* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Non Specific Host Defense Mechanisms
Rheumatic fever wikipedia , lookup
Molecular mimicry wikipedia , lookup
Polyclonal B cell response wikipedia , lookup
Adaptive immune system wikipedia , lookup
Sjögren syndrome wikipedia , lookup
Immune system wikipedia , lookup
Cancer immunotherapy wikipedia , lookup
Adoptive cell transfer wikipedia , lookup
Psychoneuroimmunology wikipedia , lookup
Complement system wikipedia , lookup
Inflammation wikipedia , lookup
Immunosuppressive drug wikipedia , lookup
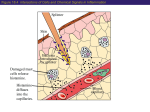
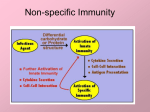
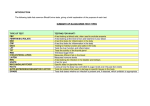
Nonspecific Host Defense Mechanisms BY Prof. DR. Zainalabideen A. Abdulla, DTM&H., MRCPI, Ph.D., FRCPath. (U.K.) Learning Objectives Host defense mechanisms Non-Specific Defense: 1. First line of defense - Intact skin & mm 2. Second line of defense - Inflammation & phagocytosis Specific Defense: 3. Third line of defense - The immune system First Line of Defense Skin and Mucous Membranes • Physical/mechanical barriers e.g. Bacteria can not penetrate intact skin, or intact mm/sticky mucus produced (by goblet cells) entraps invaders • Certain helminthes able to penetrate skin, e.g. Hookworm, Schistosomiasis Cellular and chemical factors Intact skin • Skin dryness: Inhibits pathogens • Acidity (pH ̴ 5.0) • Temperature (< 37Celsius) • Oily Sebum (sebaceous glands)- Fatty acids toxic to pathogens • Perspiration- Flushing organisms - Lysozyme degrades peptideglycan specially of G+ • Sloughing off of dead skin cont./…cellular and chemical factors Mucus membranes • Substances kill or inhibit bacteria: Lysozyme (saliva, tears, nasal secretions) Lactoferrin (Binds iron required by pathogens) Lactoperoxidase (toxic superoxide radicals) • Rapidly dividing cells/ expelled with microbes • Respiratory tract: Hair, mm, nose, cilia • GIT: Digestive enzymes, acidity of the stomach (pH ̴ 1.5), alkalinity of intestines • GUT: Urination, low vaginal pH Microbial Antagonism • Nonspecific host defense/ Factors mentioned • Superinfection: When microbiota reduced Second Line Chemical and Cellular • Transferrin • Interferon • Acute phase proteins • Inflammation • Fever • Complement system • Cytokines • Phagocytosis Transferrin • Glycoprotein; synthesized by the Liver • Store/deliver iron to host • Sequestered: Deprive pathogens from iron • Increased: In systemic bacterial infections Fever • Normal = 36.2 – 37.5 (mean: 37) Celsius • Fever = > 37.8 • Substance: Pyrogens (pyrogenic) e.g. Endotoxin, IL-1 (endogenous pyrogen) cont./… Fever augmentation of host defenses • Stimulate WBC • Reducing plasma iron levels • Production of IL-1: Stimulate lymphocytes Fever development during infectious disease • Gram negative sepsis • Endotoxin • Phagocytes ingest endotoxin IL-1 • Prostaglandins Up hypothalamic thermostat • Vasoconstriction; temp decreases when IL-1 Interferons • Small anti-viral proteins • Produced by virally infected cells • “Interfere” with viral replication • Types: Alpha, beta, gamma • Stimulants: Viruses, tumors, bacteria, cells“F. • Alpha: B-cells, monocytes, macrophages Beta: Fibroblasts, other virus-infected cells Gamma: T-cells, NK cells • Save surrounding cells; spread inhibited • Not specific, but species (animal) specific c ont cont./… interferons • Genetically produced by bacteria in which human genes inserted • Use: Warts, H. simplex, Hepatitis B & C, and Cancer (leukemia, lymphoma, Kaposi sarcoma in AIDS) • Activate NK cells • Cause: Flulike (malaise, myalgia, chills, fever) The complement system “C” • 30 different proteins (C1 – C9 & others) • “Complementary” to immune system • Complement cascade (stepwise) • Consequences of “C” activation: 1. Initiation/amplification of inflammation 2. Attraction of phagocytes to site 3. Activation of leukocytes 4. Lysis of bacteria/ foreign cells (target) 5. Opsonization (increased phagocytosis) Opsonization • Opsonins: Antibodies, C3b • Opsonins attach to surface of target cells • Phagocytes have receptors to opsonins • The process facilitate phagocytosis of certain particles such as encapsulated bacteria. Complement pathways: 1. Classical (C1-C9): Specific immunity 2. Alternative “ Properdin” (C3-C9): Nonspecific (innate) immunity Acute phase protein • Increased: Infections, inflammation, tissue injury • Function: - Enhance resistance to infections - Promote tissue repair • Examples: C-reactive protein (inflammation marker), serum amyloid A protein, protease inhibitors, coagulation proteins Cytokines • For cells’ communication (chemical messages) • Cells “sense” cytokines by surface receptors • Roles/examples: - Chemo-attractants (e.g. phagocytes) - Role in host defense Inflammation (inflammatory response) • Vasodilatation • Increased vascular permeability; plasma escape • Leukocytes escape • Purpose: - Localize infection - Prevent spread of invaders - Neutralize toxins - Aid in repair of tissue damage • Cardinal (main) 4 signs: redness, heat, pain, swelling (edema); + Pus, Function loss cont./… cont./… inflammation Physiological events • Vasodilatation (histamine & PG)- endothelial cells stretches/separate > Blood Redness, Heat, Plasma escape Edema • Influx of phagocytes (chemotactic agents) • Pain/tenderness (nerve damage: Injury, PG, Toxins, pressure by edema) cont./… cont./… inflammation • Inflammatory exudate: Fluid + cellular debris • Purulent exudate: Thick greenish yellow exudate + live/dead leukocytes (PUS) e.g. Staphylococci, Streptococci • Pseudomonas aeruginosa Green pus (due to bluish pigment of m.o.: Pyocyanin) • Lymphatic system: - Draining circulating fluid - Transport fat from GI - Filter: T, B, macrophages - Antibodies/others sub. Phagocytosis • Engulf (phagocytosis) • Professional phagocytes ( M & N) • Phagocytic granulocytes (N & E; 1st >> 2nd) • Monocytes Macrophages - Wandering macrophages - Fixed macrophages: Histiocytes in C.T., Liver: Kupffer cells, Brain: microglia • Phagocytosis steps: Chemotaxis, Attachment, Ingestion, Digestion Chemotaxis • Chemotaxis (to site): Chemotactic Agent (Chemokines) • Produced during complement activation • Move along concentration gradient • Attract: N, Mo, E Attachment • Attachment to objects (microbes) by receptors • Role of opsonization (Ab & C) Ingestion • Surround objects by pseudopodia & FUSE (Phagosome “membrane bound vesicle”) Digestion • Phagosome + Lysosome Phagolysosome • Lysosomes: Membrane-bound vesicles with digestive enzymes: - Lysozyme, Beta-lysin, Lipase, Protease, Peptidase, DNAses, RNases Degrade CHO, lipids, proteins, and nucleic acids • Neutrophils: - NADPH oxidase reduces Oxygen Superoxide Anions, Hydroxyl Radicles, Hydrogen Peroxide, and Singlet Oxygen/cont cont./… digestion • Myeloperoxidase (from lysosomes) in the presence of hydrogen peroxide & chloride ion Hypochlorous acid (potent microbicidal agents) • Example: Phagocytosis of Giardia lamblia by neutrophils Pathogens escape destruction • Capsule: Anti-Phagocytic • Leukocidin by m.o.: Kills phagocytes • Wax protects: Mycobacterium tuberculosis • Survival inside phagocytes: Transported e.g. Salmonella spp., Brucella abortus, Toxoplasma gondii, Leishmania spp. Disorders affecting phagocytic and inflammatory processes Leukopenia • Low WBC numbers; Neutropenia (low N No.) • Bone marrow injury: Radiation, drugs, nutritional deficiencies, congenital stem cell defects Disorders of Leukocyte Mobility/Chemotaxis • Defect in actin production (for mobility) • Corticosteroids • Chediak-Higashi syndrome: N chemotaxis affected, PMN abnormal lysosomes (not fuse to phagosomes) resulting in decreased bactericidal activity + albinism, CNS abnormalities, recurrent bacterial infections Disorders of intracellular killing • Deficiency of myeloperoxidase (MP) • Inability to generate: Superoxide anion, hydrogen peroxide (HP), Hypochlorite • Chronic Granulomatous Disease (CGD): - Fatal genetic disorder - Repeated bacterial infections - PMNs can ingest bacteria, but can not kill - Forms: Unable to produce HP or lack MP Additional Factors: See Table