* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Prescott`s Microbiology, 9th Edition 9 Antimicrobial Chemotherapy
Discovery and development of non-nucleoside reverse-transcriptase inhibitors wikipedia , lookup
Discovery and development of proton pump inhibitors wikipedia , lookup
Compounding wikipedia , lookup
Polysubstance dependence wikipedia , lookup
Discovery and development of tubulin inhibitors wikipedia , lookup
Orphan drug wikipedia , lookup
Discovery and development of cephalosporins wikipedia , lookup
Discovery and development of integrase inhibitors wikipedia , lookup
Drug design wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Pharmacognosy wikipedia , lookup
Neuropharmacology wikipedia , lookup
Pharmacokinetics wikipedia , lookup
Pharmaceutical industry wikipedia , lookup
Psychopharmacology wikipedia , lookup
Drug discovery wikipedia , lookup
Prescription costs wikipedia , lookup
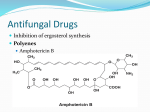
Prescott’s Microbiology, 9th Edition 9 Antimicrobial Chemotherapy CHAPTER OVERVIEW The control or the destruction of microorganisms that reside within the bodies of humans and other animals is of tremendous importance. This chapter introduces the principles of chemotherapy and discusses the ideal characteristics for successful chemotherapeutic agents (including the concept of selectively damaging the target microorganism while minimizing damage to the host). The chapter also presents characteristics of some commonly used antibacterial, antifungal, antiviral, and antiprotozoan drugs. LEARNING OUTCOMES After reading this chapter you should be able to: trace the general history of antimicrobial chemotherapy propose natural sources of new antimicrobial agents explain the difference between a narrow and broad spectrum drug correlate lack of microbial growth with selective toxicity list common side effects of antimicrobial drugs explain how to determine the level of antibacterial drug activity using the dilution susceptibility test, the disk diffusion test, and the Etest® predict antimicrobial drug levels in vivo from in vitro data compare antibacterial drug mechanisms of action relate side effect toxicity of antibacterial drugs to mechanism of action explain the relative effectiveness of various antibacterial agents based on drug target compare antifungal drug mechanisms of action explain why there are far fewer antifungal agents than there are antibacterial agents compare antiviral drug mechanisms of action provide a rationale for combination drug therapy, using an anti-HIV model explain why there are far fewer antiviral agents than there are antibacterial agents compare the mechanisms of action of antiprotozoan drugs relate side effects and toxicity of antiprotozoan drugs to their mechanism of action explain why there are far fewer antiprotozoan agents than there are antibacterial agents predict the effects (1) delivery route, (2) metabolism, and (3) local concentration on the effectiveness of an antimicrobial drug correlate the sensitivity of a microorganism to an antimicrobial agent with microbial growth in the presence of that agent identify practices that lead to antimicrobial drug resistance and suggest countermeasures CHAPTER OUTLINE I. The Development of Chemotherapy A. Paul Ehrlich (1904–1909)—aniline dyes and arsenic compounds B. Gerhard Domagk, and Jacques and Therese Trefouel (1939)—sulfanilamide C. Ernest Duchesne (1896) discovered penicillin, however, this discovery was not followed up D. Alexander Fleming (1928) accidentally discovered the antimicrobial activity of penicillin on a contaminated plate; however, follow-up studies did not show the drug would remain active in the body long enough to be effective 1 © 2014 by McGraw-Hill Education. This is proprietary material solely for authorized instructor use. Not authorized for sale or distribution in any manner. This document may not be copied, scanned, duplicated, forwarded, distributed, or posted on a website, in whole or part. Prescott’s Microbiology, 9th Edition E. Howard Florey and Ernst Chain (1939) aided by the biochemist, Norman Heatley, worked from Fleming’s published observations, obtained a culture from him, and demonstrated the effectiveness of penicillin F. Selman Waksman (1944)—streptomycin; this success led to a worldwide search for additional antibiotics, and the field has progressed rapidly since then II. General Characteristics of Antimicrobial Drugs A. Selective toxicity—ability to kill or inhibit microbial pathogen with minimal side effects in the host 1. Therapeutic dose—the drug level required for clinical treatment of a particular infection 2. Toxic dose—the drug level at which the agent becomes too toxic for the host (produces undesirable side effects) 3. Therapeutic index—the ratio of toxic dose to therapeutic dose: the larger the better B. Chemotherapeutic agents can occur naturally, be synthetic, or semisynthetic (chemical modifications of naturally occurring antibiotics) C. Drugs with narrow-spectrum activity are effective against a limited variety of pathogens; drugs with broad-spectrum activity are effective against a wide variety of pathogens D. Drug can be cidal (able to kill) or static (able to reversibly inhibit growth) E. Minimal inhibitory concentration (MIC) is the lowest concentration of the drug that prevents growth of a pathogen; minimal lethal concentration (MLC) is the lowest drug concentration that kills the pathogen III. Determining the Level of Antimicrobial Activity A. Dilution susceptibility tests—a set of broth-containing tubes are prepared; each tube in the set has a specific antibiotic concentration; to each is added a standard number of test organisms 1. The lowest concentration of the antibiotic resulting in no microbial growth is the MIC 2. Tubes showing no growth are subcultured into tubes of fresh medium lacking the antibiotic to determine the lowest concentration of the drug from which the organism does not recover; this is the MLC B. Disk diffusion tests 1. Disks impregnated with specific drugs are placed on agar plates inoculated with the test organism; clear zones (no growth) will be observed if the organism is sensitive to the drug; the size of the clear zone is used to determine the relative sensitivity; zone width also is a function of initial concentration, solubility, and diffusion rate of the antibiotic 2. Kirby-Bauer method is most commonly used disk diffusion test; test results are determined using tables that relate zone diameter to the degree of sensitivity C. The Etest® 1. Especially useful for testing anaerobic microorganisms 2. Makes use of special plastic strips that contain a concentration gradient of an antibiotic; each strip is labeled with a scale of MIC values; after incubation an elliptical zone of inhibition is observed and its intersection with the strip is used to determine the MIC IV. Antibacterial Drugs A. Inhibitors of cell wall synthesis are effective and selective because bacterial cell walls have unique structures not found in eukaryotic cells 1. Penicillins—inhibit cell wall synthesis; many types have been identified or synthesized including ampicillin, carbenicillin, and methicillin; they differ in spectrum of activity and administration route but all have a -lactam ring that is crucial for activity; resistance is an increasing problem, often due to penicillinase; some patients are allergic to these antibiotics 2. Cephalosporins—inhibit cell wall synthesis; broad spectrum of activity; they contain a -lactam ring, but are not subject to degradation by penicillinase; they can be given to some patients with penicillin allergies; they include cephalothin, cefoxitin, and ceftriazone 3. Vancomycin and teicoplanin—glycopeptide antibiotics that block peptidoglycan synthesis; vancomycin is particularly important as the last line of defense against antibiotic-resistant staphylococcal and enterococcal infections B. Protein synthesis inhibitors exploit the differences between prokaryotic and eukaryotic ribosomes 1. Aminoglycosides—contain cyclohexane ring and amino sugars; includes kanamycin, streptomycin, neomycin, and gentamicin; can be quite toxic to patients; act through interference with 30S ribosomal subunit, causing mistranslation with damaged proteins activating the envelope stress response and oxidative damage 2 © 2014 by McGraw-Hill Education. This is proprietary material solely for authorized instructor use. Not authorized for sale or distribution in any manner. This document may not be copied, scanned, duplicated, forwarded, distributed, or posted on a website, in whole or part. Prescott’s Microbiology, 9th Edition 2. Tetracyclines—contain a four-ring structure with side chains; very broad spectrum that includes intracellular parasites and mycoplasmas; bacteriostatic 3. Macrolides—12- to 22-carbon lactone rings linked to sugars; broad spectrum similar to that of penicillin; includes erythromycin and clindamycin; inhibit peptide chain elongation by binding rRNA 4. Chloramphenicol—has a broad spectrum but is quite toxic; inhibits peptidyl transfer reaction C. Metabolic antagonists are structural analogs of metabolic intermediates that act as antimetabolites, inhibiting metabolic pathways; bacteriostatic 1. Sulfonamides or sulfa drugs—inhibit folic acid synthesis in bacteria (humans don’t synthesize folic acid, so are not affected); resistance is increasing and many patients are allergic to these drugs; includes p-aminobenzoic acid (PABA) 2. Trimethoprim—synthetic antibiotic that blocks folic acid production; broad spectrum often combined with sulfa drugs D. Nucleic acid synthesis inhibitors block enzymes of transcription and translation; generally not as selectively toxic 1. Quinolones—synthetic drugs that inhibit bacterial DNA gyrase or topoisomerase II, thereby disrupting replication, repair, and other processes involving DNA; broad spectrum; includes nalidixic acid and ciprofloxacin (Cipro) V. Antifungal Drugs A. Fungal infections are more difficult to treat than bacterial infections because the greater similarity of fungi and host limits the ability of a drug to have a selective point of attack; furthermore, many fungi have detoxification systems that inactivate drugs B. Superficial mycoses are infections of superficial tissues and can often be treated by topical application of antifungal drugs such as miconazole, nystatin, and griseofulvin, thereby minimizing systemic side effects C. Systemic mycoses are more difficult to treat and can be fatal; amphotericin B and flucytosine have been used with limited success; amphotericin B is highly toxic and must be used with care; flucytosine must be converted by the fungus to an active form, and animal cells are incapable of this; some selectivity is possible, but severe side effects have been observed with both drugs; posaconazole is effective against drug-resistant fungi and are less toxic D. Subcutaneous mycoses (e.g., mycetomas) are treated with a mixture of therapies VI. Antiviral Drugs A. Selectivity is a problem because viruses use the metabolic machinery of the host B. Antiviral drugs target specific steps of life cycle, including viral uncoating and DNA replication (e.g., amantadine, vidarabine, acyclovir, cidofovir, and azidothymidine) C. Anti-HIV drugs (e.g., AZT, ddI, 3TC) have four targets: nucleoside reverse transcriptase inhibitors (NRTIs), nonnucleoside reverse transcriptase inhibitors (NNRTIs), protease inhibitors (block viral polypeptide processing), and fusion inhibitors (block viral entry into cell); combinations of drugs often used D. Tamiflu is a neuraminidase inhibitor that is used to treat influenza VII. Antiprotozoan drugs A. Mechanisms of action for antiprotozoan drugs are largely unknown; as protozoans and humans are both eukaryotes, selective toxicity is difficult to achieve B. Chloroquine and mefloquine—used to treat malaria; variety of mechanisms proposed C. Artemisinin—anti-malarial drug used in traditional Chinese medicine D. Metronidazole—used to treat Entamoeba infections; appears to interact with DNA E. Atovaquone—an analog of ubiquinone that interferes with electron transport chain VIII. Factors Influencing the Antimicrobial Drug Effectiveness A. Drug effectiveness—this is greatly influenced by the mode of administration (e.g., oral, topical, parenteral), but also can be influenced by exclusion from the site of infections (e.g., blood clots or necrotic tissue protects bacterium) B. Susceptibility of pathogen—influenced by growth rate and by inherent properties (e.g., whether or not pathogen has target of the drug) 3 © 2014 by McGraw-Hill Education. This is proprietary material solely for authorized instructor use. Not authorized for sale or distribution in any manner. This document may not be copied, scanned, duplicated, forwarded, distributed, or posted on a website, in whole or part. Prescott’s Microbiology, 9th Edition C. D. Factors influencing drug concentration in the body—must exceed the pathogen’s MIC for the drug to be effective; this will depend on the amount of drug administered, the route of administration, the speed of uptake, and the rate of clearance (elimination) from the body Overcoming drug resistance 1. Several strategies can be used to discourage emergence of drug resistance (e.g., administration of high doses, simultaneous treatment with more than one drug, limited use of broad-spectrum antibiotics) 2. Drug resistance has become an increasing problem; new drugs are constantly being developed and new treatment methods (e.g., phage treatment of bacterial infections) are being explored CRITICAL THINKING 1. Antibiotics are natural products of certain microorganisms. What advantages might these antibiotics provide for the organisms that produce them? 2. Viruses generally use the metabolic machinery of their hosts. Therefore, they should present no selective point of attack for potential antiviral drugs. Yet, recently there have been several antiviral drugs developed that have a reasonably high therapeutic index. Explain. 3. Chemotherapeutic agents that are variations of natural biotic products dominate the lists of antimicrobials. Many of these agents specifically target one particular biochemical process. In this way, they provide a strong selective pressure directed at a narrow target. Comment on how this may lead to natural selection of organisms that achieve mutations in particular pathways that facilitate resistance to chemotherapeutic substances. CONCEPT MAPPING CHALLENGE Construct a concept map based on table 9.1 that highlights some of the common antibiotics taking into account their mechanism of action. Be sure to include: cell wall disruption, membrane permeability, protein synthesis inhibitors, DNA replication disruptors, and metabolic disruptors. 4 © 2014 by McGraw-Hill Education. This is proprietary material solely for authorized instructor use. Not authorized for sale or distribution in any manner. This document may not be copied, scanned, duplicated, forwarded, distributed, or posted on a website, in whole or part.