* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download ID immunity-part1
West Nile fever wikipedia , lookup
Tuberculosis wikipedia , lookup
African trypanosomiasis wikipedia , lookup
Onchocerciasis wikipedia , lookup
Neonatal infection wikipedia , lookup
Middle East respiratory syndrome wikipedia , lookup
Human cytomegalovirus wikipedia , lookup
Gastroenteritis wikipedia , lookup
Poliomyelitis eradication wikipedia , lookup
Sexually transmitted infection wikipedia , lookup
Marburg virus disease wikipedia , lookup
Leptospirosis wikipedia , lookup
Orthohantavirus wikipedia , lookup
Hepatitis C wikipedia , lookup
Poliomyelitis wikipedia , lookup
Typhoid fever wikipedia , lookup
Cysticercosis wikipedia , lookup
Meningococcal disease wikipedia , lookup
Hepatitis B wikipedia , lookup
Anthrax vaccine adsorbed wikipedia , lookup
Neisseria meningitidis wikipedia , lookup
Eradication of infectious diseases wikipedia , lookup
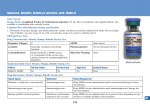
Infectious Disease & Immunity Dr. D. Barry Part 1 1) Immune System 2) Vaccinations 3) Vaccine Preventable Diseases Part 2 1) Assessing the Febrile Child 2) Common Childhood Infections 3) Antibiotic choices 4) Immunodeficiencies 1; Immune System Immune system Neonates have immature immune system (esp. adaptive system; lymphocytes, antibodies) Lymphocytes ↑ (thymus) & mature with antibody production relative to exposure Foetal/ Neonatal monocytes, mØ slow to process foreign antigens Infants produce a/b against simple proteins (eg. Vaccines) not polysaccharides until 2 years Foetal Lymphocytes from 9/40 in liver Bone, liver, spleen 12/40 T-cells from 14/40 & In utero sterile environment (ideally) Therefore no anti-bodies produced Mum’s IgG only crosses placenta Neonatal antibodies IgG; Transplacental ie maternal T1/2 21 days Nadir at 3-5months Infant’s own IgG takes over 60% of adult’s level at 1 year 100% by 6-10 years IgM; v low at birth; 75% adult level at 1 yr * IgA, IgD, IgE; 10-40% at 1 yr Exposure; 7-8 viral infections/yr ↑ with contacts (creche / school) Vast array of childhood infections from benign to critical; your job to find out which Hygiene Hypothesis ↑ allergic / immune-mediated disorders in developed nations ? ‘too clean’ environment Microbial exposure needed Causes shift from predominance of Th1 to Th2 cells, causing over-production of IgE etc. Hypersensitivity ensues [J Hopkins & T Shirakawa Science 1997 Immune system; ‘in balance’ Infection; viral/bacterial/opportunistic Hypersensitivity; Allergy, Atopy, Intolerance Autoimmune disorders Immunodeficencies Therapeutic; Vaccinations Monoclonal antibodies IVIG 2; Vaccinations “Medicine’s greatest lifesaver” Ireland; Mycobacterium Diphtheria Tetanus Pertussis Polio Haemophilus influenza b Hepatitis B Meningococcal C Pneumococcus Measles Mumps Rubella } 12 vaccines BCG* x 1 } 6in1 x3 Men C x 3 PCV x 3 MMR* x 2 Age Vaccination Birth BCG 2 months 6in1 & PCV 4 months 6in1 & Men C 6 months 6in1 & Men C & PCV 12 months MMR & PCV 13 months Men C & Hib 4 – 5 years 4in1 & MMR 11-14 years Td Those born before July 2008 Age Birth 2 months 4 months 6 months 12-15 months 4-5 years Vaccine BCG 5in1, MenC 5in1, MenC 5in1, MenC MMR, Hib 4in1, MMR No Routine Hepatitis B or Pneumococcal vaccine PCV Catch-up programme (for <2 year olds) Why Immunise? In 1974, only 5% of the worlds children had access to vaccines. A global effort in the early ’80’s aimed to provide six vaccines to 80% of children worldwide Immunisation now saves >3,000,000 lives each year Protects millions more from illness and permanent disability Other vaccines Influenza Varicella Hepatitis A HPV Travel vaccines What is immunisation? Immunisation is the process of inducing or providing immunity artifically. This may be done by the administration of a vaccine, toxoid or externally produced antigen in order to stimulate antibody production. The aim; to reduce the incidence of, or to eliminate a particular disease. Immunisation has both a direct and an indirect effect. Direct effect; antibody protection in the individual Indirect effect; reduction of the incidence of the disease in others – so called ‘herd immunity’ Vaccine Considerations Pathogen factors; How common? Vaccine factors; vaccine immunogenicity efficacy, side-effects & risks? Host factors; maturity immune system, How dangerous / complications? When is infant most at risk of this disease? Population factors; disease prevalence, vaccine uptake & herd immunity, cost-benefit Live Attenuated Measles Mumps Rubella BCG Killed Orgs Polio (IPV) Influenza Subunits Hib Men C Pneumo (PCV) Hep B Acellular Pertussis Varicella Cellular Pertussis Cholera/typhoid/ Cholera/Typhoid Hep A yellow fever /Rabies Oral Polio MMR Vaccine: Is It Really A Factor In Autism? There has been a concern about a link between the MMR (measles, mumps, rubella) vaccine and the development of autism in children because: – MMR vaccine is first given at age 12 to 15 months. – The first signs of autism (e.g. poor social interaction and speech, repetitive behaviors) often appear between 12 to 18 months of age. MMR vaccine first given Birth 0 months First signs of autism 12 months 15 months Independent Studies Have Found No Link Between Autism and MMR. A United States study by Dr. Loring Dales showed that the number of autism cases in young children increased even when the number of MMR vaccines decreased over the same time period! A British study by Dr. Brent Taylor showed that the number of diagnosed autism cases did not increase after the MMR vaccine was introduced in 1988. If a link existed between the MMR vaccine and autism, then one would expect the number of autism cases to increase or decrease over time as the number of children immunised with MMR decreases or increases over the same time. No study has shown this trend. Additional studies conducted in the United States and in Europe have found no association between the MMR vaccination and autism. WHO opinion on MMR "WHO has noted that other scientists have not been able to reproduce the results claimed by Dr Wakefield and his team regarding measles virus in the gut. His published observations regarding the onset of autism following administration of MMR vaccine do not meet the scientific criteria required to suggest that the vaccine is the cause. Other studies not cited by Dr Wakefield find no link with autism or Crohn's disease." WHO strongly endorses the use of MMR (measles, mumps and rubella) vaccine on the grounds of its convincing record of safety and efficacy. IRISH Working Party Consensus The Joint Committee considers that: there is no evidence of a proven link between MMR and autism. there is no evidence to show that the separate vaccines are any safer than the combined MMR vaccine. Babies are very susceptible to measles, mumps and rubella, which are killer diseases, so they much be protected as soon as possible and this can only be done with the MMR vaccine. Giving separate measles, mumps and rubella vaccines would leave children unnecessarily exposed and vulnerable. Late Entrants To Irish Health Care System MMR; Immunisation recommended 2 doses recommended between 12-15 mo and 4-6 yrs at least 1 month apart Men C; recommended under 22 years Hib; Recommended under aged 4 years ( 3 doses < 1 yr, 1 dose > 1yrs) Polio; 4 doses recommended before the age of 4-6 yrs DtaP; recommended under 12 years If it is likely 3 or more doses given, serological testing for IgG antibodies +/- booster If a child at presentation is > 10yrs Td is given Contraindications/ Precautions ……..NOT Contraindications Family history of adverse reactions to immunisations Minor infections without fever or systemic upset Family hx of convulsions History of measles, mumps, pertussis in the absence of proof of immunity Child’s mother is pregnant or Child being breast-fed Impending surgery Child over the recommended age Corticosteroid replacement therapy Diphtheria Corynebacterium diphtheriae Affects upper respiratory tract Incubation – 2-5 days Spread; droplet/close contact Disease characterised by an inflammatory exudate obstructive membrane over the airway Other manifestation: Myocarditis Vocal cord paralysis Guillain Barre type ascending paralysis Since vaccination; virtually eliminated in Ireland Vaccine Toxoid Component of 6 in 1 Booster at 4-5yrs and low dose booster at 11-14 yrs Adverse reactions Transient local reactionc occur in > 50% Malaise, headache and transient fever occur occasionally Tetanus Clostridium tetani Muscular rigidity with superimposed contractions Organism is ubiquitous Nb; puncture wounds, bites etc. Incubation period: 4-21 days Vaccine Primary immunisation Toxoid Poor immunogen 6 in 1, three doses Booster dose at school entry and at 11-14yrs Immunised adults who have received 5 doses do not need further booster doses Pertussis (Whooping cough) Bordetella pertussis Highly infectious (90% of nonimmune contacts acquire it) 3 phases Transmitted; droplets etc. 1-2 week incubation Endemic with periodic outbreaks Diagnosis; often clinical Peri-nasal swab; poor yield Lymhocytosis Treatment; Isolate Erythromycin reduces infectivity Supportive Vaccination ‘100 day cough’ Catarrhal phase; 1-2 weeks of low fever, URTI Highly infectious Transmission; Droplet/ close contact Paroxysmal phase; Whoop (gasps for breath between coughing fits) 3-5 weeks Often associated vomiting etc. Recovery phase; 2-3 weeks Complications; Apnoea in neonates Bronchopneumonia Cerebral hypoxia; Seizures, Encephalopathy Death Vaccine Acellular pertussis 6 in 1 x 3 Booster at 4-5 yrs No upper age limit but considered unnecessary > 7 yrs Efficacy variable; 35 – 100% in studies Previous concern re; seizures induced by Cellular Vaccine (not used anymore) Pertussis - special precautions Advice from the child’s paediatrician may need to be sought prior to immunisation where there is: A personal history of convulsions An evolving neurological problem If an event listed in precaution section has occurred after a previous dose Poliomyelitis Caused by polio virus 1-3 Transmission; faecal/oral, droplet Incubation: 3- 21 days Clinical disease Non-paralytic fever Aseptic meningitis Paralysis Pre-vaccine; 20,000 cases/yr USA 1,900 deaths /yr Ireland most recent case 1984 Endemic in developing world Vaccine Most infections asymptomatic IPV since 2001 Part of 6 in 1 3 doses + 4th at 4- 5 yrs OPV not recommended Haemophilus influenzae type B Hib vaccine introduced 1992 80% of invasive haemophilus infections caused by type B After 12 months of age, Hib disease declines Clinical disease includes: Meningitis Epiglottis Septicaemia Cellulitis Osteomyelitis Septic arthritis Vaccine Capsular poly or oligosaccharide Part of 6 in 1 3 doses + booster If first dose given at > 1 yr need only 1 dose Children > 4 yrs do not need immunisation with Hib Persons with asplenia or undergoing splenectomy should be vaccinated Hib Treatment Index case; tx with cefotaxime or ceftriaxone Household contacts / Play-group/ creche; chemoprophylaxis Immunise 1 month after disease if < 2 yrs Except pregnant women Non-immunised contacts < 4yrs need vaccine All household contacts irrespective of age or immunisation history IF there are any unvaccinated children< 4yrs Chemoprophylaxis; Rifampicin Neonates and infants < 1 yr : 10mg/kg od for 4 days Children > 1 yr: 20mg/kg od for 4 days ( max 600mg/day) Adults : 600mg one daily x 4 days Hepatitis B DNA virus Highly contagious 30% transmission rate with puncture injury High risk contacts 10% chronic infection, 1% fulminant hepatitis Risk of Hepatocellular Ca Hepatitis B vaccination Traditionally only vaccinated high risk groups Sex workers Individuals who change sexual partner frequently IVDU’s Prisoners Tattoo artists Homeless people Immigrants from, or travellers to, areas with a high prevalence of HBV Security and emergency services personnel Family contacts of HBV pts CRF / HIV / chronic hepatitis Healthcare workers Hepatitis B vaccine Vaccine; HBsAg in 6in1 Primary Immunisation Schedule (since July) At 2, 4, 6/12 At birth with HBIG if risk of vertical transmission + follow-up testing No Catch-up unless at risk Meningococcus C Neisseria Meningitidis Gram neg. cocci Causes Meningitis, Septicaemia Notifiable disease Contact tracing & chemoprophylaxis required Contact tracing/ prophylaxis Antibiotic prophylaxis for close contacts of confirmed or suspected cases: Close contacts defined as those who in the seven days prior to the onset of illness in the index case Rifampicin is drug of choice Have shared living or sleeping accomodation Had mouth kissing contact with the patient Nursery/creche /daycare contacts Medical personnel who have had ‘intimate’ contact with the patient ( mouth-to-mouth, intubation) Alternative prophylaxis is Ceftriaxone 250 mg im for adults and 125mg for children For vaccine preventable strains (A, C, W-135) vaccination is offered. Streptococcal Pneumoniae Capsular organism Gram + Diplococci Some asymptomatic carriers Diseases; Meningitis with effusions Pneumonia with effusions Bacteraemia/Sepsis Otitis Media Sinusitis Pneumococcal Conjugate Vaccine 7 serotypes (75-80% invasive pneumococcus) ↑ immunogenicity with mutant diphtheria toxin > 90% effective 23-valent polysaccharide available for high risk children > 2years age eg. Asplenia Effective for 5 years Not in Primary Immunisation Schedule Measles Transmission; airborne/droplet Incubation; 10-14 days Clinical; Prodrome; high fever, harsh cough, coryza, conjunctivitis, Rash; ‘morbilliform’, maculopapular Begins d3-6 from hairline, down face to trunk Lasts up to 10/7 Koplik’s spots Measles (Rubeola) Complications; RNA Paramyxovirus Otitis, pneumonia, croup Clinical diagnosis Salivary swab measles IgM Encephalitis 1/5000 within a week of rash Treatment 15% Mortality Supportive 20-40% Neuro Ribavirin if patient sequelae Immunocompromised Late complication; ?Contacts Prevention: HNIG within SSPE (subacute sclerosing panencephalitis) 6/7 if imunocompromised 1/100,000 contact Measles Vaccine; MMR 12-15 months of age, 2nd dose at 4-5 yrs Can be given to those with history of measles, mumps or rubella infection Mini-measles can occur 6 -10 days after immunisation Mild pyrexia and erythematous rash Measles outbreak Immunise all susceptible individuals within 72 hrs Contraindications; Pregnancy is a contraindication and should be avoided for 2 months after vaccination Untreated malignancy and immunodeficiency states (except HIV) Immunosuppressive therapy History of anaphylaxis to a previous dose Mumps Acute viral illness Swelling of one or more salivary glands usually the parotids CNS involvement is frequent Symptomatic meningitis occurs in <10% Rarely transverse myelitis, cerebellar ataxia or encephalitis can occur Orchitis occurs in 20% of post-pubertal males Sterility rare Other manifestations Arthritis, carditis, nephritis, pancreatitis, thyroiditis, hearing impairment Transmission is by droplet Incubation period: 12 -25 days Vaccine; live MMR Rubella Rubella – difficult to diagnose Fever <38.5, LN + (esp Post Triangle) May have splenomegaly, palatal petechiae Mild self limited disease in children – 25 -50% subclinical Incubation 2 – 3 weeks Infectious (droplets) for <1wk from rash onset Buccal swab, urine, rising antibody titre Rare complications: Polyarthralgia / Polyarthritis Thrombocytopenia Encephalitis (1 in 6000) Congenital Rubella LBW, growth retardation Microcephaly, learning disability, psyche Microphthalmia, catarract, glaucoma Micrognathia Sensori-neural deafness Hepato-Spleno-megaly (transient), diabetes Thrombocytopenic purpura ‘blueberry muffin’ PDA Congenital Rubella 1964-1965 USA; Rubella epidemic; 12.5mil cases with 20,000 cases congenital rubella 2001; 19 cases Rubella in USA Serology checked on antenatal booking bloods >80% women infected in 1st trimester; affected infants Infants with congenital rubella may shed virus for over a year MMR Prevention: Active vaccination Rubella component of MMR vaccine occasionally produces mild arthralgia especially in post pubertal girls (25%) Pregnancy remains a contraindication (no evidence of congenital rubella related to vaccine) HIV And Immunisation Children With HIV infection whether symptomatic or asymptomatic should receive: DtaP, IPV, Hib, Men C as per primary schedule Yearly influenza vaccine beginning at 6 months Pneumococcal (conjugate) vaccine at 2,4 and 6 months MMR at 14 months ( unless severely immunocompromised), 2nd dose 1-2 months later BCG if infant has 2 negative HIV PCR tests in the first 6 weeks of life Hepatitis A Hepatitis B Summary Neonates & Infants immature immune systems Vaccines very effective protection Know schedule (old & new & catch-up) Know diseases they prevent (MCQs) Age Vaccination Birth BCG 2 months 6in1 & PCV 4 months 6in1 & Men C 6 months 6in1 & Men C & PCV 12 months MMR & PCV 13 months Men C & Hib 4 – 5 years 4in1 & MMR 11-14 years Td