* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Anti Hyperlipidaemic Agents
Discovery and development of neuraminidase inhibitors wikipedia , lookup
Discovery and development of angiotensin receptor blockers wikipedia , lookup
Pharmaceutical industry wikipedia , lookup
Drug design wikipedia , lookup
Prescription costs wikipedia , lookup
Drug discovery wikipedia , lookup
Neuropharmacology wikipedia , lookup
Discovery and development of ACE inhibitors wikipedia , lookup
Discovery and development of proton pump inhibitors wikipedia , lookup
Plateau principle wikipedia , lookup
Discovery and development of cyclooxygenase 2 inhibitors wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
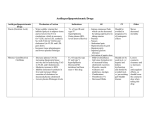
Anti Hyperlipidaemic Agents Basis of Anti Hyperlipidaemic Agents Usage Decision in choosing Anti Hyperlipidaemic agents 1. Specific metabolic defect that causes hyperlipidaemia 2. The potential of the particular metabolic defect to cause a. Artherosclerosis b. Pancreatitis 3. Treatment in children a. In heterozygous familial hypercholestrolaemia i. Only be given Antihyperlipidaemic agents after 7-8 years old 1. Complete myelination of nervous system happens at this particular age ii. Can be treated with 1. Statin 2. Niacin 3. Resin 4. Ezetimibe b. Decision should solely depends on i. Level of LDL ii. Family history iii. Child’s age iv. Other risk factors c. Antihyperlipidaemic agents rarely be given in patient below the age of 16 4. Antihyperlipidaemic agents should never be given to a. Pregnant ladies b. Woman who intends to get pregnant c. Lactating mother 5. Dose should be adjusted in patient receiving a. Warfarin b. Indandione anticoagulant Disorder Manifestations Familial Hyperchylomicronaemia Famillial Hypertriglyceridaemia Moderate Severe Familial Combined Hyperlipidaemia Broad Beta Band Disease ↑chylomicron ↑VLDL ↑chylomicron (maybe increased) ↑VLDL ↑chylomicron ↑VLDL ↑↑VLDL ↑↑LDL Both ↑ ↑IDL ↑Chylomicron remnant ↑LDL ↑↑LDL ↑LDL Heterozygous Familial Hypercholesterolaemia Homozygous Familial Ligand-defective apo B Lp(a) Hyperlipoproteinaemia Lp(a)↑ *Single Therapy – only one drug is used out of the list Single Therapy* Combined Therapy 1. Niacin 2. Fibrate 1. Niacin (and) 2. Fibrate 1. 2. 3. 1. 2. 3. 1. 2. 1. 2. 1. Two or three of the single therapy drugs Niacin Fibrate Statins Niacin Statins Ezetimibe Niacin Statins Niacin Fibrate 3. Statins 4. Resin 5. Niacin 6. Ezetimibe 7. Niacin 8. Atorvastatin 9. Rosuvastatin 10. Ezetimibe 11. Niacin 12. Statins 13. Ezetimibe 14. Niacin 1. 2. 1. 2. 3. 4. Niacin + Statins (or) Fibrate + Statins Niacin + Fibrate (or) Niacin + Statins (or) Fibrate + Statins Two or three of the single therapy drugs 5. Niacin +Statins + Ezetimibe 6. Niacin + Statins (or) 7. Niacin + Ezetimibe 8. NA HMG-CoA Reductase Inhibitor (Statins) Drug Simvastatin Drug drug interactions 1. Plasma level ↑ if given with CYP450 inhibitors a. Macrolides b. Cyclosporine c. Ketoconazole d. Protease Inhibitor in HAART e. Tacrolimus f. Fibrates g. Nefazodone 2. Plasma level ↓ if given with CYP450 inducers a. Phenytoin b. Griseofulvin c. Barbiturates d. Rifampicin Pharmacokinetic Absorption Given in inactive form (lactone prodrug) o Metabolized in the gut wall into active B-hydroxyl derivatives Readily absorp (lipophilic in nature) through intestinal mucosa Improve absorption when taken with food o Knowledge that it is absorp together with lipid and fatty acids of the food Distribution Plasma half life is 12-24 hours Metabolism Extensively undergoes 1st metabolism Excretion Bile o 80% Urine o 20% 1. 2. 3. 4. Mechanism of Action HMG-CoA Reductase is an enzyme required for a commited step in coverting HMG-CoA Mevalonate Simvastatin is an analogue of HMG-CoA and therefore acts as competitve partial inhibitor of HMG-CoA Reductase enzyme Consequences to the inhibition of the HMG-CoA Reductase commited step are a. ↓in the synthesis of endogenous cholesterol in the liver b. As a part of compensatory mechanism secondary to ↓heaptic cholesterol level, liver will ↑the expression of LDL receptors on its surface so that i. ↑internalization of plasma 1. IDL 2. LDL ii. ↓level of LDL in the circulation c. ↓in the level of the hepatic cholesterol level will lead to secondary ↓of TG as VLDL (endogenous TG carrier) needs cholesterol during its synthesis Other therapeutical effects of statin are a. ↓vascular inflammation b. Stabilizes artheromatous plaque i. ↓new coronary event ii. ↓formation of thromboembolism c. ↓oxidative stress levels Adverse Effects 1. Myositis/Rhabdomyolisis a. ↑CK level and myoglobin in the blood i. ↑renal shut down b. Need to be carefully monitored and might be discontinued if CK level persistently ↑ 2. Hepatotoxicity a. ↑plasma aminotransferase level (3 times higher than that of normal range) b. Discontinued immediately if plasma aminotransferase ↑persistently Should be temporarily discontinued in case of 1. Serious illness 2. Trauma 3. Major surgery Niacin (Vitamin B3) Drug Nicotinic Acid Pharmacokinetic Absorption Readily absorb through gut mucosa Hydrophilic in nature therefore absorbed together with water Distribution Tends to accumulate in blood Also tends to accumulate in water-filled compartment of the body Metabolism Extensively metabolized into amide Incorporated into Niacinamide Adenine Dinucleotide (NAD) Excretion Excreted readily through urine as o Unmodified form o Several metabolites 1. 2. 3. 4. Mechanism of Action Magnifies the activity of Lipoprotein Lipase of adipose tissues a. ↑clearance of triglycerides from i. Chylomicron ii. VLDL b. ↑excretion of sterol acutely as cholesterol is mobilized from tissue i. New steady state reached Inhibits the activity of Hormone Sensitive Lipase of adipose tissue via receptor mediated signalling a. ↓hydrolization of peripheral tissues (adipose) of TG b. ↓influx of fatty acids into the liver i. Consequently ↓VLDL synthesis and plasma level No effect on bile acid formation Therefore, Nicotinic Acid a. ↓VLDL b. ↓chylomicron c. ↓TG d. ↓LDL e. ↓TC f. ↑HDL 1. 2. 3. 4. 5. 6. Adverse Effects Hyperglyceamia a. ↑activity of LPL, which needs insulin as an activator b. ↑prolong usage of insulin ↑insulin tolerence c. Therefore partially contraindicate d in insulin dependent diabetis mellitus pts Gastritis Pruritus Rashes Abdominal discomfort Hepatotoxicity Fibrates Drug Pharmacokinetic Absorption Gemfibrozil 1. Should be avoided Quantitatively absorbed through intestinal mucosa in patient with ↑absorption when taken with a. Hepatic failure food b. Renal failure Distribution Drug Drug Interaction Undergoes Enterohepatic Recycling 1. Potentiate o ↑half life (1.5 hours) Warfarin effect a. Displace warfarin Readily passes placental barrier from plasma Tightly bound to plasma protein protein Metabolism Hepatic modification into o Hydroxylmethyl o Carboxyl o Quinol derivatives Excretion Renal clearance in unmodified form Mechanism of Action 1. Fibrate is a ligand of nuclear transcription factor; PPAR-a a. Activation of this transcription factor will lead i. ↑ up-regulate 1. LPL 2. Apo-A1 3. Apo-AII ii. ↓trancription of apo-CIII 1. ↓inhibition of lipolysis 2. Major effect a. ↑oxidation of fatty acids in i. Liver ii. Striated muscles b. ↑lypoprotein lipase activity i. ↓VLDL ii. ↓TG c. ↓activity of Hormone Sensitive Lipase i. ↓liberation of TG from adipose tissues into the circulation d. Moderately ↑HDL level Adverse Effects 1. Rhabdomyolisis a. ↑when it is given with statins b. EXCEPT rosuvastatin 2. Cholestasis (gallstones) a. ↑in liver uptake of plasma cholesterol b. ↑clearance of cholesterol via bile acids c. Should be used in caution for patient with i. Billiary tract disease ii. High risk; women 3. Hepatotoxicity a. ↑aminotransferase b. ↑alkaline phosphatase Bile Acid Sequestrants (Resins) Drug Cholestyramine 1. Should be given with Niacin in patient having combined hyperlipidaemia 1. 2. 3. 4. Pharmacokinetic Large polymeric cationic exchange resins Insoluble in water Bind with bile acid in the intestinal lumen Not being absorbed Mechanism of Action 1. Binds to bile acid in the gut, reduces bile acid reabsorption as high as ten folds. 2. ↑excretion of bile acid a. ↑cholesterol secretion b. ↓hepatic cholesterol level c. ↑uptake of LDL from circulation i. ↓plasma LDL ii. ↓plasma cholesterol level d. Compensatory mechanism of the loss of LDL will ↑VLDL and therefore ↑plasma TG level 3. It most be clear that Resins is not effective in patient having homozygous Familial Hypercholeterolaemia due to the absence of LDL receptor in the liver, but useful in heterozygous 1. 2. 3. 4. 5. 6. 7. 8. 9. Adverse Effects Hypertriglyceridaemia Constipation Bloating Flatulence Heartburn Diarrhea Steatorrhea Malabsorption of Vitamin K a. Hypoprothrombinaemia Gallstones formation Intestinal Sterol Absorption Inhibitor Drug Ezetimibe 1. No interaction with warfarin Pharmacokinetic Absorption Readily absorp in the intestinal mucosa Distribution Undergoes Enterohepatic Recycling Half life is 22 hours Peak level within 12-24 hours Metabolism Conjugated with glucuronide into active form Excretion Bile acids (therefore reduce reabsorption when given with resins) Mechanism of Action 1. Selective inhibitor of transport protein NPCL1L1, important in the absorption of a. Cholesterol b. Phytosterols 2. Effective even when there is an absence of dietary cholesterol, as it also inhibits reabsorption of cholesterol in the bile acids Adverse Effects 1. Myositis (rare) 2. Hepatotoxicity (rare) a. When given with statin