* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Cardiovascular
History of invasive and interventional cardiology wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Heart failure wikipedia , lookup
Rheumatic fever wikipedia , lookup
Aortic stenosis wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Electrocardiography wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Artificial heart valve wikipedia , lookup
Coronary artery disease wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Heart arrhythmia wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
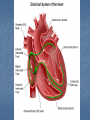
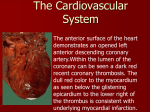
Heart Chapter 12 Heart System of a pump and pathway for blood to travel Arteries- vessels that carry blood away from the heart Veins- vessels that carry blood to the heart Capillaries are very small vessels that connect the two at the microscopic level - Exchange nutrients for waste Exchange O2 for CO2 Heart lies in the pericardial cavity in the lower portion of the mediastinum resting on the diaphragm. The inferior portion has a point or tip called the apex. Broad upper surface called the base The pericardium consists of two principle portions. 1- fibrous pericardium 2- serous pericardium Fibrous pericardium: tough and inelastic - rests on and attaches to diaphragm. - provides protection Serous pericardium: - thinner, delicate, double layered. - - - 1- Visceral pericardium: (epicardium) contacts the surface of the heart 2- Parietal pericardium: fused to the fibrous pericardium Pericardial cavity: separates two layers with pericardial fluid (lubricates membranes) - cardiac tamponade Heart consists of three layers: 1- Endocardium: lines inside of heart and heart valves 2- Myocardium: thick heart muscle. Blood supplied by coronary arteries. involuntary, striated, intercalated disks 3- Epicardium: smooth outer layer Heart is a double pump Right side of the heart is the receiving side. - pulmonary circulation Left side of the heart is the giving side. - systemic circulation (the body) Heart has four chambers Two upper chambers are called atria (sing. atrium) Right and left Two lower chambers called ventricles Right and left Right and left ventricles are separated by a thick walled structure called the Interventricular septum Blood flow between chambers and larger arteries pass through valves. Valves that connect the upper atria to the lower ventricles are termed atrioventricular valves (AV). There are two 1- Tricuspid valve. This “3 flapped” valve connects the right atria to the right ventricle 2- Bicuspid valve (mitral): This “2 flapped” valve connect the left atria to the left ventricle AV Valves Valves that connect the lower ventricles to the larger arteries carrying blood away from the heart are called semilunar valves. 1- Pulmonary semilunar valve: Valve located between the right ventricle and the pulmonary artery 2- Aortic semilunar valve: Valve located between left ventricle and aorta. Contraction of the heart is systole Relaxation of the heart is called diastole When the heart beats the atria contract first and together then the ventricles contract second and together. Deoxygenated blood drains into right atrium from - superior vena cava - inferior vena cava - coronary sinus (from heart) Blood is supplied to the heart by the first two branches of the aorta, right and left coronary arteries. These arteries arise from the base of the aorta and encircle the heart in the atrioventricular groove. Left coronary artery: anterior interventricular artery - supplies blood to the interventricular septum and anterior walls of both ventricles circumflex artery - supplies blood to the left atrium and the posterior walls of the left ventricle Right coronary artery: Posterior interventricular artery - runs to the apex and supplies blood to the posterior ventricular walls Marginal artery - supplies blood to the myocardium of the right side of the heart The myocardium needs a constant supply of oxygen in order for the heart to continually pump. Myocardium capillaries are branches of cardiac veins which join to form the coronary sinus, an enlarged vein which empties into the right atrium. Coronary veins: -Great cardiac vein, -Middle cardiac vein, -Small cardiac vein… … drains into cardiac sinus which drains into right atrium. Conduction and Pacemaker Conductility- ability to conduct an electrical impulse These impulses must be coordinated. Intercalated disks are electrical connectors that join the muscle fibers. Remember: Atria contract together then ventricles. Intrinsic 1- Sinoatrial node (SA node) pacemaker of the heart. 2- Atrioventricular (AV node) 3- Bundle of His- interventricular septum - right and left bundle branches 4- Purkinje fibers- ventricle walls Beating heart Cardiovascular (CV) center is located in the medulla of the brainstem. Sympathetic nervous system: cardiac accelerator nerves coming off of thoracic spinal cord segments. Increases heart rate Parasympathetic nervous system: Vagus nerve (CNX) coming off of medulla (brainstem). Decreases heart rate. Extrinsic ELECTROCARDIOGRAM (ECG or EKG) (Action Potential) Conduction system can be measured P QRS T P wave: SA node firing and atria contract (depolarization) QRS wave: atria relax (repolarization) and ventricles contract (depolarization) T wave: ventricle walls relax (repolarization) Myocardial infarction Elevated ST segment 1- Enlarged P-wave: Atrial hypertrophy 2- Missing or inverted P-wave: SA node damage. 3- Enlarged Q-wave: Myocardial infarct. 4- Enlarged R wave: Ventricular hypertrophy 5- Abnormal T-wave: Hypoxia or hyperkalemia (K+) 6- Inverted QRS: Premature Ventricular Contractions (PVC’s) 7- Elevated S-T segment: MI Sinus bradycardia Apart from fit, but otherwise normal individuals, there's a long list of situations where sinus bradycardia occurs, including: hypothermia; increased vagal tone (due to vagal stimulation or e.g. drugs); hypothyroidism; marked intracranial hypertension; obstructive jaundice, and even in uremia; structural SA node disease, or ischemia. Sinus tachycardia Always consider pain as a possible cause of tachycardia. Any cause of adrenergic stimulation (including pain); thyrotoxicosis; hypovolemia; vagolytic drugs (e.g. atropine) anemia, pregnancy; fever myocarditis Cardiac cycle Auscultation of the heart “Lubb – Dupp” “Lubb”: AV valves closing. (S1) Systole “Dupp”: Semilunar valves closing. (S2) -Diastole 1- Pulmonary valve: ribs 2 & 3 on left 2- Aortic valve: ribs 2 & 3 on right 3- Biscuspid valve: ribs 5 & 6 on left mid line of clavicle 4- Tricuspid valve: ribs 5 & 6 on right sternal margin Factors Affecting SV Preload Contractility Afterload Frank-Starling Law Inotropic: Contractility -Positive Inotropic Agents - Sympathetic NS - Digitalis - Glucagon (pancreas) - Epinephrine - Hypercalcemia - Negative Inotropic Agents - Hyperkalemia - Hypocalcemia - Cardiac hypoxia - Cardiac hypercapnia Chronotropic: Heart Rate - Postive Chronotropic Agents - Sympathetic stimulation - Epinephrine - Thyroid hormone - Hypocalcemia - Hypercapnia (acidosis) - Digitalis - Negative Chronotropic Agents - Parasympathetic NS - Acetylcholine - Hypokalemia - Hypercalcemia - Hypoxia Homeostasis