diverticulitis, colitis . b. As antispasmodic for ureter and urinary bladder. 3- Ipratropium: It is useful in the treatment of asthma and COAD in patients unable to take adrenergic agonists. Adverse effect of antimuscarinic drugs: In the infants even ordinary dose could result in antimuscarinic fever, while in adults it depends on the dose : 1. Small dose: decrease salivation , decreased bronchial secretion, decrease sweating . 2. medium dose: pupil dilation visual accommodation decreased and heart rate is increased. 3. Largest dose: inhibition to the urination and intestinal motility and this is followed by decrease in gastric section and motility. 4. over dose: all above are exaggerated , with CNS excitation , restlessness , irritability and hallucination. Contraindication of antimuscarinic agents: 1. glaucoma. 2. In elderly men should be used in caution and should be avoided in those have history of prostatic hyperplasia . 3. Because atropine slow gastric empting , they increase symptoms in patient with peptic ulcer . 13 Nicotinic antagonists 1- Ganglion blocking agent: Trimethaphan 2- Neuromuscular Blocking Drugs: a- Non Depolarizing Competitive N-M blocking agents: Tubocurarine, Pancuronium, Atracurium, b- Depolarizing Non competitive N-M blocking agents Suxamethonium (Succinylcholine). 1- Ganglion blocking agent: - Hexamethionin, mecamylamine and other ganglion-blockers were extensively used in the treatment of hypertension. - But unfortunately, the adverse effect of ganglion blocked are so sever (both sympathetic and parasympathetic divisions are blocked), that patients are unable to tolerate long term treatment with them Trimethaphan: - It is the only Ganglion-blocker still in clinical use. Its poorly lipid soluble. Inactive orally and has a short half-life. - It is used I.V to treat sever accelerated hypertension (malignant hypertension). Note: As ganglion-blocking agents interrupts sympathetic control of venous-pooling, postural hypotension is the result. 2- Neuromuscular Blocking Drugs: - These drugs are important for producing complete sk-m relaxation in surgery, by specific blockade of the N-M junction. -They enable light level of anesthesia to be employed with adequate relaxation of the muscles of the abdomen and diaphragm. - They also relax the vocal cords and allow the passage of a tracheal tube. Note: Patients who have received a M-relaxant should always have their respiration assisted or controlled until the drug have been inactivated or antagonized. a. Non Depolarizing competitive N-M blocking agents Action: - Drugs of this group cause N-M block by competing with Ach at the receptor site at the N-M junction so prevent depolarization of muscle cell membrane and inhibit muscle contraction so causing complete SK- M relaxation. PK: Most non depolarizing agent have relatively long t1/2 ranging from 20 min to several hours. - These drugs are given parentally (by injection). 14 Tubocurarine - Is the prototype it produces a competitive block at the endplate causing flaccid paralysis lasts 30-60 min. - Tubocurarine blocks autonomic ganglia and causes an initial transient drop in blood pressure and cause histamine release which may induce bronchospasm. Note: The action of competitive N-M blocking agent is antagonized by anticholinesterases, Neostigmine is usually given I.V , preceded by atropine to prevent the parasympathetic autonomic effect of Neostigmine (bradycardia and salivation). b. Depolarizing Non competitive N-M blocking agents Suxamethonium (Succinylcholine) Mechanism of action: - It attaches to the nicotinic receptors and acts like Ach to depolarize the N-M junction. - Unlike acetylcholine, which is instantly destroyed by Achesterase, the depolarizing agent persists at high concentrations in the synaptic cleft, remaining attached to the receptor for a relatively long time, & providing a constant stimulation of the receptor. - Initially produces short-lasting muscle fasciculation, followed within a few minutes by paralysis. - The drug does not produce a ganglionic block, except in high doses, although it does have weak histamine-releasing action. - Normally, the duration of action of succinylcholine is extremely short (Total paralysis last up to 4 min) *It is particularly useful (used) for brief procedures such as tracheal intubations or electroconvulsive therapy (ECT). PK of Suxamethonium (succinylcholine): - Succinylcholine is injected intravenously. - Unlike the non depolarizing muscle relaxants its action cannot be reversed. - Its brief duration of action (several minutes) results from rapid hydrolysis by plasma pseudo cholinesterase. - It is hydrolyzed by plasma pseudo cholinesterase and its persistence in the body is increased by : 1- Neostigmine, which inactivate that enzyme. 2- In patient with hepatic disease or sever malnutrition, whose plasma concentration of enzyme may be lower than normal. 3- Procaine and amethocaine also are destroyed by this enzyme and so by competing with suxamethonium for the enzyme, may prolong its action. 15 4- There are persons with hereditary defects in amount or kind of enzyme, who cannot destroy the drug as rapidly as normal, so paralysis (Apnea) then lasts for hours. - Here treatment consist of ventilation until recovery, and may need fresh blood transfusion. Adverse effects of Succinylcholine: 1- Hyperthermia: When halothane is used as an anesthetic, administration of succinylcholine has occasionally caused malignant hyperthermia (with muscular rigidity and hyperpyrexia) in genetically susceptible people. - Treated by rapidly cooling the patient and by administration of dantrolene ?.. 2- Apnea: A genetically related deficiency of plasma cholinesterase or presence of an atypical form of the enzyme can lead to apnea due to paralysis of the diaphragm. 3- Cardiovascular: a- Repeated injections of suxamethonium can cause bradycardia and even cardiac arrest these probably due to activation of cholinoceptors in the heart and this can be prevented by atropine. b- It causes release of K from muscle which can be enough to cause cardiac arrest in patients with already hyperthermia. 4- Muscle pain lasting 1-3 days due to muscle fasciculation preceded the paralysis by Suxamethonium. - The pain can largely prevented by preceding succinylcholine with a small dose of a competitive N-M blocking agent (tubocurarine). 5- High dose can stimulate the uterus and can cause premature labor in pregnant. Contraindication of succinylcholine: 1- Hypersensitivity to suxamethonium, 2- Severe liver disease. 3- Burned patient. 4- Pregnancy. Uses of N-M blocking Drugs: - These drugs are important for producing complete skeletal muscle relaxation in surgery (main use). Other uses: 1- Control Ventilation: - In respiratory failure due to obstructive airway disease. 2- Treatment of convulsion: - By decrease peripheral manifestation of convulsion (As these drugs not cross BBB so has no effect on the central processes involved).