* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download 203.transplantation
Drosophila melanogaster wikipedia , lookup
DNA vaccination wikipedia , lookup
Psychoneuroimmunology wikipedia , lookup
Monoclonal antibody wikipedia , lookup
Immune system wikipedia , lookup
Adaptive immune system wikipedia , lookup
Cancer immunotherapy wikipedia , lookup
Molecular mimicry wikipedia , lookup
Adoptive cell transfer wikipedia , lookup
Innate immune system wikipedia , lookup
Polyclonal B cell response wikipedia , lookup
Human leukocyte antigen wikipedia , lookup
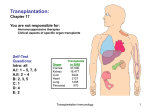
Major Histocompatibility Complex and Transplantation • Major histocompatibility complex (MHC) proteins were discovered for the first time with the beginning of tissue transplantation • The success of tissue and organ transplantation depends upon the donor’s and recipient’s “human leukocyte antigens” (HLA) encoded by HLA genes • These proteins ( MHC ) are allo-antigens which means : the same gene locus ( site ) in different individuals of the same species will express different antigens ( proteins ) , so when one antigen of one individual is transported to another who doesn’t have it , it will induce immune response against it ] like blood groups [ Major Histocompatibility Complex and Transplantation • Genes for HLA proteins are clustered in the MHC complex region located on the short arm of chromosome 6 • Three genes HLA-A, HLA-B and HLA-C code for Class I MHC proteins • HLA-D loci encode for Class II MHC proteins ie, DP, DQ and DR Major Histocompatibility Complex and Transplantation • Each individual has two “haplotypes” ie, ( two sets of these genes one paternal and one maternal ) • These genes are very diverse “polymorphic” – There is about 47 HLA-A genes – There is about 88 HLA-B genes - There is about 29 HLA-C genes – There is about More than 300 HLA-D genes So the child will have a different combination of genes different from his parents and from any other person ( except for identical twins ) Major Histocompatibility Complex and Transplantation • • • • Minor HLA genes – are unknown They mount a weak immune response Play role in chronic rejection of a graft There are no laboratory tests to detect minor antigens • Class III MHC locus found between MHC I & II regions • Encode for TNF, lymphotoxin, complement proteins ( C2 and C4 ) MHC Class I, II & III Genes MHC Class I Proteins • They are glycoproteins found on surface of virtually all the nucleated cells • The A locus which have HLA-A genes encode 20 different proteins , B locus having HLA-B genes will encode 40 different proteins and C locus will encode 8 different proteins • So the different proteins will make the individuals differ from each other • all class I proteins are composed of a heavy chain (α1 + α2 + α3 ) bound to a 2-microglobulin molecule • The heavy chain is highly polymorphic and has a hypervariable region at N-terminal – Polymorphism – self and non-self recognition – Constant regions react with CD8 protein of Tcytotoxic MHC Class I Protein The polymorphism happen in the α chain ( heavy chain ) And the α chain ( specially α3 domain ) has transmembrane part which contact with the intracellular part of α chain Class II MHC Proteins • They are glycoproteins normally found on the surface of antigen presenting cells such as ( marophages, B cells, dendritic cells of spleen and Langerhans cells of skin • They are highly polymorphic • Composed of two polypeptide chains bound noncovalently • They have hypervariable regions leading to Polymorphism MHC Class II Protein Here the polymorphism found in both α and β chains And both α and β chains have a transmembrane part to contact it’s intracellular part Major Histocompatibility Complex and Transplantation • Both chains of Class II MHC proteins are encoded by the MHC locus • Constant regions of both the peptides interact with CD4 proteins of helper T cells Biologic Importance of MHC • Tc kills virus infected cells in association with class I MHC proteins • Helper T cell recognize antigen in association with class II MHC proteins • This is called MHC restriction • Success of organ transplant is determined by compatibility of the MHC genes between the donor and the recipient Transplantation antigens Compatible , so there is no immune response against the graft Non – compatible , so there is immune response against the graft Transplantation Transplantation • Types of transplants: – Autografts or ( Autologous grafts ) • Donor and recipient are the same person • Common in skin grafting; bone marrow – Syngeneic grafts or ( isograft ) • Donor and recipient are genetically identical • Animal models; identical twins Transplantation • Types of transplants: – Allogeneic grafts ( allograft ) very imp • Donor and recipient are in the same species, but genetically unrelated • Common : heart, lung, kidney, liver graft – Xenogeneic grafts ( xenograft ) • Donor and recipient are different species • Like graft from Animal to humans – Artificial grafts Like artificial joints and skin Transplantation • Major Barrier to transplantation is the immune response – T cells play primary ( main ) role in graft rejection – B cells can/do play a role – Classic adaptive/acquired immune response • Memory • Specificity 1st set versus 2nd set reactions Transplantation In the previous picture :1- in column ( a ) there is in autograft of epidermis from the same person , so there will be no immune response against it and no rejection 2- in column ( b ) there is allograft from human to another human , there will be a rejection if they don’t match , but it will take long time ( up to 14 days ) because he exposed to it for the first time ( hens called first- set rejection ) 3 – in column ( c ) we repeat the step 2 but the rejection happen faster because there is memory cell which directly get activated ( called second-set rejection ) it is always faster ( up to 6 days ) 1st set versus 2nd set reactions Role of cell mediated responses Unprimed syngeneic recipient Transplantation In the previous slide There is 2 syngeneic mice ( like identical twins ) , the first one get skin graft that doesn,t match , so after 14 days the grafted skin get rejected by the first-set rejection Now the T cells have memory cells , if we transplant another skin graft to the same mouse the rejection will happen in 6 days due to the memory cells If we transport the T memory cells to the other mouse who didn’t have skin graft , and then give him a skin graft it will reject it in 6 days due to the presence of T memory cells And that tells that T cells have a main role in graft rejection Role of CD4+ versus CD8 T+ cells Injecting recip. mice with mab to deplete one or both types of T cell Transplantation ] In the previous slide [ This slid will tell you which type of T cell is dominant or have the main function in graft rejection : 1- when we transplant a graft that doesn’t match and give the recipient an ( anti CD8 ) the graft will stay intact for about 15 days before it get rejected 2 – when we transplant a graft that doesn’t match and give the recipient an ( anti CD4 ) the graft will stay intact for about 30 days before it get rejected That tells you that the CD4 cell have the main function in graft rejection And if we block both CD4 and CD8 the grafr will persist for 60 days Transplantation • T cells play primary role in 1st and 2nd set rejection reactions – Nude mice ( don’t have T cells ) accept allografts – B cell deficient mice reject allografts , because they still have T cells A Nude mouse has a transplant of rabbit skin Mechanisms involved in Graft Rejection Sensitization stage = = = = Effector stage Rejection Response Clinical manifestations of graft rejection I. Hyperacute rejection: very quick ( within minutes ) II. Acute rejection: about 10 days (cell mediated) III. Chronic rejection: months-years (both) by minor HLA gene Clinical manifestations of graft rejection Hyperacute rejection ( mediated by humoral immunity ) : In this condition , the recipient already have antibodies against the graft even before the transplant , so when we transplant the organ the preexisting antibodies will attach to the organ and activate the complement system to destroy the organ within minutes Acute rejection ( cell mediated ) : In this condition , the graft persist for about 10 days ( in contrast to hyperacute which is in minutes ) and that due to the action of T cells this reaction is cell mediated so take longer time to multiply and arrive to the site of graft Chronic Rejection ( cell mediated and humoral immunity ) – This occurs months to years after engraftment – Main pathologic finding in chronic rejection is atherosclerosis of the vascular endothelium – Main cause of chronic rejection is not known • Minor histocompatibility antigen miss match • Side effects of immunosuppressive drugs Graft-versus-Host (GVH) Reaction • Some times the patient need a transplanted bone marrow or thymus which are have a large number of lymphocytes from the donor • So when the graft is allograft ( from the same species but not identical ) the transplanted lymphocyte ( specially T cells ) will lock around in the recipient body if it didn,t find a match in the MHC it will attack the recipient body because it look foreign bodies for it • so in this case instead of making the patient healthier , he will become worse Graft-versus-Host (GVH) Reaction The donor’s cytotoxic T cell will play a major role in destroying the recipient’s cells Symptoms are: maculopapular rash, jaundice, hepatosplenomegaly and diarrhea GVH reactions usually end in infections and death So in brief the transplanted organ will work against or versus the host Maculopapular rash HLA Typing in the Laboratory • Prior to transplantation , laboratory test commonly called as HLA typing or tissue typing is performed to determine the closest MHC match between the donor and recipient is performed • Methods applied in this test is : – – – – DNA sequencing by Polymerase Chain Reaction (PCR) Serologic Assays Mixed Lymphocyte Reaction (MLR) Crossmatching – (D) lys + (R) serum + complement ( very important ) Tissue Matching Effect of HLA class I & II matching on survival of kidney grafts Zero = means no difference So the MHC match Notice that class II is more important than class I So when it is zero or close to zero the survival rate increase Tissue Matching Serological Method In this test you take the recipient’s serum which contain antibodies and then add to it the donor’s HLA antigens Then add complement to them , if the antibodies bind to the HLA antigens the complement will be activated and will attack the donor’s cells and then add a dye to confirm the lysis If the dye radiate ( visible ) that mean the recipient will reject the graft , if not he will except it Tissue Matching Mixed Leukocyte Reaction (MLR) In this test we will take leukocytes from the recipient and the donor and but them in tube , if the MHC in the different leukocytes don’t match they will be activated against each other and proliferate , then we add a radioactive material ( thymidine ) which will be incorporated into the DNA and it will radiate ( become visible ) , if the MHC match ther will be no proliferation and the thymidine will not be taken by the cell’s DNA Tissue Matching Very important General Immunosuppression Therapy After the transplantation 1) Mitotic inhibitor : azathioprine ( pre & post ) 2) Corticosteroids: (+ 1) 3) Cyclosporin A, FK506: IL-2 and IL-2R 4) Total lymphoid irradiation Immunosuppresive Therapy Immunosuppresive Therapy Cyclosporin FK506 Immunosuppresive Therapy Here you see the survival of the graft with and without the immunosuppresive therapy The blue = with The black = without Specific Immunosuppression Therapy a) Mabs (Monoclonal antibody ) to T cell components or cytokines b) Agents that blocking co-stimulatory signal Immunosuppresive Therapy • Downsides – Must be maintained for life – Toxicity – Susceptibility to infections – Susceptibility to tumors ( due to inactivation of CD8 )