* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download of Tumor Origin Influence in Colorectal and Renal Cell Carcinoma
Lymphopoiesis wikipedia , lookup
Hygiene hypothesis wikipedia , lookup
Immune system wikipedia , lookup
Polyclonal B cell response wikipedia , lookup
Adaptive immune system wikipedia , lookup
Immunosuppressive drug wikipedia , lookup
Innate immune system wikipedia , lookup
Psychoneuroimmunology wikipedia , lookup
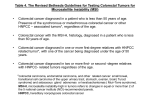
Published OnlineFirst June 19, 2013; DOI: 10.1158/1078-0432.CCR-12-3847 Characteristics and Clinical Impacts of the Immune Environments in Colorectal and Renal Cell Carcinoma Lung Metastases: Influence of Tumor Origin Romain Remark, Marco Alifano, Isabelle Cremer, et al. Clin Cancer Res 2013;19:4079-4091. Published OnlineFirst June 19, 2013. Updated version Supplementary Material Cited Articles E-mail alerts Reprints and Subscriptions Permissions Access the most recent version of this article at: doi:10.1158/1078-0432.CCR-12-3847 Access the most recent supplemental material at: http://clincancerres.aacrjournals.org/content/suppl/2013/06/19/1078-0432.CCR-12-3847.DC1.html This article cites by 50 articles, 22 of which you can access for free at: http://clincancerres.aacrjournals.org/content/19/15/4079.full.html#ref-list-1 Sign up to receive free email-alerts related to this article or journal. To order reprints of this article or to subscribe to the journal, contact the AACR Publications Department at [email protected]. To request permission to re-use all or part of this article, contact the AACR Publications Department at [email protected]. Downloaded from clincancerres.aacrjournals.org on October 10, 2014. © 2013 American Association for Cancer Research. Published OnlineFirst June 19, 2013; DOI: 10.1158/1078-0432.CCR-12-3847 Clinical Cancer Research Human Cancer Biology Characteristics and Clinical Impacts of the Immune Environments in Colorectal and Renal Cell Carcinoma Lung Metastases: Influence of Tumor Origin Romain Remark1,2,3,4, Marco Alifano3,5, Isabelle Cremer1,2,3, Audrey Lupo1,2,3,4,5, Marie-Caroline Dieu-Nosjean1,2,3, Marc Riquet3,6, Lucile Crozet1,2,3, Hanane Ouakrim1,2,3, Jeremy Goc1,2,3, jou2,8, Laure Gibault3,9, Virginie Verkarre3,10, Jean-François Re gnard3,5, lie Cazes3,6, Jean-François Fle Aure 5 3,6 1,2,3 1,2,3 , Catherine Sautes-Fridman , Olivier-Nicolas Pages , Stephane Oudard , Bernhard Mlecnik Wolf-Herman Fridman1,2,3,7, and Diane Damotte1,2,3,5 Abstract Purpose: If immune cells are involved in tumor surveillance and have a prognostic impact in most primary tumors, little is known about their significance in metastases. Because patients’ survival is heterogeneous, even at metastatic stages, we hypothesized that immune cells may be involved in the control of metastases. We therefore characterized the tumor immune microenvironment and its prognostic value in colorectal and renal cell carcinoma (RCC) metastases, and compared it to primary tumors. Experimental Design: We analyzed by immunohistochemistry (n ¼ 192) and qPCR (n ¼ 32) the immune environments of colorectal carcinoma and RCC lung metastases. Results: Metastases from colorectal carcinoma and RCC have different immune infiltrates. Higher densities of DC-LAMPþ mature dendritic cells (P < 0.0001) and lower densities of NKp46þ NK cells (P < 0.0001) were observed in colorectal carcinoma as compared to RCC metastases, whereas densities of T cells were similar. High densities of CD8þ and DC-LAMPþ cells correlated with longer overall survival (OS) in colorectal carcinoma (P ¼ 0.008) and shorter OS in RCC (P < 0.0001). High NK-cell densities were associated with improved survival in RCC (P ¼ 0.002) but not in colorectal carcinoma. Densities of immune cells correlated significantly from primary to relapsing metastases for the same patient. A TH1 orientation was found in colorectal carcinoma metastases, whereas a heterogeneous immune gene expression was found in RCC metastases. Conclusions: Our results show a major prognostic value of the immune pattern (CD8þ/DC-LAMPþ cell densities) in colorectal carcinoma and RCC, reproducible from primary to metastatic tumors, although with opposite clinical impacts, and highlight the role of the tumor cell in shaping its immune environment. Clin Cancer Res; 19(15); 4079–91. 2013 AACR. et de la Recherche Authors' Affiliations: 1Institut National de la Sante dicale (INSERM), U872, Centre de Recherche des Cordeliers; 2UniMe 3 Paris Des Pierre et Marie Curie-Paris 6, UMRS 872; Universite versite Denis Diderot-Paris 7; 5Services cartes-Paris 5, UMRS 872; 4Universite ^ pital Ho ^ tel Dieu; d'anatomie-pathologique et de chirurgie thoracique, Ho 6 Services d'anatomie-pathologique, oncologie et de chirurgie thoracique; 7 ^ pital Europe en Georges Pompidou; Service d'Immunologie Biologique, Ho 8 ^ pital Saint-Antoine; 9Service d'anaService d'anatomie-pathologique, Ho 10 ^ pital Cochin; and Service d'anatomie-patholotomie-pathologique, Ho ^ pital Necker-Enfants Malades, AP-HP, Paris, France gique, Ho Note: Supplementary data for this article are available at Clinical Cancer Research Online (http://clincancerres.aacrjournals.org/). W.-H. Fridman and D. Damotte contributed equally to this article. Corresponding Author: Diane Damotte, INSERM U872, Centre de decine, 75006 Paris, Recherche des Cordeliers, 15 rue de l'Ecole de Me France. Phone: 33-1-42-34-87-12; Fax: 33-1-42-34-86-41; E-mail: [email protected] doi: 10.1158/1078-0432.CCR-12-3847 2013 American Association for Cancer Research. Introduction Immune cells are found in human solid tumors, and the immune pattern of the tumor microenvironment is a major predictor of patient survival in a large array of primary tumors (1). Thus, a high density of T cells with a TH1 and CD8þ T cells cytotoxic orientation or of mature dendritic cells (DC) are beneficial in most cancers, especially in colorectal (2–4), lung (5), breast (6), gastric (7), pancreatic (8), urothelial (9), hepatocellular (10), esophageal (11), ovarian cancer (12) and melanoma (13), with the exception of renal cell carcinoma (RCC) in which high densities of CD8þ and CD45ROþ cells are associated with poor prognosis (14, 15). Even if metastatic spreading is the main cause of death by cancer (16), metastatic patients have heterogeneous survival (17). A classical view of cancer progression is that genetic modifications (18) may allow malignant cells to www.aacrjournals.org Downloaded from clincancerres.aacrjournals.org on October 10, 2014. © 2013 American Association for Cancer Research. 4079 Published OnlineFirst June 19, 2013; DOI: 10.1158/1078-0432.CCR-12-3847 Remark et al. Translational Relevance This article demonstrates for the first time, in a large cohort of patients with lung metastasis from 2 different primary tumors, colorectal and renal cell carcinoma, that densities of CD8þ T cells and DC-LAMPþ mature dendritic cells ("immune pattern"), evaluated in paraffin sections, were independent prognostic factors of patients’ survival, and stronger prognosticators than currently evaluated clinical and pathological parameters. Furthermore, tumor immune environment is reproduced throughout cancer disease, from primary tumor to relapsing metastasis. This finding is the first important step for further extensive studies on the role of the tumor cells in shaping their own immune environment and the patients’ outcome. A escape local and systemic immune control (19) and consequently invade and metastasize in distant organs. This hypothesis would predict that the immune microenvironment in metastatic sites should be poor and have no impact on clinical outcome. Only a limited number of studies have reported the presence of immune cells in metastatic lesions. They showed that high densities of CD8þ T cells were associated with longer survival in colorectal carcinoma (20) and ovarian cancer (21), and potential response to chemotherapy in liver metastases from colorectal carcinoma (22). Another question, which remains largely unanswered, concerns the respective roles of the malignant cells and the seeding organ in shaping the immune microenvironment. We therefore analyzed the immune environment of colorectal carcinoma and RCC metastases seeded in a same organ, the lung, compared coincident and relapsing C CD8+ T cells: CD8+ and DC-LAMP+ cells: P = 0.039 1 0.8 Overall survival Overall survival 0.8 0.6 0.4 0.2 B CD8 hi / DC-LAMP hi (n = 67) CD8 lo / DC-LAMP hi or CD8 hi / DC-LAMP lo (n = 53) CD8 lo / DC-LAMP lo (n = 20) 0 20 40 60 80 100 Hi 71 53 40 24 12 4 Lo 69 52 30 15 5 2 Time (months) 0 120 Hi/Hi At risk patients D DC-LAMP+ mature DC: 67 20 40 60 80 100 51 39 24 13 4 MIX 53 42 24 9 3 1 Lo/Lo 20 12 7 6 2 1 120 NKp46+ NK cells: P = 0.001 1 P = 0.12 1 0.8 0.8 Overall survival Overall survival 0.4 CD8 lo (n = 69) Time (months) 0 0.6 0.4 0.2 DC-LAMP Time (months) 0 lo 0.6 0.4 0.2 DC-LAMP hi (n = 116) 0 At risk patients 0.6 0.2 CD8 hi (n = 71) 0 At risk patients P = 0.008 1 NKp46 hi (n = 58) (n = 24) NKp46 lo (n = 26) 0 20 40 60 80 100 Hi 116 91 62 33 16 5 Lo 24 14 8 6 2 1 120 Time (months) 0 At risk patients 20 40 60 80 100 Hi 58 49 39 23 14 5 Lo 26 17 8 3 0 0 120 þ þ þ Figure 1. Prognostic value of the densities of CD8 T cells, DC-LAMP mature dendritic cells, and NKp46 NK cells in lung metastases from colorectal carcinoma. Kaplan–Meier curves for the duration of OS according to a separated (A, B) and combined (C) analysis of CD8þ and DC-LAMPþ densities in colorectal carcinoma lung metastases. D, Kaplan–Meier curves for the duration of OS according to the densities of NKp46þ cells in colorectal carcinoma lung metastases (n ¼ 84). The numbers of at risk patients according to a separated and combined analysis of CD8þ and DC-LAMPþ densities and NKp46þ cells densities were given. Statistical comparison was conducted by the log-rank test and all OS log-rank P values were corrected using the formula proposed by Altman and colleagues. 4080 Clin Cancer Res; 19(15) August 1, 2013 Clinical Cancer Research Downloaded from clincancerres.aacrjournals.org on October 10, 2014. © 2013 American Association for Cancer Research. Published OnlineFirst June 19, 2013; DOI: 10.1158/1078-0432.CCR-12-3847 In Situ Immune Reaction in Lung Metastases E High expression Low expression –2.0 1:1 2.0 Mean(ΔCt) P = 0.014 CD3E CD4 CD8A CD68 Immune cell populations Mean(ΔCt) P = 0.04 IFNG IL12A IL12B 1L18 TBX21 LTA TH1 orientation Mean(ΔCt) P = 0.42 Figure 1. (Continued ) E, expression of genes related to immune cell populations, TH1/TH2 orientations, inflammation, angiogenesis, immuno-suppression, cytotoxicity, chemokines/chemokine receptors according to the densities of CD8þ and DC-LAMPþ cells (high/high vs. low/low) in lung metastases from colorectal carcinoma. Expression levels of genes were determined using threshold cycle (Ct) values normalized to actin B [ACTB] (DCt). We used Mann–Whitney test to identify genes with significantly different levels of expression among patient groups (high vs. low CD8þ/DC-LAMPþ densities). , P < 0.05 for individual gene expression. IL4 IL5 IL10 IL13 TH2 orientation Mean(ΔCt) P = 0.39 C3 FN1 IL3 IL6 IL7 TNF CSF1 IL1A IL8 IL1B IL17 PTGS2 SELE CSF3 STAT3 Inflammation * mean(ΔCt) P = 0.13 ACE CD34 VEGF Angiogenesis mean(ΔCt) P = 0.23 Immunosuppression TGFB1 CTLA4 IL10 * * mean(ΔCt) P = 0.032 GLNY GZMB PRF1 IL15 Cytotoxicity mean(ΔCt) P = 0.03 CCL2 CCL3 CCL5 CCR2 CCR5 Chemokines/ chemokine receptors CCL19 CCR4 CCR7 CXCL10 CXCL11 CXCR3 High CD8+/DC-LAMP+ densities metastases in the lung, and the primary tumor from the same patients, and determined their clinical impacts. We report that tumor cells induce a characteristic and reproducible immune pattern in the primary and metastatic tumors, supporting the hypothesis that the malignant cells, rather than the host organ, shape their microenvironment. We found that a high infiltration by DC-LAMPþ mature dendritic cells and CD8þ T cells is a major predictor of good survival in lung metastases from colorectal carcinoma, whereas it is associated with poor survival in lung metastases from RCC. This shows that the immune microenvironment www.aacrjournals.org Low CD8+/DC-LAMP+ densities pattern remains a major prognostic factor even in advanced cancer stages, but with different consequences depending on the origin of the primary tumor. Altogether our results suggest a strong influence of the tumor origin on the immune environment characteristics and clinical impact. Patients and Methods Patients We constituted a retrospective and unselected cohort of 140 patients with colorectal carcinoma lung metastasis operated at H^ otel-Dieu hospital between 2000 and 2010 Clin Cancer Res; 19(15) August 1, 2013 Downloaded from clincancerres.aacrjournals.org on October 10, 2014. © 2013 American Association for Cancer Research. 4081 Published OnlineFirst June 19, 2013; DOI: 10.1158/1078-0432.CCR-12-3847 Remark et al. Table 1. Univariate and multivariate Cox proportional hazards analyses for OS according to clinical parameters and immune cell densities in colorectal carcinoma and RCC lung metastases Univariate analyses Colorectal carcinoma lung metastases RCC lung metastases Multivariate analyses Variable HR 95% CI P value HR Stage (stage 3 þ 4 vs. stage 1 þ 2) Presence of extrathoracic metastases (yes vs. no) Completeness of resection (R1 vs. R0) CEA level (5 ng/mL vs. <5 ng/mL) NK cells (high vs. low) 1.68 1.56 (0.88–3.20) (0.88–2.75) 0.116 0.128 Not included in the multivariate analysis 2.49 1.55 0.58 (0.77–8.05) (0.86–2.82) (0.28–1.16) 0.129 0.148 0.123 Thoracic lymph node invasion (yes vs. no) Number of metastases (>2 vs. 2) Immune pattern (high/mix/low) 1.49 1.84 0.54 (0.60–3.66) (1.03–3.28) (0.39–0.76) 0.0503 0.0405 0.0002 1.80 2.17 0.54 Initial Fuhrman nuclear grade (3 þ 4 vs. 1 þ 2) Time from lung metastasis diagnosis to surgery (>1 year vs. 1year) Number of metastases (multiple vs. 1) Presence of extrathoracic metastases (yes vs. no) Completeness of resection (R1 vs. R0) Alkaline phosphatase (>80 U/L vs. 80 U/L) Neutrophils (>7,500/mm3 vs. 7,500/mm3) Platelets (>400,000/mm3 vs. 400,000/mm3) 1.32 (0.56–3.11) 0.533 Not included in the multivariate analysis 1.77 (0.83–3.76) 0.142 1.30 1.34 (0.61–2.79) (0.51–3.55) 0.501 0.555 1.40 1.52 0.87 0.80 (0.42–4.65) (0.75–4.33) (0.29–2.62) (0.23–2.82) 0.587 0.682 0.805 0.728 0.35 2.23 (0.16–0.74) (1.02–4.86) 0.0064 0.0435 0.33 1.74 (0.14–0.73) (0.47–6.46) 0.0067 0.407 1.92 2.26 (0.91–4.05) (0.96–5.33) 0.086 0.061 2.41 1.00 (0.81–7.17) (0.34–2.67) 0.113 0.935 0.46 2.68 (0.22–0.95) (1.58–4.57) 0.037 0.00028 0.32 2.70 (0.14–1.03) (1.37–5.29) 0.0579 0.0039 a DFI (1 year vs. <1 year) Metastases at presentation (synchronous vs. metachronous) Thoracic lymph node invasion (yes vs. no) Hemoglobin (men: <13 g/dL vs. 13 g/dL and women: <12 g/dL vs. 12 g/dL) NK cells (high vs. low) Immune pattern (high/mix/low) 95% CI (0.87–3.72) (1.20–3.93) (0.39–0.75) P value 0.115 0.011 0.0003 NOTE: To be able to conduct regression with a categorical variable, they were coded before entered into the Cox model. Parameters with significant impact on survival appear in bold. a The stage was determined by pathologic examination at the time of diagnosis. None of the variables violated the proportional hazards assumption. and 52 patients with RCC lung metastasis, operated at H^ otel-Dieu or Laennec/H^ opital Europeen Georges Pompidou hospitals between 1992 and 2010. In the RCC series, 51 of 52 patients were treated with radical nephrectomy and 1 with partial nephrectomy. None of the patients had signs of local recurrence of primary tumor. We also analyzed 25 colorectal carcinoma and 24 RCC primary tumors from the same patients, operated at Saint-Antoine, Cochin, or Necker-Enfants Malades hospitals between 1987 and 2008. In addition, 14 coincident and 12 recurrent colorectal carcinoma lung metastases from the same patients were studied. Altogether, 218 lung metastases from 192 patients were analyzed. Among these 192 patients, 32 frozen samples of lung metastases were available for patients with colorectal carcinoma (n ¼ 19) or RCC (n ¼ 13). 4082 Clin Cancer Res; 19(15) August 1, 2013 Baseline characteristics of these patients are summarized in Supplementary Tables S1 and S2. All experiments were conducted with the agreement of the Ile de France II ethics committee (no. 2012-0612). Immunohistochemistry For each tumor, 2 observers (R. Remark and D. Damotte, A. Lupo, A. Cazes, L. Gibault, or V. Verkarre, expert pathologists) selected the tumor section containing the highest density of immune cells on hematoxylin and eosin stained slides. Serial 5-mm formalin-fixed and paraffin-embedded tissue sections were stained with autostainer Link 48 (Dako). Tissue sections were incubated with primary antibodies [CD3 polyclonal antibody (Dako), CD8 (SP16, Springbioscience), CD20 (L26, Dako), DC-LAMP (1010.01, Dendritics), granzyme B (11F1, Novocastra), NKp46 (195314, Clinical Cancer Research Downloaded from clincancerres.aacrjournals.org on October 10, 2014. © 2013 American Association for Cancer Research. Published OnlineFirst June 19, 2013; DOI: 10.1158/1078-0432.CCR-12-3847 In Situ Immune Reaction in Lung Metastases A Coincident metastases: Relapsing metastases: t = 1–9 months C R = 0.643 ns Number of DC-LAMP+ cells/mm2 3,000 2,000 1,000 0 rs Fi E d on sid tm 0 s ap a et is re Lung metastasis R = 0.895 ns rs Fi d on sid tm F a et is re 100 G * R = 0.659 ns 15 8,000 6,000 4,000 2,000 0 10 5 C d on sid c Se M -L C CR tm ps la a et is re as st rs Fi e is as st a et M H R = 0.656 ns 800 600 400 200 0 0 T -P CR e e id ts M R = 0.693 10,000 200 rs Fi as st rs Fi s ap l s a et c Se s ta 300 0 e is e e id ts M Primary tumor versus metastases: Primary tumor 5 as st rs Fi 10 l s a et c Se s ta R = 0.696 ns 400 15 e is e e id ts D R = 0.580 ns Number of DC-LAMP+ cells/mm2 Number of CD8+ cells/mm2 4,000 R = 0.614 ns Metastasis relapse Number of NKp46+ cells/mm2 R = 0.644 ns Number of CD8+ cells/mm2 B First metastasis Second side Number of NKp46+ cells/mm2 First side t = 14–52 months T -P C CR M -L C CR PT C- CR LM C- CR þ þ þ Figure 2. CD8 T cells, DC-LAMP mature dendritic cells, and NKp46 NK cell densities in coincident or relapsing metastases and in primary colorectal cancer. A, surgical treatment for coincident and relapsing colorectal carcinoma lung metastases. B–D, coincident or relapsing metastases have the same densities of CD8þ, DC-LAMPþ, and NKp46þ cells. E, surgical treatment for primary colorectal carcinoma and their lung metastases. F–H, colorectal carcinoma primary tumors were more infiltrated by CD8þ cells than lung metastases, but have similar densities of DC-LAMPþ and NKp46þ cells. R values show the positive correlations (0.5 < R < 0.9 and P < 0.05, Spearman test) between coincident metastases, relapsing metastases, primary tumors, and associated metastases according to the CD8þ, DC-LAMPþ, and NKp46þ cell densities. PT, primary tumor; LM, lung metastasis; ns, not significant; , P < 0.05 (Wilcoxon matched pairs test). R&D Systems), or PNAd (MECA-79, BD Pharmingen)] followed by secondary antibodies coupled with biotin or alkaline phosphatase. Biotinylated antibodies were coupled with streptavidin-peroxidase and peroxidase activity www.aacrjournals.org was revealed using 3-amino-9-ethylcarbazole substrate (Vector Laboratories). Alkaline phosphatase activity was revealed using alkaline phosphatase substrate III (Vector Laboratories). Clin Cancer Res; 19(15) August 1, 2013 Downloaded from clincancerres.aacrjournals.org on October 10, 2014. © 2013 American Association for Cancer Research. 4083 Published OnlineFirst June 19, 2013; DOI: 10.1158/1078-0432.CCR-12-3847 Remark et al. A C CD8+ T cells: CD8+ and DC-LAMP+ cells: P = 0.03 1 0.8 Overall survival 0.8 Overall survival P < 0.0001 1 0.6 0.4 0.6 0.4 CD8 lo / DC-LAMP lo (n = 25) CD8 lo / DC-LAMP hi or CD8 hi / DC-LAMP lo (n = 18) CD8 hi / DC-LAMP hi (n = 9) 0.2 0.2 CD8 lo (n = 36) CD8 hi (n = 16) 0 Time (months) 0 At risk patients B 0 20 40 60 80 100 Hi 16 7 4 2 0 0 Lo 36 27 16 11 6 4 Time (months) 0 120 Hi/Hi At risk patients D DC-LAMP+ mature DC: 60 80 100 0 0 0 0 18 13 7 5 2 1 25 19 13 8 5 4 120 NKp46+ NK cells: P = 0.002 1 0.8 Overall survival Overall survival 40 2 Lo/Lo 0.8 0.6 0.4 0.2 0.6 0.4 0.2 DC-LAMP lo (n = 32) NKp46 hi (n = 28) DC-LAMP hi (n = 20) 0 Time (months) 0 At risk patients 20 MIX P = 0.03 1 9 NKp46 lo (n =24) 0 20 40 60 80 100 Hi 20 10 5 3 1 0 Lo 32 24 16 10 6 5 120 Time (months) 0 At risk patients 60 80 100 Hi 28 20 20 40 13 9 5 3 Lo 24 12 7 4 2 2 120 þ þ þ Figure 3. Prognostic value of the densities of CD8 T cells, mature dendritic cells (DC-LAMP ), and NK cells (NKp46 ) in lung metastases from RCC. Kaplan–Meier curves for the duration of OS according to a separated (A, B) and combined (C) analysis of CD8þ and DC-LAMPþ cell densities. D, Kaplan–Meier curves for the duration of OS according to the densities of NKp46þ cells. The numbers of at risk patients according to a separated and combined analysis of CD8þ and DC-LAMPþ densities and NKp46þ cells densities were given. Statistical comparison was conducted by the log-rank test and all OS log-rank P values were corrected using the formula proposed by Altman and colleagues. The density of DC-LAMPþ cells was manually counted on the entire section as previously described (23). CD3þ, CD8þ, granzyme Bþ, and NKp46þ cells were counted in the center of the tumor and in the invasive margin of the tumor with the convergence to the mean method (24). For each slide, 40 to 100 high-power fields (1.37–3.43 mm2) were examined on each tumor zone. Both immunostaining and scoring were evaluated by 3 independent observers blinded to clinical data (R. Remark, L. Crozet, and A. Lupo, expert pathologist). Gene expression analyses RNA from the frozen tissues of 32 lung metastases was extracted with the RNeasy Mini Kit (Qiagen) according to the manufacturer’s instructions and controlled for quantity and quality on an Agilent 2100 Bioanalyser (Agilent Technologies). Then, reverse transcription PCR was conducted with the High-Capacity cDNA Reverse 4084 Clin Cancer Res; 19(15) August 1, 2013 Transcription kit (Applied Biosystem). Finally, the quantitative gene expression analysis of selected targets was conducted in duplicates with the TaqMan Human Immune Array on an Applied Biosystems 7900HT Fast Real-Time PCR System. Expression levels of genes were determined using threshold cycle (Ct) values normalized to actin B (DCt) and were represented using the Genesis program. Statistical analyses We used the Mann–Whitney test to compare the densities of infiltrating immune cells in the different tumors and DCt, and the Wilcoxon matched pairs test to compare the density of infiltrating immune cells in different tumors from the same patient. Because all gene expression comparisons were preplanned and the 51 genes clustered according to their immune functions before analysis, the P values were not corrected by Bonferroni Clinical Cancer Research Downloaded from clincancerres.aacrjournals.org on October 10, 2014. © 2013 American Association for Cancer Research. Published OnlineFirst June 19, 2013; DOI: 10.1158/1078-0432.CCR-12-3847 In Situ Immune Reaction in Lung Metastases E High expression –2.0 1:1 2.0 Low expression Mean(ΔCt) P = 0.0046 CD3E CD4 CD8A CD68 Immune cell populations Mean(ΔCt) P = 0.0094 IFNG IL12A IL12B 1L18 TBX21 LTA TH1 orientation Mean(ΔCt) P = 0.36 IL4 IL5 IL10 IL13 TH2 orientation Mean(ΔCt) P = 0.16 C3 FN1 IL3 IL6 IL7 TNF CSF1 IL1A IL8 IL1B IL17 PTGS2 SELE CSF3 STAT3 Inflammation Mean(ΔCt) P = 0.130 ACE CD34 VEGF Angiogenesis Mean(ΔCt) P = 0.165 Immunosuppression * * * TGFB1 CTLA4 IL10 Mean(ΔCt) P = 0.126 GLNY GZMB PRF1 IL15 Cytotoxicity Mean(ΔCt) P = 0.018 CCL2 CCL3 CCL5 CCR2 CCR5 Chemokines/ chemokine receptors CCL19 CCR4 CCR7 CXCL10 CXCL11 CXCR3 High CD8+/ DC-LAMP+ densities Low CD8+/ DC-LAMP+ densities Figure 3. (Continued ) E, expression of genes related to immune cell populations, TH1/TH2 orientations, inflammation, angiogenesis, immuno-suppression, cytotoxicity, chemokines/chemokine receptors according to the CD8þ and DC-LAMPþ cell densities (high/high vs. low/low) in lung metastases from RCC. Expression levels of genes were determined using threshold cycle (Ct) values normalized to actin B [ACTB] (DCt). We used Mann–Whitney test to identify genes with significantly different levels of expression among patient groups (high vs. low). , P < 0.05 for individual gene expression. or similar methods. Correlations were evaluated by the Spearman test. Overall survival (OS) curves were estimated by Kaplan–Meier method and differences between the groups of patients were calculated using the log-rank test. The start of follow-up for OS was the time of lung surgery. In addition to mature dendritic cells, CD8þ T cells, and NK cells densities, the following available clinical parameters were tested: initial stage (colorectal carcinoma), completeness of resection at pulmonary level, number of lung metastases, presence of extrathoracic metastases at www.aacrjournals.org time of lung surgery, thoracic lymph node invasion, carcinoembryonic antigen (CEA) level (colorectal carcinoma), initial Fuhrman nuclear grade (RCC), presence of metastases at presentation (RCC), time from lung metastasis diagnosis to surgery (RCC), disease-free interval (RCC), alkaline phosphatase, hemoglobin, neutrophils, and platelets levels (RCC). The lower limit of normal was used for hemoglobin (cutoff values: men ¼ 13 g/dL and women ¼ 12 g/dL) and the upper limit (ULN) was used for alkaline phosphatase (cutoff value: 80 U/L), neutrophils (cutoff value: 7500/mm3), and platelets (cutoff value: 400,000/mm3). With respect to immune cell densities and number of metastases, the "minimum P value" approach was used to determine the cutoff for the best separation of patients referring to their OS outcome (outcome-oriented approach). Because the P values obtained might be overestimated, OS log-rank P values were corrected using the formula proposed by Altman and colleagues (25) and using 10-fold crossvalidations as recommended by Faraggi and colleagues (26). The confidence interval was important around the optimal P value (Supplementary Table S3). We have also ensured that the significance established at the optimal cutoff remained valid at the quartiles (dataoriented approach). A P value less than 0.05 was considered statistically significant. Independent parameters identified at univariate analysis as possibly influencing outcome (P < 0.1) were introduced in a multivariate Coxproportional hazards regression model. All analyses were conducted with Prism 5 (GraphPad), Statview (Abacus Systems), and the R (http://www.r-project.org/). Results The densities of immune cells correlate with OS in lung metastases from colorectal carcinoma Because densities of CD8þ T cells and DC-LAMPþ mature dendritic cells in primary tumors correlate with survival (1), we counted these cells in lung metastases from 140 colorectal carcinoma patients. We also quantified NKp46þ NK cells as a marker of innate immune response. High densities of infiltrating CD8þ T cells (Fig. 1A) and mature dendritic cells (Fig. 1B) were associated with prolonged OS (P ¼ 0.039 and 0.001, respectively). Combination of these 2 immune parameters allowed to identify patients with better outcome (CD8high/DC-LAMPhigh; Fig. 1C, P ¼ 0.008). NKp46þ cell density did not predict clinical outcome (P ¼ 0.12; Fig. 1d). Significance was established at the optimal cutoff, but remained valid at quartiles including the median (Supplementary Table S3). The quantification of CD8þ T cells separately in the center of the tumor and the invasive margin regions yielded similar results (Supplementary Fig. S1). Univariate analysis of other clinical and pathological parameters is reported in Table 1. At multivariate analysis (Table 1), immune pattern (CD8þ/DC-LAMPþ densities) of metastases was the strongest independent predictor of survival. As reported in colorectal carcinoma primary tumors (3), gene expression analyses revealed that a strong CD8þ and DC-LAMPþ cell infiltration was associated with a higher Clin Cancer Res; 19(15) August 1, 2013 Downloaded from clincancerres.aacrjournals.org on October 10, 2014. © 2013 American Association for Cancer Research. 4085 Published OnlineFirst June 19, 2013; DOI: 10.1158/1078-0432.CCR-12-3847 Remark et al. expression of genes linked to TH1 orientation, cytotoxicity, and lymphoid chemokines/chemokine receptors in lung metastases (Fig. 1e). Expressions of clusters of genes associated with TH2 orientation, inflammation, angiogenesis, or immunosuppression were not correlated with the CD8þ/ DC-LAMPþ densities. However, individual gene expression of VEGF was inversely correlated with CD8þ/DC-LAMPþ infiltration, as reported in primary colorectal carcinoma (3, 27) whereas that of IL17 and CTLA4 were positively correlated (Fig. 1e). The in situ immune pattern is reproduced from primary tumors to metastases in colorectal carcinoma To investigate whether the in situ immune pattern varies during the course of the metastatic disease for a given patient, we analyzed coincident colorectal carcinoma lung metastases occurring in the other lung side (n ¼ 14) operated 1 to 9 months after the initial metastatic surgery, and/or relapsing metastasis occurring 14 to 52 months after surgical removal of the lung metastasis (n ¼ 12; Fig. 2A). Densities of CD8þ (Fig. 2B), DC-LAMPþ (Fig. 2C), and NKp46þ (Fig. 2D) cells were not significantly different between 2 coincident metastatic sites or between the first lung metastasis and its relapse. We found correlations in the densities of immune cells between coincident and relapsing metastases (Fig. 2B–D). To address the question of the relationship between immune cell densities in the primary tumor and metastasis, we compared immune infiltrates of primary tumors and lung metastases from the same individuals (n ¼ 25; Fig. 2E). Primary colorectal carcinoma differed from lung metastases by significantly higher density of CD8þ T cells (P < 0.05; Fig. 2F), but the density of each cell type was positively correlated between the primary and the metastatic tumors (Fig. 2F–H for CD8þ, DC-LAMPþ, and NKp46þ cells, respectively). We had access to a small number (n ¼ 5) of matched hepatic metastases and the correlation was also found between primary colorectal carcinoma, lung, and liver metastases (data not shown). The densities of immune cells correlate with OS in lung metastases from RCC We have also analyzed a cohort of 52 RCC lung metastases. Patients with high densities of infiltrating CD8þ T cells (Fig. 3A) or DC-LAMPþ cells (Fig. 3B) have reduced survival (P ¼ 0.03). These 2 immune parameters allowed to identify, with strong significance, patients with poorer outcome (CD8high/DC-LAMPhigh; Fig. 3C, P < 0.0001). High density of NKp46þ cells was associated with improved survival (P ¼ 0.002; Fig. 3D). Separate analysis of the CD8þ and NKp46þ immune infiltrates in the center of the tumor and invasive margin also correlated with OS (Supplementary Fig. S2). Significance was established at the optimal cutoff but also conserved at the quartiles (Supplementary Table S3). Univariate proportional hazard Cox analyses revealed that the immune pattern (CD8þ/DC-LAMPþ densities), NKp46þ cell density, presence of metastases at presentation, and diseasefree interval were the only prognostic factors of patients’ 4086 Clin Cancer Res; 19(15) August 1, 2013 survival in our cohort (Table 1). Our data also suggest that hemoglobin and thoracic lymph node invasion tended to be associated with survival (P ¼ 0.061 and 0.086, respectively). In the resulting multivariate proportional hazard Cox model, DFI and immune pattern were independent prognostic factors (P ¼ 0.0067 and 0.0039, respectively; Table 1). A strong CD8þ/DC-LAMPþ infiltration was associated with a higher expression of genes linked to TH1 orientation, lymphoid, and myeloid chemokine/chemokine receptors. Contrasting with colorectal carcinoma, cytotoxicity-related genes were highly expressed in both groups of tumors (refs. 3, 27; Fig. 3E) and, interestingly, VEGF gene expression was positively correlated with CD8þ/DC-LAMPþ infiltration, as well as that of interleukin-6 and STAT3. As previously shown in colorectal carcinoma, we found a correlation between the density of infiltrating DC-LAMPþ, CD8þ, and NKp46þ cells in the primary tumor and in the corresponding lung metastasis (n ¼ 24; Fig. 4A–D), indicating that the in situ immune pattern of the primary tumor was reproduced in the metastasis. The cell composition, organization, and polarization of the immune reaction is different in colorectal carcinoma and RCC lung metastases Because CD8þ, DC-LAMPþ, and NKp46þ cell densities in lung metastases have different clinical impacts in colorectal carcinoma and RCC, we compared their microenvironments. Histologic analyses revealed profound differences between colorectal carcinoma and RCC lung metastases. We found glands, often necrotic, in an abundant and collagenous stroma surrounded by a high density of tertiary lymphoid structures (TLS) in colorectal carcinoma metastases (Fig. 5A). In contrast, in RCC metastases, tumor cell nests were separated by a thin stroma with few and scattered TLS (Fig. 5A). TLS contained a B-cell follicle, a T-cell zone, and PNAdþ high-endothelial venules (Fig. 5B). We found similar densities of CD3þ and CD8þ T cells in the whole tumor zone (Fig. 5C). Mature dendritic cells, located in the T-cell area of TLS, were found at higher density in colorectal carcinoma than in RCC (P < 0.0001; Fig. 5B and C), in accordance with the higher number of TLS in colorectal carcinoma lung metastases. The colorectal carcinoma metastases contained significantly lower densities of NK cells as compared to RCC metastases (P < 0.0001; Fig. 5B and C). No significant differences in the densities of CD8þ, DC-LAMPþ, and NKp46þ cells were observed in tumors from colorectal carcinoma or RCC patients having received or not preoperative treatment (chemotherapy, IL-2/IFN, or association of bevacizumab and chemotherapy; Fig. S3 and Supplementary Tables S1 and S2 for treatment details). Although expression of genes linked to adaptive immune populations was not significantly different between both types of metastatic tumors, we found a lower expression of CD68 gene in colorectal carcinoma lung metastases (Fig. 5D and Supplementary Fig. S4 for detailed gene level expression). A similar TH1 orientation was found in colorectal carcinoma and RCC metastases, but a stronger expression of genes linked to TH2 was detected in RCC Clinical Cancer Research Downloaded from clincancerres.aacrjournals.org on October 10, 2014. © 2013 American Association for Cancer Research. Published OnlineFirst June 19, 2013; DOI: 10.1158/1078-0432.CCR-12-3847 In Situ Immune Reaction in Lung Metastases Primary tumor versus lung metastasis: A C R = 0.689 ns 8,000 6,000 4,000 2,000 D R = 0.547 * 15 Number of DC-LAMP+ cells/mm2 10,000 10 5 RC T M L C- RC lung metastases. Genes linked to acute inflammation were upregulated in colorectal carcinoma lung metastases and genes linked to chronic inflammation, angiogenesis, or immunosuppression were upregulated in RCC lung metastases. A higher expression of cytotoxicity-related genes in RCC metastases was observed, in accordance with their higher NK-cell content. Chemokines and receptors genes prone to attract TH1, T regulatory, and dendritic cells were more expressed in colorectal carcinoma metastases, whereas RCC lung metastases were characterized by the expression of inflammatory chemokines and chemokine receptors genes. Discussion The objective of our study was to characterize the immune microenvironment of metastatic lesions and its clinical impact. If several clinical parameters have been reported to be associated with survival in metastatic patients, none has obtained general agreement (17, 28), justifying the search of new nonclinical prognostic markers. We report here a major prognostic value of the immune pattern (densities of mature dendritic cells and CD8þ T cells) in metastases from colorectal carcinoma and RCC, although with opposite impact on OS. In our cohorts of oligometastatic surgically treated 600 400 200 0 0 T P C- R = 0.817 ns 800 Number of NKp46+ cells/mm2 B 0 www.aacrjournals.org Lung metastasis Primary tumor Number of CD8+ cells/mm2 þ þ Figure 4. CD8 T cells, DC-LAMP mature dendritic cells, and NKp46þ NK cell densities in metastases and in primary RCC tumors. A, surgical treatment for primary RCC and their lung metastases. B–D, RCC primary tumors were less infiltrated by DC-LAMPþ cells than lung metastases. R values show the positive correlations (0.5 < R < 0.9 and P < 0.05, Spearman test) between primary tumors and lung metastases according to the CD8þ, DC-LAMPþ, and NKp46þ cell densities. PT, primary tumor; LM, lung metastasis; ns, not significant; , P < 0.05 (Wilcoxon matched pairs test). P C- RC PT M RC L C- C- RC M -L C RC patients, the strongest prognosticator was the immune pattern, that is CD8þ and DC-LAMPþ cell density combination, as reported for many primary tumors (1–13, 23, 27, 29–31). NK cells density had also a prognostic value in RCC. It seems that the immune pattern is a powerful prognostic factor and a potentially important parameter for metastatic patients’ management. Because of the incomplete data collection (especially for laboratory values which were difficult to collect in a retrospective analysis), conclusions remain difficult to draw on the prognostic value of the Memorial Sloan-Kettering Cancer Center (32) and Heng and colleagues (33) prognostic factor models. Our previous studies showed the highly clinical impact of the CD8þ cell densities in primary colorectal carcinoma up to stage III, that is without distant metastases at the time of diagnosis (2). In this study, the impact of the immune pattern on OS was lower in primary tumors (P ¼ 0.15 and 0.01 for CD8þ and DC-LAMPþ cells, respectively; data not shown) than in lung metastases from colorectal carcinoma (P ¼ 0.039 and 0.001 for CD8þ and DC-LAMPþ cells, respectively; data not shown). Clinical significance of CD8þ T cells density seems to be contrasted, according to primary tumor’s origin. Although we found similar densities of CD8þ T cells in both colorectal carcinoma and RCC metastases, the prognostic value of Clin Cancer Res; 19(15) August 1, 2013 Downloaded from clincancerres.aacrjournals.org on October 10, 2014. © 2013 American Association for Cancer Research. 4087 Published OnlineFirst June 19, 2013; DOI: 10.1158/1078-0432.CCR-12-3847 Remark et al. A B Colorectal cancer Lung metastasis Renal cell carcinoma Lung metastasis Colorectal cancer Lung metastasis Renal cell carcinoma Lung metastasis Figure 5. Comparison of the immune contextures in colorectal carcinoma and RCC lung metastases. A, representative pictures of colorectal carcinoma and RCC lung metastases [hematoxylin–eosin–safran (HES) 4088 Clin Cancer Res; 19(15) August 1, 2013 these cells was different. Similar conflicting observations about the prognostic role of immune infiltrate have been reported in primary colorectal carcinoma and RCC (2, 4, 15, 27) and one could hypothesize that the seeding organ (colon or kidney) may explain this variability in the outcome. Because it remains valid in the lung metastases, our data support the idea that the kind of primary tumor is essential in determining the prognostic value of the host immune infiltrate at metastatic level. This is in accordance with the fact that primary RCC seems as an exception to the well-documented general findings that TH1/CD8 immune cell infiltrate and high density of mature dendritic cells correlate with favorable prognosis in the majority of solid tumors (1). The differential clinical impacts of the T cells might be due to their site of activation. Indeed, we have previously reported that TLS in early stages of non–small cell lung cancer may act as potential structures of antitumor T-cell generation (23, 34). We found more TLS, reflected by higher densities of mature dendritic cells and higher expression of CCL19 gene, a chemokine expressed in TLS (34), in colorectal carcinoma than in RCC metastases. Because TLS are scarce in RCC lung metastases and numerous in lung metastases from colorectal carcinoma, one may postulate that the T cells present in the former have not been educated in tumor-adjacent TLS (35) and reflect rather a chronic inflammatory reaction which is known to be deleterious for the host (36). Indeed, gene expression analyses revealed significant differences between lung metastases from colorectal carcinoma and RCC, which share a TH1 profile, but the latter exhibit also a TH2, inflammatory, and immunosuppressive pattern. The high expression of VEGF, IL-6, and M-CSF genes in RCC may also inhibit the differentiation of dendritic cells and induce monocyte differentiation to macrophages (37–39), which could initiate an impaired T-cell response in RCC, resulting in poor prognosis. Interestingly, VEGF gene expression was positively correlated with high CD8þ and DC-LAMPþ infiltration in RCC lung metastases and with low CD8þ and DC-LAMPþ infiltration in colorectal carcinoma lung metastases. Because it has been suggested that VEGF may induce non-coordinated immune responses (27), affect cytotoxic TH1 adaptive immune responses (39, 40) and contribute to the progression of malignant disease, the correlation between CD8þ/DC-LAMPþ densities and VEGF expression could be one explanation among others to explain the negative impact associated with this immune signature. Moreover, upregulation of IL6 and STAT3 genes in the CD8high/DCLAMPhigh group could reflect the inflammatory milieu of the RCC microenvironment (41, 42). It could also explain the reasons that immunotherapies, which modify the staining] showing the organization of tumors. Original magnification: 40 and 200. TLS, tertiary lymphoid structure; T, tumor; S, stroma. B, þ location and organization of CD20 B-cell follicles (red) surrounded by high-endothelial venules (blue), DC-LAMP expressing mature dendritic cells (red, black arrows), CD3þ T cells (red), CD8þ T cells (red), and NKp46þ NK cells (red) in colorectal carcinoma (left) and RCC (right) lung metastases. Original magnification: 200 and 400. Clinical Cancer Research Downloaded from clincancerres.aacrjournals.org on October 10, 2014. © 2013 American Association for Cancer Research. Published OnlineFirst June 19, 2013; DOI: 10.1158/1078-0432.CCR-12-3847 In Situ Immune Reaction in Lung Metastases C CD8+ T cells: CD3+ T cells: ns 10,000 D –2.0 High expression ns 10,000 1:1 2.0 Low expression Number of CD8+ cells/mm2 Number of CD3+ cells/mm2 CD68 1,000 CD3E CD4 CD8A Th1 orientation 100 Th2 orientation LM LM C- C- DC-LAMP+ mature *** CR M M L C- L C- RC ns IL18 TBX21 IFNG IL12A IL12B LTA ns IL5 IL4 * IL10 IL13 ns FN1 C3 VEGF STAT3 CSF1 ACE CD34 IL6 IL7 TNF IL3 * IL8 IL1A *** 1,000 Number of NKp46+ cells/mm2 0.01 Inflammation and angiogenesis NKp46+ NK cells: 10 0.1 C- RC CR 1 LM LM C- RC CR * 1,000 10 100 Number of DC-LAMP+ cells/mm2 Immune cell populations Immunosuppression * IL1B PTGS2 SELE CSF3 IL17 ns TGFB1 CSF1 * CTLA4 IL10 ns GZMB GLNY PRF1 IL15 * 100 Cytotoxicity CCR2 CCL2 CCR5 CCL3 CCL5 10 Chemokines/ chemokines receptors 1 M M CR L C- L C- RC Colorectal carcinoma - LM * CCR4 CCL19 CXCL11 * CXCR3 CXCL10 CCR7 ns Renal cell carcinoma - LM þ þ þ þ Figure 5. (Continued ) C, quantification of CD3 , CD8 , DC-LAMP , and NKp46 cells in lung metastases from colorectal (colorectal carcinoma-LM, n ¼ 140) and renal cell carcinoma (RCC-LM, n ¼ 52). Whiskers length represents 10 to 90 percentile. ns, not significant; , P < 0.0001 (Mann–Whitney test). D, heat map of the expression levels of genes according to the origin of lung metastases (colorectal carcinoma and RCC) represented using the Genesis program. LM, lung metastasis; ns, not significant; , P < 0.05 (Mann–Whitney test). acute/chronic inflammatory microenvironment, are often reported to have some efficacy in metastatic renal cell carcinoma (43). The Von Hippel Lindau phenotype, often found in RCC, may also be involved in the shaping of peculiar tumor microenvironments, through induction of hypoxia, production of VEGF, induction of regulatory immune circuits (44–47), and increased sensitivity of tumor cells to NK-cell lysis (48). It may also influence differently the stroma characteristics, the vascularization, or the collagen content which could also impact on the migration, organization, and functionality of intratumor immune cells (49). Together, these data may explain the negative clinical impact of the adaptive immune pattern at the primary and advanced stages of RCC. www.aacrjournals.org We found that colorectal carcinoma and RCC have a correlated pattern of DC-LAMPþ, CD8þ, and NKp46þ cells, from primary tumor to relapsing metastasis, which could reflect, either a potential "imprinting" of the immune microenvironment by the tumor cells or the possibility that the immune contexture in the primary tumor, results in "educated" immune cells that are recalled in the metastatic sites. In conclusion, our findings highlight the fact that during all steps of cancer development, reciprocal interactions occur between immune and cancer cell and are critical for patients’ survival. The immune signature seems to be a phenotypic marker for the disease and is remarkably reproduced between primary and metastatic sites in the same patient. The immune contexture affects OS in lung metastases from colorectal Clin Cancer Res; 19(15) August 1, 2013 Downloaded from clincancerres.aacrjournals.org on October 10, 2014. © 2013 American Association for Cancer Research. 4089 Published OnlineFirst June 19, 2013; DOI: 10.1158/1078-0432.CCR-12-3847 Remark et al. carcinoma and RCC, and the analysis of the immune pattern might be useful to guide therapeutics (50). Disclosure of Potential Conflicts of Interest S. Oudard has honoraria from speakers bureau of Sanofi, Roche, Novartis, BMS, Takeda, and Jansen. No potential conflicts of interest were disclosed by the other authors. Authors' Contributions Conception and design: R. Remark, J.-F. Regnard, C. Sautes-Fridman, W.H. Fridman, D. Damotte Development of methodology: R. Remark, M.-C. Dieu-Nosjean, D. Damotte Acquisition of data (provided animals, acquired and managed patients, provided facilities, etc.): R. Remark, M. Alifano, A. Lupo, M. Riquet, H. Ouakrim, J. Goc, A. Cazes, J.F. Flejou, L. Gibault, J.-F. Regnard, O.N. Pages, S. Oudard, D. Damotte Analysis and interpretation of data (e.g., statistical analysis, biostatistics, computational analysis): R. Remark, M. Alifano, I. Cremer, M.-C. Dieu-Nosjean, S. Oudard, W.H. Fridman, D. Damotte Writing, review, and/or revision of the manuscript: R. Remark, M. Alifano, I. Cremer, M.-C. Dieu-Nosjean, J. Goc, S. Oudard, C. Sautes-Fridman, W.H. Fridman, D. Damotte Administrative, technical, or material support (i.e., reporting or organizing data, constructing databases): R. Remark, L. Crozet, A. Cazes, L. Gibault, V. Verkarre, B. Mlecnik, C. Sautes-Fridman, W.H. Fridman, D. Damotte Study supervision: W.H. Fridman, D. Damotte Acknowledgments The authors thank P. Bonjour, V. Ducruit, T. Fredriksen for technical assistance and M. Bovet for help in clinical data collection, the H^ otel-Dieu hospital tumor bank (no. DC 2009-947), the tumorotheque cancer-est (Tumo0203), and the "Centre d’Imagerie Cellulaire et de Cytometrie" (Cordeliers Research Center, Paris). Grant Support This work was supported by Institut National de la Sante et de la Recherche Medicale (INSERM), Universite Paris-Descartes, Universite Pierre et Marie Curie, Institut National du Cancer, Canceropole Ile de France, and Labex Immuno-oncology (2011-1-PLBIO-06-INSERM 6-1, PLBIO09-088IDF-KROEMER, 11LAXE62_9UMS872 FRIDMAN). The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked advertisement in accordance with 18 U.S.C. Section 1734 solely to indicate this fact. Received December 21, 2012; revised May 23, 2013; accepted June 7, 2013; published OnlineFirst June 19, 2013. References 1. Fridman WH, Pages F, Sautes-Fridman C, Galon J. The immune contexture in human tumours: impact on clinical outcome. Nat Rev Cancer 2012;12:298–306. 2. Galon J, Costes A, Sanchez-Cabo F, Kirilovsky A, Mlecnik B, LagorcePages C, et al. Type, density, and location of immune cells within human colorectal tumors predict clinical outcome. Science 2006;313:1960–4. 3. Pages F, Kirilovsky A, Mlecnik B, Asslaber M, Tosolini M, Bindea G, et al. In situ cytotoxic and memory T cells predict outcome in patients with early-stage colorectal cancer. J Clin Oncol 2009;27:5944–51. 4. Naito Y, Saito K, Shiiba K, Ohuchi A, Saigenji K, Nagura H, et al. CD8þ T cells infiltrated within cancer cell nests as a prognostic factor in human colorectal cancer. Cancer Res 1998;58:3491–4. 5. Al-Shibli KI, Donnem T, Al-Saad S, Persson M, Bremnes RM, Busund LT. Prognostic effect of epithelial and stromal lymphocyte infiltration in non-small cell lung cancer. Clin Cancer Res 2008;14:5220–7. 6. Mahmoud SM, Paish EC, Powe DG, Macmillan RD, Grainge MJ, Lee AH, et al. Tumor-infiltrating CD8þ lymphocytes predict clinical outcome in breast cancer. J Clin Oncol 2011;29:1949–55. 7. Ubukata H, Motohashi G, Tabuchi T, Nagata H, Konishi S. Evaluations of interferon-gamma/interleukin-4 ratio and neutrophil/lymphocyte ratio as prognostic indicators in gastric cancer patients. J Surg Oncol 2010;102:742–7. 8. Fukunaga A, Miyamoto M, Cho Y, Murakami S, Kawarada Y, Oshikiri T, et al. CD8þ tumor-infiltrating lymphocytes together with CD4þ tumorinfiltrating lymphocytes and dendritic cells improve the prognosis of patients with pancreatic adenocarcinoma. Pancreas 2004;28:e26–31. 9. Sharma P, Shen Y, Wen S, Yamada S, Jungbluth AA, Gnjatic S, et al. CD8 tumor-infiltrating lymphocytes are predictive of survival in muscle-invasive urothelial carcinoma. Proc Natl Acad Sci U S A 2007;104: 3967–72. 10. Gao Q, Qiu SJ, Fan J, Zhou J, Wang XY, Xiao YS, et al. Intratumoral balance of regulatory and cytotoxic T cells is associated with prognosis of hepatocellular carcinoma after resection. J Clin Oncol 2007; 25:2586–93. 11. Schumacher K, Haensch W, Roefzaad C, Schlag PM. Prognostic significance of activated CD8(þ) T cell infiltrations within esophageal carcinomas. Cancer Res 2001;61:3932–6. 12. Zhang L, Conejo-Garcia JR, Katsaros D, Gimotty PA, Massobrio M, Regnani G, et al. Intratumoral T cells, recurrence, and survival in epithelial ovarian cancer. N Engl J Med 2003;348:203–13. 4090 Clin Cancer Res; 19(15) August 1, 2013 13. Clemente CG, Mihm MC Jr, Bufalino R, Zurrida S, Collini P, Cascinelli N. Prognostic value of tumor infiltrating lymphocytes in the vertical growth phase of primary cutaneous melanoma. Cancer 1996;77:1303–10. 14. Hotta K, Sho M, Fujimoto K, Shimada K, Yamato I, Anai S, et al. Prognostic significance of CD45ROþ memory T cells in renal cell carcinoma. Br J Cancer 2011;105:1191–6. 15. Nakano O, Sato M, Naito Y, Suzuki K, Orikasa S, Aizawa M, et al. Proliferative activity of intratumoral CD8(þ) T-lymphocytes as a prognostic factor in human renal cell carcinoma: clinicopathologic demonstration of antitumor immunity. Cancer Res 2001;61:5132–6. 16. Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin 2011;61:69–90. 17. Riquet M, Foucault C, Cazes A, Mitry E, Dujon A, Le Pimpec Barthes F, et al. Pulmonary resection for metastases of colorectal adenocarcinoma. Ann Thorac Surg 2010;89:375–80. 18. Campbell PJ, Yachida S, Mudie LJ, Stephens PJ, Pleasance ED, Stebbings LA, et al. The patterns and dynamics of genomic instability in metastatic pancreatic cancer. Nature 2010;467:1109–13. 19. Dunn GP, Old LJ, Schreiber RD. The three Es of cancer immunoediting. Annu Rev Immunol 2004;22:329–60. 20. Katz SC, Pillarisetty V, Bamboat ZM, Shia J, Hedvat C, Gonen M, et al. T cell infiltrate predicts long-term survival following resection of colorectal cancer liver metastases. Ann Surg Oncol 2009;16:2524–30. 21. Leffers N, Gooden MJ, de Jong RA, Hoogeboom BN, ten Hoor KA, Hollema H, et al. Prognostic significance of tumor-infiltrating T-lymphocytes in primary and metastatic lesions of advanced stage ovarian cancer. Cancer Immunol Immunother 2009;58:449–59. 22. Halama N, Michel S, Kloor M, Zoernig I, Benner A, Spille A, et al. Localization and density of immune cells in the invasive margin of human colorectal cancer liver metastases are prognostic for response to chemotherapy. Cancer Res 2011;71:5670–7. 23. Dieu-Nosjean MC, Antoine M, Danel C, Heudes D, Wislez M, Poulot V, et al. Long-term survival for patients with non-small-cell lung cancer with intratumoral lymphoid structures. J Clin Oncol 2008;26: 4410–7. 24. Platonova S, Cherfils-Vicini J, Damotte D, Crozet L, Vieillard V, Validire P, et al. Profound coordinated alterations of intratumoral NK cell phenotype and function in lung carcinoma. Cancer Res 2011;71: 5412–22. Clinical Cancer Research Downloaded from clincancerres.aacrjournals.org on October 10, 2014. © 2013 American Association for Cancer Research. Published OnlineFirst June 19, 2013; DOI: 10.1158/1078-0432.CCR-12-3847 In Situ Immune Reaction in Lung Metastases 25. Altman DG, Lausen B, Sauerbrei W, Schumacher M. Dangers of using "optimal" cutpoints in the evaluation of prognostic factors. J Natl Cancer Inst 1994;86:829–35. 26. Faraggi D, Simon R. A simulation study of cross-validation for selecting an optimal cutpoint in univariate survival analysis. Stat Med 1996; 15:2203–13. 27. Camus M, Tosolini M, Mlecnik B, Pages F, Kirilovsky A, Berger A, et al. Coordination of intratumoral immune reaction and human colorectal cancer recurrence. Cancer Res 2009;69:2685–93. 28. Pfannschmidt J, Dienemann H, Hoffmann H. Surgical resection of pulmonary metastases from colorectal cancer: a systematic review of published series. Ann Thorac Surg 2007;84:324–38. 29. Ladanyi A, Kiss J, Somlai B, Gilde K, Fejos Z, Mohos A, et al. Density of DC-LAMP(þ) mature dendritic cells in combination with activated T lymphocytes infiltrating primary cutaneous melanoma is a strong independent prognostic factor. Cancer Immunol Immunother 2007; 56:1459–69. 30. Mlecnik B, Tosolini M, Kirilovsky A, Berger A, Bindea G, Meatchi T, et al. Histopathologic-based prognostic factors of colorectal cancers are associated with the state of the local immune reaction. J Clin Oncol 2011;29:610–8. 31. Ishigami S, Ueno S, Matsumoto M, Okumura H, Arigami T, Uchikado Y, et al. Prognostic value of CD208-positive cell infiltration in gastric cancer. Cancer Immunol Immunother 2009;59:389–95. 32. Motzer RJ, Bacik J, Murphy BA, Russo P, Mazumdar M. Interferon-alfa as a comparative treatment for clinical trials of new therapies against advanced renal cell carcinoma. J Clin Oncol 2002;20:289–96. 33. Heng DY, Xie W, Regan MM, Warren MA, Golshayan AR, Sahi C, et al. Prognostic factors for overall survival in patients with metastatic renal cell carcinoma treated with vascular endothelial growth factor-targeted agents: results from a large, multicenter study. J Clin Oncol 2009;27:5794–9. 34. de Chaisemartin L, Goc J, Damotte D, Validire P, Magdeleinat P, Alifano M, et al. Characterization of chemokines and adhesion molecules associated with T cell presence in tertiary lymphoid structures in human lung cancer. Cancer Res 2011;71:6391–9. 35. Halle S, Dujardin HC, Bakocevic N, Fleige H, Danzer H, Willenzon S, et al. Induced bronchus-associated lymphoid tissue serves as a general priming site for T cells and is maintained by dendritic cells. J Exp Med 2009;206:2593–601. 36. Grivennikov SI, Greten FR, Karin M. Immunity, inflammation, and cancer. Cell 2010;140:883–99. 37. Chomarat P, Banchereau J, Davoust J, Palucka AK. IL-6 switches the differentiation of monocytes from dendritic cells to macrophages. Nat Immunol 2000;1:510–4. www.aacrjournals.org 38. Menetrier-Caux C, Montmain G, Dieu MC, Bain C, Favrot MC, Caux C, et al. Inhibition of the differentiation of dendritic cells from CD34(þ) progenitors by tumor cells: role of interleukin-6 and macrophage colony-stimulating factor. Blood 1998;92:4778–91. 39. Gabrilovich DI, Chen HL, Girgis KR, Cunningham HT, Meny GM, Nadaf S, et al. Production of vascular endothelial growth factor by human tumors inhibits the functional maturation of dendritic cells. Nat Med 1996;2:1096–103. 40. Ohm JE, Carbone DP. VEGF as a mediator of tumor-associated immunodeficiency. Immunol Res 2001;23:263–72. 41. Li N, Grivennikov SI, Karin M. The unholy trinity: inflammation, cytokines, and STAT3 shape the cancer microenvironment. Cancer Cell 2011;19:429–31. 42. Grivennikov S, Karin E, Terzic J, Mucida D, Yu GY, Vallabhapurapu S, et al. IL-6 and Stat3 are required for survival of intestinal epithelial cells and development of colitis-associated cancer. Cancer Cell 2009;15: 103–13. 43. Negrier S, Escudier B, Lasset C, Douillard JY, Savary J, Chevreau C, et al. Recombinant human interleukin-2, recombinant human interferon alfa-2a, or both in metastatic renal-cell carcinoma. Groupe Francais d'Immunotherapie. N Engl J Med 1998;338:1272–8. 44. Kim WY, Kaelin WG. Role of VHL gene mutation in human cancer. J Clin Oncol 2004;22:4991–5004. 45. Corzo CA, Condamine T, Lu L, Cotter MJ, Youn JI, Cheng P, et al. HIF1alpha regulates function and differentiation of myeloid-derived suppressor cells in the tumor microenvironment. J Exp Med 2010;207: 2439–53. 46. Motz GT, Coukos G. The parallel lives of angiogenesis and immunosuppression: cancer and other tales. Nat Rev Immunol 2011;11: 702–11. 47. Gabrilovich DI, Ostrand-Rosenberg S, Bronte V. Coordinated regulation of myeloid cells by tumours. Nat Rev Immunol 2012;12: 253–68. 48. Perier A, Fregni G, Wittnebel S, Gad S, Allard M, Gervois N, et al. Mutations of the von Hippel-Lindau gene confer increased susceptibility to natural killer cells of clear-cell renal cell carcinoma. Oncogene 2011;30:2622–32. 49. Salmon H, Franciszkiewicz K, Damotte D, Dieu-Nosjean MC, Validire P, Trautmann A, et al. Matrix architecture defines the preferential localization and migration of T cells into the stroma of human lung tumors. J Clin Invest 2012;122:899–910. 50. Pages F, Galon J, Dieu-Nosjean MC, Tartour E, Sautes-Fridman C, Fridman WH. Immune infiltration in human tumors: a prognostic factor that should not be ignored. Oncogene 2009;29: 1093–102. Clin Cancer Res; 19(15) August 1, 2013 Downloaded from clincancerres.aacrjournals.org on October 10, 2014. © 2013 American Association for Cancer Research. 4091