* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Hematology - kau.edu.sa
Survey
Document related concepts
Transcript
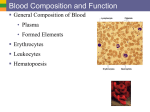
Hematology Mohamad H Qari, MD, FRCPA Hematology Cellular Components Components of Blood Red Blood Cells White Blood Cells Inflammatory process Coagulation Blood Typing Clotting disorders Hematology Spleen Blood Kidneys Hematopoietic System Bone Marrow Liver Hematopoeisis Three developmental periods Mesoblastic Hepatic Blood islands of yolk sac Primarily RBC production Embryonic hemoglobin produced At 6 weeks cell production in liver Fetal hemoglobin produced Spleen, thymus, lymph nodes also active prod. Myeloid At 5th month Bone Marrow becomes site of prod. Liver & spleen now Extramedullary Hemoglobin A (22) Requirements For Hematopoiesis Stem Cells Growth Factors Microenviroment Stem Cell theory Pluripotent stem cell originator of all cells Gives rise to cells committed to specific development Research supporting the theory PHSC has self-maintaining ability Committed cells differentiate continuously/ No Reverse Flow Stem cells in Research Pluripotent cells derived from: Cell mass of embryos at blastocyst stage (IVF) Fetal tissue from terminated pregnancy Application Identification of factors of cellular decision-making Development and testing of drugs Generation of cells and tissue for therapy Cytokines & Growth Factors Cytokines stimulate or inhibit Prevent apoptosis Colony-Stimulating Factors produced by many different cells Interleukins numbered according to discovery Components of Blood Plasma Components Plasma Water 90% Transport mechanism 90-92% water. 6-7% proteins 2-3% Fats Carbohydrates (glucose) Electrolytes Gases (O2, CO2) Chemical messengers Other 3% Protein 7% Cellular Components Pluripotent Stem Cell Myeloid Multipotent Stem Cells Common Lymphoid Stem Cells Unipotent Progenitors Lymphocytes WBC’s Basophils Eosinophils Neutrophils Monocytes RBC’s Thrombocytes Platelets Erythrocytes Erythropoietin Components of Blood Red Blood Cells Erythrocyte Hemoglobin – O2 bearing molecule Comprised of 4 subunits: • Globin (binds to 1 O2 molecule) • Heme (iron) 100% saturation = 4 globin subunits carrying O2 • Each gram of hemoglobin = 1.34 ml O2 Cellsalive.com Blood Products and Blood Typing Blood Types Antigens A, B, AB, O Rh factor Rh+ = ~85% Rh- = ~15% Blood transfusion Components of Blood Red Blood Cells (cont.) Oxygen Transport Oxy-hemoglobin dissociation curve 2,3-DPG Components of Blood White Blood Cells (Leukocytes) Margination Phagocytosis The macrophage is using its internal cytoskeleton to envelop cells of the fungus Candida albicans. Components of Blood Leukocytes (cont.) White Blood Cell Count Leukopoiesis Granulocytes Neutrophil Basophil Eosinophil Monocytes Lymphocytes Human Neutrophil: Phagocytosis of Strep pyogenes Components of Blood Leukocytes (cont.) Immunity Subpopulation of lymphocytes known as T cells and B cells T cells develop cellular immunity. B cells produce humoral immunity Components of Blood Inflammatory Process MAST CELLS. Immunoglobulin E antibody IgE, Antigens Antigens stick to the mast cell IgE antibodies, causing granules in the mast cell to fire their contents into the surrounding tissue. This releases a host of inflammatory materials - leukotrienes, tumor necrosis factor, interleukin-4 and other cytokines that turn on other inflammatory cells. These materials cause fluid to leak from the capillaries and white cells including neutrophils, T cells and eosinophils to leave the circulation. The end result is a "local inflammatory response", a red, itchy welt. Cellsalive.com Components of Blood Hemostasis3 mechanisms Vascular spasm Platelet plug Contraction of tunica media Platelet aggregation Coagulation Formation of fibrin clot Components of Blood Hemostasis (cont.) Fibrinolysis Lysis of clot (plasmin) Thrombosis Thrombolytics Medications affecting clot formation Alter the enzyme on the platelet. Affect the coagulation cascade. Enhance clotting. Coagulation Cascade Synopsis This scanning electron micrograph shows the fine structure of a blood clot. Platelets released from the circulation and exposed to the air use fibrinogen from the blood plasma to spin a mesh of fibrin. General Assessment Management Focused History and Physical Exam SAMPLE history Hematological disorders are rarely the chief complaint. Physical exam Evaluate nervous system function. Skin signs General Assessment - Management Physical Exam (cont.) Lymphatic signs Gastrointestinal signs Musculoskeletal signs Arthralgia (rheumatoid arthritis) Hemarthrosis Cardiorespiratory signs Epistaxis Atraumatic bleeding gums Thrush Atraumatic splenic/hepatic pain Tachycardia, cx pn, dyspnea - CHF Genitourinary signs Hematuria Menorrhagia Infection Blood Products and Blood Typing Blood Typing - ABO Blood type Antigen present Antibody on erythrocyte present in serum O AB B A None A and B B A Anti-A, Anti-B None Anti-A Anti-B Blood Products and Blood Typing Compatibility Among ABO Blood Groups Reaction with serum of Recipient Donor Cells AB B A O AB B A O - + + - + + - + + + - -= no reaction + = reaction Blood Products and Blood Typing Brady; Paramedic Care Principles and Practice Diseases of Erythrocytes Anemias Anemia is a sign, not a separate disease process. Signs and symptoms may not be present until the body is stressed. Differentiate chronic anemia from acute episode. Treat signs and symptoms. Maximize oxygenation and limit blood loss. Establish IV therapy if indicated. Diseases of Erythrocytes Brady; Paramedic Care Principles and Practice Diseases of Erythrocytes Sickle Cell Disease Normal red cells maintain their shape as they pass through the capillaries and release oxygen to the peripheral tissues (upper panel). Hemoglobin polymers form in the sickle rell cells with oxygen release, causing them to deform. The deformed cells block the flow of cells and interrupt the delivery of oxygen to the tissues (lower panel). Diseases of Erythrocytes Sickle Cell Disease (cont.) Sickle cell crises Vaso-occlusive Hematological Musculoskeletal/abdominal pain Priapism Renal/cerebral infarctions Lowered hemoglobin Splenic sequestration Infectious Management Follow general treatment guidelines prn. Consider analgesics. Diseases of Erythrocytes Polycythemia Overproduction of erythrocytes. Occurs in patients > 50 years old or with secondary dehydration. Most deaths due to thrombosis Results in bleeding abnormalities: Epistaxis, spontaneous bruising, GI bleeding. Management: Follow general treatment guidelines. Diseases of Leukocytes Leukopenia/Neutropenia Too few white blood cells or neutrophils. Follow general treatment guidelines and provide supportive care. Leukocytosis An increase in the number of circulating white blood cells, often due to infection. Leukemoid reaction Diseases of Leukocytes Leukemia Cancer of hematopoietic cells Initial presentation Acutely ill, fatigued, febrile and weak, anemic. Thrombocytopenia Often have a secondary infection. Management Follow general treatment guidelines. Utilize isolation techniques to limit risk of infection. Diseases of Leukocytes Lymphomas Cancers of the lymphatic system Presentation Hodgkin's Non-Hodgkins Swelling of the lymph nodes Fever, night sweats, anorexia, weight loss, fatigue, and pruritis Management Follow general treatment guidelines. Utilize isolation techniques to limit risk of infection. Clotting Disorders Thrombocytosis and Thrombocytopenia Thrombocytosis An abnormal increase in the number of platelets Thrombocytopenia An abnormal decrease in the number of platelets Sequestration Destruction (ITP) Decreased production Management Provide supportive care and follow general treatment guidelines. Clotting Disorders Hemophilia Deficiency or absence of a blood clotting factor Deficiency of factor VIII causes hemophilia A. Deficiency of factor IX causes hemophilia B. Deficiency is a sex-linked, inherited disorder. Defective gene is carried on the X chromosome. Signs & Symptoms Numerous bruises, deep muscle bleeding, and joint bleeding. Clotting Disorders Hemophilia (cont.) Management Treat the patient similarly to others. Administer supplemental oxygen. Establish IV access. Be alert for recurrent or prolonged bleeding, and prevent additional trauma. Von Willebrand’s Disease Deficient component of factor VIII Generally results in excessive bleeding. Generally is not serious; provide supportive care. Clotting Disorders Disseminated Intravascular Coagulation Components of Blood Leukocytes (cont.) Autoimmune disease May be specific or general Alterations in the immune process Immunosuppression HIV Anti-rejection medication Chemotherapy/Cancer System activation of coagulation cascade. Anticoagulants/Antiplatelets Classifying agents Anticoagulants Antiplatelets Block synthesis and activation of clotting factors Interfere with platelet aggregation or activation Fibrinolytics Dissolve fibrin component of thrombi Anticoagulants/Antiplatelets Anticoagulants Warfarin Unfractionated Heparin Blocks activation of Vit K Interferes w/ coagulation factors II, VII, IX, and X Binds antithrombin III (AT-III) Inhibits coagulation factors IX and X and thrombin Hirudin (medicinal leech) Prevents thrombin binding Anticoagulants/Antiplatelets Antiplatelets Aspirin Prevents platelet activation through cyclooxygenase blockade. Prevents production of thromboxane A2 Allows prostacyclin synthesis Ticlodipine Deforms platelet membrane fibrinogen receptor Anticoagulants/Antiplatelets Antiplatelets (cont.) Glycoprotein IIb-IIIa Receptor Inhibitors G IIb-IIIa = platelet membrane receptor of fibrinogen Abciximab Eptifibatide Tirofiban Fibrinolytics Activate plasminogen to plasmin = fibrinolysis Streptokinase Anistreplase Tissue Plasminogen Activator Reteplase Urokinase Hemorrhage Class I Class II Class III Class IV Blood Loss (ml) Up to 750 750-1500 1500-2000 >2000 Blood Loss (% volume) Up to 15% 15%-30% 30%-40% >40% Pulse <100 >100 >120 >140 BP Normal Normal Decreased Decreased Pulse Pressure Normal or increased Decreased Decreased Decreased Resp. Rate 14-20 20-30 30-40 >35 Urine Output (ml/hr) >30 20-30 5-15 Negligible Mental Status Slightly anxious Mildly anxious Anxious, confused Confused, lethargic Fluid Replacement (3:1) rule Crystalloid Crystalloid Crystalloid and Crystalloid and blood blood Transfusion Reactions Hemolytic Reaction Signs & Symptoms Facial flushing, hyperventilation, tachycardia, hives, chest pain, wheezing, fever, chills, and cyanosis Treatment Stop transfusion, change all IV tubing, and initiate IV therapy with normal saline or lactated Ringer’s. Consider furosemide, dopamine, and diphenhydramine. Transfusion Reactions Febrile Non-hemolytic Reactions Signs & Symptoms Headache, fever, and chills Treatment Stop transfusion, change all IV tubing, and initiate IV therapy with normal saline or lactated Ringer’s. Consider Diphenhydramine and an antipyretic. Observe closely to ensure reaction is nonhemolytic.