* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Hyperlipidemias
Discovery and development of direct thrombin inhibitors wikipedia , lookup
Environmental impact of pharmaceuticals and personal care products wikipedia , lookup
Pharmaceutical industry wikipedia , lookup
Toxicodynamics wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
Pharmacokinetics wikipedia , lookup
Psychopharmacology wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Prescription costs wikipedia , lookup
Wilson's disease wikipedia , lookup
Discovery and development of cyclooxygenase 2 inhibitors wikipedia , lookup
Plateau principle wikipedia , lookup
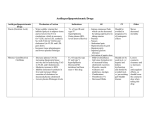
Hyperlipidemias Cholesterol is absorbed from the intestine and transported to the liver by chylomicron remnants. Hepatic cholesterol enters the circulation as very low density lipoprotein VLDL which is metabolized by lipoprotein lipase enzyme to intermediate lipoprotein LDL and low density lipoprotein LDL which are then removed by liver liver or peripheral tissues. In the peripheral tissues cholesterol is converted to steroid hormones or used to form cell walls and membranes. The quantity of cholesterol transported from the liver to peripheral tissues greatly exceeds its catabolism, so the excess amount of cholesterol is returned back to the liver by high density lipoprotein HDL. Atherosclerosis and coronary heart disease are associated with elevated levels of low density lipoprotein (LDL cholesterol) and triacyglycerol with low levels of HDL cholesterol. Other risk factors include smoking, hypertension, obesity, diabetes, lack of exercise and consumption of a diet containing saturated fat. Hyperlipidemia can also result from a single inherited gen defect in 1 lipoprotein metaboli 2 Treatment strategies A. Diet: by reducing the total intake of cholesterol and saturated B. Drugs aft. Alcohol raises triglyceride TG and VLDL so should be avoided. 3 1- HMG CoA reductase inhibitors: Statins. Mechanism of action Inhibition of HMG CoA reductase: they inhibit 3-hydroxy-3methyl glutaryl (HMG)coenzyme A(CoA) which is the rate limiting step in cholesterol synthesis, so depleting the intracellular supply of cholesterol. Ac-CoA HMG-CoA cholesterol bile acid inhibited by resin gut Increase in LDL receptors: as a compensatory mechanism for the depletion of intracellular cholesterol synthesis, liver increases the number of LDL receptors as a method to recapture cholesterol. Thus the end result is a reduction in plasma cholesterol both by lowered synthesis and increase catabolism of LDL. Clinical uses: lowering plasma cholesterol in all types of hyperlipidemia and reduce the risk of coronary events and ischemic heart disease. 4 Pharmacokinetics: well absorbed after oral administration undergo first pass metabolism, excreted through bile and feces and some urinary elimination also occurs. Adverse effects: Biochemical abnormalities in liver function have occurred, therefore it important to evaluate liver function and measure serum transaminase levels periodically. Myopathy and rhabdomyolysis (disintegration or dissolution of muscle) rarely reported. Drug interactions: these drugs increase warfarin levels; on the other hand enzyme inhibitors increase the risk of hepatotoxicity because they increase statins level. Statins are contraindicated during pregnancy, nursing mothers and in children. Some adverse effects and precautions 5 2- resin or called bile binding resins They are anion-exchange resins that bind negatively charged bile acids and bile salts in the small intestine. The resin/bile acid complex is excreted in the feces, thus preventing the bile acids from returning to the liver by the enterohepatic circulation. This causes hepatocytes to increase conversion of cholesterol to bile acids, resulting in decreasing the intracellular cholesterol concentration which activates an increased hepatic uptake of cholesterolcontaining LDL particles ( by increasing surface LDL receptors), leading to a fall in plasma LDL. Clinical uses: treatment of hypercholesterolemia and relieve pruritus caused by accumulation of bile acids in patients with biliary obstruction. Pharmacokinetics: they are taken orally. Because they are insoluble in water and are very large , they are neither absorbed nor metabolically altered by the intestine. Instead, they are totally excreted in the feces. Adverse effects: 1- constipation, nausea, and flatulence. 2- impair the absorption of the fat-soluble vitamins (A, D, E, and K). 3- interfere with the intestinal absorption of many drugs for example, tetracycline, phenobarbital, digoxin, warfarin, pravastatin, fluvastatin, aspirin, and thiazide diuretics. Therefore, drugs should be taken at least 1 to 2 hours before, or 4 to 6 hours after, the bile acid binding resins. 6 7 3- Cholesterol absorption inhibitors Ezetimibe selectively inhibits intestinal absorption of dietary and biliary cholesterol in the small intestine, leading to a decrease in the delivery of intestinal cholesterol to the liver. This causes a reduction of hepatic cholesterol stores with a compensatory increase in the synthesis of high affinity LDL receptors lead to increase the removal of LDL from the blood. Ezetimibe metabolized in the small intestine and liver with subsequent biliary and renal excretion. It is used to treat hypercholesterolemia but should be avoided in patients with moderate to sever hepatic insufficiency. 4- Niacin (nicotinic acid) Mechanism of action: niacin strongly inhibits lipolysis in adipose tissuethe primary producer of circulating free fatty acids. The liver normally utilizes these circulating fatty acids in triacylglycerol synthesis. Thus, niacin causes a decrease in liver triacylglycerol synthesis, which is required for VLDL production. LDL (the cholesterol-rich lipoprotein) is derived from VLDL in the plasma. Therefore, a reduction in the VLDL concentration also results in a decreased plasma LDL concentration. Thus, both plasma triacylglycerol (in VLDL) and cholesterol (in VLDL and LDL) are lowered. Niacin treatment increases HDL cholesterol levels. Therapeutic uses: treatment of severe hypercholesterolemias. Pharmacokinetics: Niacin is administered orally. It is converted in the body to nicotinamide, and excreted in the urine. Adverse effects: flushing, feeling of warmth and pruritus. Administration of aspirin prior to taking niacin decreases flushing. Other side effects include nausea, abdominal pain and hyperuricemia. 8 4- The fibrates: Fenofibrate and gemfibrozil Mechanism of action: they interact with peroxisome proliferator activated receptor-alpha (PPAR-ά) protein, a receptor that regulates transcription of genes involved in lipid metabolism. This interaction results in increased activity of lipoprotein lipase and enhanced clearance of VLDL (triglyceride rich lipoprotein) they decrease cholesterol synthesis and increase HDL level. Therapeutic uses: The fibrates are used in the treatment of hypertriacylglycerolemias, and incombination with other cholesterol lowering agents for treatment of patients with elevated concentration of both LDL and VLDL. Pharmacokinetics: well absorbed orally, widely distributed, undergo extensive biotransformation and excreted in urine. Adverse effects: Nausea, Lithiasis: Because these drugs increase biliary cholesterol excretion, lead to the formation of gallstones. Others is Myositis (inflammation of a voluntary muscle) 9 They should not be used in patients with severe hepatic and renal dysfunction or in patients with preexisting gallbladder disease. Drug interactions: Both fibrates compete with the coumarin anticoagulants for binding sites on plasma proteins, thus transiently potentiating anticoagulant activity. these drugs may transiently elevate the levels of sulfonylureas. 10 Combination drug therapy It is often necessary to employ two antihyperlipidemic drugs to achieve treatment goals in plasma lipid levels. The most commonly combined agents: Niacin + bile acid-binding agent. HMG-CoA reductase inhibitor + bile acid- binding agent. Low dose statin + ezetimibe. 11