* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download click here for presentation
Coronary artery disease wikipedia , lookup
Heart failure wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Myocardial infarction wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Cardiac surgery wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
Electrocardiography wikipedia , lookup
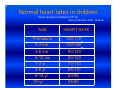
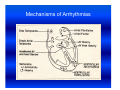
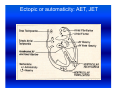
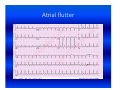
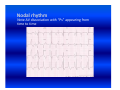
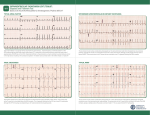
Cardiac arrhythmias in children Definition, identification and management Emphasis on SVT Otto H. P. Teixeira, MD, FRCPC, FACC Conflict of interest None Conduction system of the heart What is an arrhythmia? An arrhythmia is an abnormal heart rhythm • Sinus arrhythmia • Premature ventricular beats (PVCs) • Premature atrial beats (PACs) What is an Arrhythmia? • An arrhythmia is an abnormal heart rhythm What is an Arrhythmia? • An arrhythmia is an abnormal heart rhythm • Bradycardia is when the heart rate is too slow What is an Arrhythmia? • An arrhythmia is an abnormal heart rhythm • Bradycardia is when the heart rate is too slow • Tachycardia is when the heart rate is too fast for the age Normal heart rates in children Nelson Textbook of Pediatrics 19th ed. Elsevier/Saunders 2011: 1613‐16 AGE Premature 0-3 mo 3-6 mo 6-12 mo 1-3 yr 3-6 yr 6-12 yr 12+yr HEART RATE 120-170* 100-150* 90-120 80-120 70-110 65-110 60-95 55-85 Cardiac arrhythmia in children What's "too slow" ? • newborn: less than 80 beats a minute. • a trained teenage athlete: 50 beats a minute Cardiac arrhythmia in children Symptoms of bradycardia • • • • • Fatigue Dizziness Lightheadedness Fainting or near‐fainting spells In extreme cases, cardiac arrest may occur Supraventricular tachycardia (SVT) All forms of tachycardia except VT * * Van Hare G. Supraventricular tachycardia. In: Kliegman, Stanton, St. Geme, Schor, Behrman, eds. Nelson Textbook of Pediatrics 19th ed. Elsevier/Saunders 2011: 1613‐16 SVT in children Most common form of tachycardia in children: 1 : 250‐1000 (Gillette & Garson) SVT in children Most common form of tachycardia in children: 1 : 250‐1000 (Gillette & Garson) Narrow QRS complexes often with no discernible “P” wave HR: 150‐300 bpm and unvarying Mechanisms of Arrhythmias Classifying tachycardia: frequency Common: AV reentry Less common: atrial Uncommon: AV node reentry Rare: other SVT in children Re‐entrant: with accessory pathway without pathway SVT in children Re‐entrant: with accessory pathway without pathway Ectopic or automaticity: AET, JET AV re‐entrant tachycardias Reentry: most common etiology in children AVRT, AVNRT: age dependent Narrow QRS: usual 1:1 AV conduction: usual Sudden onset and cessation SVT in children Etiology Reentry: AVRT: most common in infants Accessory connection anywhere in the AV ring ‐ WPW, Mahaim tracts, others AVNRT: adolescents and adults AV peri‐nodal area: dual AV node “slow‐fast” AV node tracts SVT in children HR 215, occasional “P wave” seen SVT in children HR 187 bpm: P waves not discernible AV re‐entrant tachycardias • WPW: 1 : 1000 • 25 % of SVT orthodromic: narrow QRS during tachycardia antidromic: broad QRS (indistinguishable from VT) WPW AV re‐entrant tachycardias Orthodromic tachycardia using an accessory pathway in WPW Activation: AV node, HisPurkinje system, ventricle, accessory pathway, atria. P wave closely follows the QRS PR > RP AV re‐entrant tachycardias Antidromic tachycardia: antegrade conduction may lead to atrial fibrillation and VF: risk of SCD AV nodal re‐entrant tachycardia: AVNRT Dual pathways within the AV node “slow-fast” AV nodal tracts More common in adolescents and adults May cause syncope May respond to beta blockers and ablation* * Teixeira OH, Bilaji, Gillette PC. RF catheter ablation of atrioventricular nodal reentrant tachycardia in children. PACE 1994; 17:1621-1626. Management: SVT in children Evaluate General: IV, O2, capillary filling, BP 12‐lead ECG (may double speed): REENTRY? Stable? 1. Vagal maneuvers: infant ‐ modified diving reflex (ice to face); older ‐ gag, head immersion in water, Valsalva Management (cont’d) 2. Adenosine: 0.1 mg/kg mx 6 mg ECG rhythm should be running Management (cont’d) • Adenosine: 0.1 mg/kg mx 6mg. ECG rhythm should be running f a i l e d!? • Check tracing: reentry? check IV Double dose to mx. 12 mg Management (cont’d) 3. Consider synchronized DC cardioversion: 0.5‐2 Joules/kg failed!? • Check: equipment, paddles, position, coupling gel, contact • Repeat: double dose 4. Overdrive pacing: PM, esophageal lead 5. Other drugs: • Amiodarone: 5 mg/kg IV over 20‐60 min • Procainamide: 15 mg/kg IV over 30‐60 min Question • One month‐old male with narrow QRS heart rate of 320 bpm and tachypnea, poor peripheral pulse. Your treatment of choice includes all, EXCEPT: • 1. Vagal maneuvers, ie, ice to face. Question • One month‐old male with narrow QRS heart rate of 320 bpm and tachypnea, poor peripheral pulse. Your treatment of choice includes all, EXCEPT: • 1. Vagal maneuvers, ie, ice to face. • 2. Adenosine 0.1‐0.2 mg/Kg IV push Question • One month‐old male with narrow QRS heart rate of 320 bpm and tachypnea, poor peripheral pulse. Your treatment of choice includes all, EXCEPT: • 1. Vagal maneuvers, ie, ice to face. • 2. Adenosine 0.1‐0.2 mg/Kg IV push • 3. Verapamil 0.1 mg/Kg IV push Question • One month‐old male with narrow QRS heart rate of 320 bpm and tachypnea, poor peripheral pulse. Your treatment of choice includes all, EXCEPT: • 1. Vagal maneuvers, ie, ice to face. • 2. Adenosine 0.1‐0.2 mg/Kg IV push • 3. Verapamil 0.1 mg/Kg IV push • 4. Synchronized DC cardioversion: 0.5‐1.0 J/Kg Ectopic or automaticity: AET, JET SVT in children Etiology Automaticity: atrial ectopic tachycardia (AET) junctional ectopic tachycardia (JET) AET Atrial automatic focus: incessant , may be associated with cardiac dysfunction Insidious onset with “warm‐up” and “cool‐down” Abnormal “P” wave axis and PR interval Rate variation May have periods of sinus rhythm during sleep: P changes The P wave morphology depends on the position of the focus May appear like sinus tachycardia: RP interval is longer than the PR. The P waves may be blocked (not shown). AET AET • Rarely needs emergency treatment • Adenosine may work and helps diagnosis: P waves revealed during adenosine ‐ induced AV block Inappropriate sinus tachycardia (Bauernfeind R et al An Intern Med 1979; 91:702‐710) Chaotic or multifocal AET • • • • • • > 3 ectopic Ps Frequent blocked Ps Varying PR Occurs mostly in infants < 1 yr Difficult single drug management May improve spont by 3 yr of age Chaotic or multifocal AET • • • • • • > 3 ectopic Ps Frequent blocked Ps Varying PR Occurs mostly in infants < 1 yr Difficult drug management May improve spont by 3 yr of age JET • Uncommon; often post‐op • EKG: narrow QRS with V rate faster than A, and AV dissociation • Diff. to distinguish from VT: ”Why?” • Rates 180‐240 bpm • Congenital: rare may be seen pre‐natally: HR 370 bpm JET First‐degree AV block is typical and 2nd‐degree AVB is common. The tachycardia and degree of AV block are influenced by the autonomic tone Lead II of a ECG from a patient with postoperative JET. “Ps” are marked with blue lines and QRS complexes are in red JET • Difficult management: post‐op • several drugs may have to be tried in stepwise fashion: amiodarone, propafenone, sotalol Question In atrial ectopic tachycardia (AET): • 1. The etiology is automaticity Question • In atrial ectopic tachycardia (AET): • 1. The etiology is automaticity • 2. Warm‐up and cool‐down may be seen Question • • • • In atrial ectopic tachycardia (AET): 1. The etiology is automaticity 2. Warm‐up and cool‐down may be seen 3. P wave is present Question • • • • • In atrial ectopic tachycardia (AET): 1. The etiology is automaticity 2. Warm‐up and cool‐down may be seen 3. P wave is present 4. Blocked Ps may be seen Question • • • • • • In atrial ectopic tachycardia (AET): 1. The etiology is automaticity 2. Warm‐up and cool‐down may be seen 3. P wave is present 4. Blocked Ps may be seen 5. All of the above Atrial flutter Reentry: • Intra‐atrial reentry: note flutter waves (“saw‐tooth”), variable AV conduction Atrial flutter Atrial flutter: management • 1. Synchronized DC cardioversion: choice treatment • 2. Chronic flutter: risk of embolism > anticoagulartion • Digoxin, B‐blockers, Ca blockers: delay AV node conduction • Other drugs used to maintain sinus rhythm: procainamide, propafenene, amiodarone, sotalol Atrial flutter: management Atrial flutter: unstable 1. Synchronized DC cardioversion: half doses 2. Calcium channel blockers: Diltiazem: 0.25‐0.35 mg/kg over 2‐15 min (may repeat) Drip: 0.5‐0.15 mg/kg/h 3. Overdrive pacing: PM, esophageal lead 4. Other drugs: procainamide, amiodarone, sotalol Atrial flutter: management • Neonatal flutter: digoxin for 1 yr after which arrhythmia may not recur Atrial fibrillation • Uncommon • Often associarted with atrial problem: enlargement • Seen in older children with atrial enlargement or, rheumatic valve stenosis or surgery Atrial fibrillation: management • Rate control: Ca blockers • No digoxin if there is WPW • Acute: Procainamide, amiodarone, DC cardioversion Anticoagulation may be necesssary Conclusions SVT is the most common tachyarrhythmia in children The etiology is primarily reentry In older children it is usually well tolerated In infants it may be a life‐threatening emergency GOOD LUCK ! Nodal rhythm Note AV dissociation with “Ps” appearing from time to time Nodal bradycardia: HR 37bpm 3‐ year‐old girl with hyperthyroidism (Pediatr 1997; 100.2.e11). Flutter 1:1 conduction. Note negative flutter waves in V1‐V3 and II, III, aVF ATRIAL FLUTTER