* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
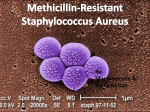
Download Methicillin-Resistant Staphylococcus Aureus
Eradication of infectious diseases wikipedia , lookup
Brucellosis wikipedia , lookup
Traveler's diarrhea wikipedia , lookup
Neglected tropical diseases wikipedia , lookup
Sarcocystis wikipedia , lookup
Tuberculosis wikipedia , lookup
Gastroenteritis wikipedia , lookup
Hepatitis C wikipedia , lookup
Antibiotics wikipedia , lookup
Middle East respiratory syndrome wikipedia , lookup
Human cytomegalovirus wikipedia , lookup
Dirofilaria immitis wikipedia , lookup
African trypanosomiasis wikipedia , lookup
Trichinosis wikipedia , lookup
Marburg virus disease wikipedia , lookup
Hepatitis B wikipedia , lookup
Clostridium difficile infection wikipedia , lookup
Bottromycin wikipedia , lookup
Sexually transmitted infection wikipedia , lookup
Anaerobic infection wikipedia , lookup
Carbapenem-resistant enterobacteriaceae wikipedia , lookup
Onchocerciasis wikipedia , lookup
Leptospirosis wikipedia , lookup
Schistosomiasis wikipedia , lookup
Oesophagostomum wikipedia , lookup
Coccidioidomycosis wikipedia , lookup
Neonatal infection wikipedia , lookup
Staphylococcus aureus wikipedia , lookup
Methicillin-resistant Staphylococcus aureus wikipedia , lookup
Running head: MRSA 1 Methicillin-Resistant Staphylococcus Aureus Chris Common Ferris State University Disaster Nursing and Emergency Preparedness NURS 319 Marietta Bell-Scriber April 09, 2010 MRSA 2 Abstract Incidents of infectious disease outbreaks have been common topic in the news nationwide. Finding treatment for these diseases has proven to be a difficult task for medical personnel. For some individuals whose bodies have become increasingly resistant to traditional treatment regimens, the solution becomes even more difficult. Methicillin-resistant Staphylococcus aureus (MRSA) is one form of infectious disease that has become increasingly prevalent in recent years. A descriptive summary in the areas of transmission/isolation, clinical presentation, diagnosis, and therapy will be discussed. An identification of factors and/or situations that may promote this emerging disease will be supported with resources throughout this evidenced based paper. MRSA 3 Methicillin-Resistant Staphylococcus Aureus Methicillin-resistant Staphylococcus aureus (MRSA) are a type of staphylococcus or “staph” bacteria that are resistant to many antibiotics. Staph bacteria normally live on your own skin and in your nose, usually without causing problems. Approximately 25% to 30% of the population is colonized in the nose with Staph bacteria. It can also be carried in the armpit, groin, or genital area. Staph bacteria are one of the most common causes of skin infections in the United States (CDPH, 2009). By definition, staphylococcus is a genus of gram-positive cocci, sometimes part of the normal flora of the skin, mucous membranes, respiratory, or gastrointestinal tracts. Staphylococcus is also common in the general environment (UMHS, 2007). The problem exists when these bacteria mutate into strains that become resistant to traditional medicines such as penicillin or its synthetic form, methicillin. As more antibioticresistant bacteria or “super bugs” as they are sometimes referred to as, develop, hospitals are taking extra care to practice infection control to decrease the likelihood of spreading the bacteria to others. In the late 1970s, hospitals in eastern Australia saw the first outbreaks of methicillinresistant Staphylococcus aureus (MRSA). By the 1980s, MRSA had emerged in various places throughout the world (PRHI, 2003). It is very difficult to accurately date the exact time frame as to when this resistant form of staphylococcus was formed. These same bacteria that once were harmless while being present on the human body are thought to have mutated due to over usage or misusage or antibiotics. The Centers for Disease Control have identified other key problems related to the spread of this “super bug”. Inappropriate treatment of colonization instead of treating only active infection increases resistance. Inadequate infection prevention and control allows for spread from infected or colonized patient and the under use of vaccines (such as MRSA 4 influenza) allows fro more secondary bacterial infections in persons with vaccine preventable disease and increased use of antibiotics to treat as mentioned earlier. Physicians and scientists now realize the seriousness of this emerging infectious disease and must take special precautions to prevent further spread. When the bacteria grows on the skin and mucous membranes without causing infection it is known as colonization, and people who are colonized with MRSA are known as carriers of MRSA (UMHS, 2007). MRSA can cause infections such as boils, wound infection, infected and decubitus ulcers. MRSA is a strain of Staphylococcus aureus that is distinguished from other Staphylococcus aureus strains by its resistance to beta-lactam antibiotics. MRSA are identified in laboratories through the use of the mecA gene test (UMHS, 2007). Although the mecA gene test is the most accurate method for the detection of methicillin-resistant Staphylococcus aureus (MRSA), it is not widely used at hospitals and many clinicians lack knowledge regarding the appropriate and timely application of mecA gene test results for the selection of optimal antimicrobial therapy (OAT) against S. aureus infections (ASM, 2008). The majority of MRSA infections occur among patients in hospitals or other healthcare settings. However, it is becoming more common in the community setting (CDC, 2008). Community settings refer to those persons who acquire Staph and MRSA outside of hospitals and other healthcare facilities. The major concern facing healthcare workers who come in contact with infected individuals is the potential of spreading the infection to other patients. There are some individuals that are more prone for infection. Children and elderly who have weakened immune systems are said to be at greater risk of contracting the infection or colonizing MRSA (UMHS, 2007). That is not to say that only immunocompromised patients are at risk. MRSA is becoming more common in healthy people. These infections can occur among people who are likely to have cuts or wounds and who have MRSA 5 close contact with one another, such as members of sports teams (UMHS, 2007). Spread may also occur through indirect contact by touching objects (e.g., towels, sheets, wound dressings, clothes, workout areas, or sports equipment) contaminated with Staph bacteria or MRSA (Charmeck, 2010). When an individual tests positive for MRSA special contact precautions must be followed along with general infection control measures. These measures consist of frequent hand washing by physicians, nurses and other health care workers, as the most common way hospitalacquired MRSA is transmitted to patients in through human hands. The wearing of gowns, eye protection, and gloves and masks when appropriate also aid in reducing transmission. MRSA is not usually spread through the air like the common cold or flu virus, unless a person has MRSA pneumonia and is coughing (UMHS, 2007). Frequent cleaning of medical devices, instruments, and bedding is essential anytime they have come into contact with the infected individuals. At some facilities it is policy that a contact precautions sign be placed outside the patient’s room. This precaution is designed to alert visitors and other healthcare workers of the patient’s condition and also acts as a reminder of which barrier equipment will be needed prior to entering the room. According to the Centers for Disease Control it is not recommended that all health care workers be screened to see if they are colonized with MRSA and it is not recommended to treat all workers that do test positive for MRSA. Culturing can detect carriers, but not who will come down with infection or who might spread the bacteria. Treatment is often unsuccessful and can create further resistance, and most carriers of MRSA will not become ill (CDC, 2008). Most Staphylococcus skin infections are minor and may be easily treated. In mild cases of skin infection the treatment will include taking an antibiotic or having the doctor drain the infection. One might also be given an ointment to put on the infected skin or inside the nose MRSA 6 along with washing one’s skin with antibiotic soap called chlorhexidine (Hibiclens) to reduce MRSA bacteria on the skin (AAP, 2005). Staphylococcus also may cause more serious infections, such as infections of the bloodstream, surgical sites, or pneumonia. Sometimes, a Staphylococcus infection that starts as a skin infection may worsen (CDC, 2008). Symptoms of a MRSA infection depend on where the infection is. Staphylococcal disease has distinctly different clinical and epidemiological patterns in the general community, in newborns, in menstruating women (Toxic Shock Syndrome), in institutionalized patients, and in heath care workers (AAP, 2005). If MRSA is causing an infection in a wound, that area of the skin may be red or tender. If one develops MRSA pneumonia, a cough may develop. Community-based MRSA commonly causes skin infections, such as boils, abscesses, or cellulitis (UMHS, 2007). Neglecting to seek medical attention upon developing symptoms could be dangerous as MRSA infections can become serious in a short amount of time. The incubation period is commonly 4-10 days following exposure, however disease may not occur until several months after colonization (AAP, 2005). Symptoms often mimic those of an insect or spider bite. Many times these lesions are localized and discrete. However, in some cases the infection can enter the bloodstream and may lead to much more serious conditions such as pneumonia, osteomyelitis, septicemia, endocarditis, meningitis, or other serious diseases (UMHS, 2007). In any case where an antibiotic is prescribed it is essential that the individual continues to take the antibiotic in its entirety even if the infection appears to be getting better. The only time one should stop taking the medication is if it is recommended by their physician or they develop a reaction to the medication, in which case they should notify their physician immediately. Methicillin-resistant Staphylococcus aureus has proven to be a dangerous infectious disease that affects individuals of all ages and social background. The Staphylococcal bacteria MRSA 7 themselves are not dangerous and can be found on the skin and mucous membranes of most human beings. The potential for becoming infected with the resistant strain of the bacteria depends largely on the environment that the individual is exposed to and how often the individual was given antibiotics for viral infections. However, that is not to say that every patient that receives a dose of antibiotics when antibiotics were not indicated will automatically develop the resistant strain. For those that do become infected with MRSA, symptoms may not become evident until several months after colonization. In mild cases of skin infection the treatment will include taking an antibiotic or having the doctor drain the infection. One might also be given an ointment to put on the infected skin or inside the nose along with washing one’s skin with antibiotic soap. For those individuals with more severe cases that require hospitalization will be placed in a private room to reduce the chances of spreading the bacteria to other patients. The healthcare workers caring for the patient will follow strict contact precautions by donning a gown, gloves, and face mask when MRSA pneumonia is suspected. Visitors or patients along with health care providers are asked to at the very least wash their hands with soap and warm water prior to exiting the patient’s room. As for the patient receiving treatment the single most important factor is to take all of their prescribed antibiotics until all doses have been completed to eliminate the possibility of their body building resistance to the antibiotic being used to fight the infection. According to the CDC the good news is major strides have been made in recent years to reduce the numbers of MRSA infections in healthcare settings. MRSA 8 References American Society for Microbiology. (2008). Impact of mecA Gene Testing and Intervention by Infectious Disease Clinical Pharmacists on Time to Optimal Antimicrobial therapy for staphylococcus aureus bacteremia at a university hospital. Retrieved from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2446910/ Centers for Disease Control and Prevention. (2008). Community-associated MRSA information for the public. Retrieved from http://www.cdc.gov/ncidod/dhqp/ar_mrsa_ca_public.html#5 CharMeck.org. (2010). Let’s talk about ...community-associated methicillin resistant staphylococcus aureus. Retrieved from http://www.charmeck.org/Departments/Health+Department/Top+News/MRSA.htm Pittsburgh Regional Healthcare Initiative. (2003). MRSA: a short history of a monster microbe. Retrieved from http://www.prhi.org/docs/MRSAa%20short%20history%20of%20a%20monster%20micr obe12-1-2003.pdf Report of the Committee on Infectious Diseases (26 ed.). (2005). Elk Grove Village, IL: American Academy of Pediatrics. State of California- Health and Human Services Agency. (2009). Community-associated (CAMRSA)/staph infections: a guideline for athletic departments. Retrieved from http://www.cdph.ca.gov/healthinfo/discond/documents/camrsainfectionsguidelineathletic sdepartment.pdf University of Michigan Health System. (2007). MRSA: a guide for health care staff. Retrieved from http://www.med.umich.edu/i/policies/ice/ICM_ip/pdf/cpexhibitc.pdf MRSA 9 University of Michigan Health System. (2007). Protecting our patients against MRSA. Retrieved from http://www.med.umich.edu/opm/newspage/2007/mrsa.htm