* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Childhooh Infections - Welcome to Selly Park Technology
Dirofilaria immitis wikipedia , lookup
Sarcocystis wikipedia , lookup
Herpes simplex wikipedia , lookup
Gastroenteritis wikipedia , lookup
Brucellosis wikipedia , lookup
African trypanosomiasis wikipedia , lookup
Meningococcal disease wikipedia , lookup
Oesophagostomum wikipedia , lookup
Onchocerciasis wikipedia , lookup
Orthohantavirus wikipedia , lookup
Trichinosis wikipedia , lookup
Ebola virus disease wikipedia , lookup
Rocky Mountain spotted fever wikipedia , lookup
Human cytomegalovirus wikipedia , lookup
Herpes simplex virus wikipedia , lookup
Neonatal infection wikipedia , lookup
Whooping cough wikipedia , lookup
Sexually transmitted infection wikipedia , lookup
Schistosomiasis wikipedia , lookup
Eradication of infectious diseases wikipedia , lookup
West Nile fever wikipedia , lookup
Henipavirus wikipedia , lookup
Neisseria meningitidis wikipedia , lookup
Middle East respiratory syndrome wikipedia , lookup
Hepatitis C wikipedia , lookup
Coccidioidomycosis wikipedia , lookup
Hospital-acquired infection wikipedia , lookup
Marburg virus disease wikipedia , lookup
Leptospirosis wikipedia , lookup
Hepatitis B wikipedia , lookup
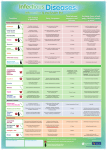
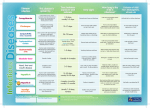
Common Childhood Illnesses •Transmission •Symptoms •Prevention LBeattie – 2006 Viruses can enter our bodies in a variety of ways, for example... LBeattie – 2006 How Disease Is Transmitted • The process begins with someone who has the infection • The infectious pathogen (bacteria, virus, fungus, or parasite) leaves the sick person’s body • The infectious pathogen reaches another child and enters his body • The child develops the infection LBeattie – 2006 Most common ways of the infection transmission in child care 1. INHALATION • inhaling droplets of moisture containing viruses, bacteria, etc, from an infected person who has coughed or sneezed • touching surfaces covered by droplets or from the person’s hands and then touching our own face or eyes – surfaces include door knobs, – telephones, toys, flush handles LBeattie – 2006 INHALATION What can you catch? • • • • • • • • • colds and flu TB measles mumps rubella whooping cough chickenpox conjunctivitis viral gastro-enteritis LBeattie – 2006 INHALATION PREVENTION of the INFECTION • difficult to avoid getting infected • cover mouth or nose when coughing or sneezing • wash hands if you have contact with items or fabrics contaminated with droplet fluids • encourage parents to keep their infectious child away from nursery until they are well LBeattie – 2006 2. INGESTION – eating contaminated food or drinking contaminated water – sucking fingers, thumbs, biting finger nails, smoking a cigarette with dirty hands – hands can become contaminated from touching pets, farm animals, raw meat and poultry, soiled nappies, toilets... LBeattie – 2006 INGESTION What can you catch? salmonella food poisoning dysentery hepatitis A threadworms LBeattie – 2006 INGESTION PREVENTION of the INFECTION • you can have some control over getting infected – always wash hands after touching animals and pets, using the toilet and changing nappies – always wash hands before and after preparing food and before eating – follow good practices for storing, – cooking chilling and re-heating food LBeattie – 2006 3. INOCULATION • by blood or certain body fluids from an infected person, getting into the body of another person – through cuts or damaged skin – by injection through the skin e.g. – body piercing, tattoos, IV drug use, blood transfusion LBeattie – 2006 INOCULATION What can you catch? • HIV which can lead to AIDS • hepatitis B • hepatitis C LBeattie – 2006 INOCULATION PREVENTION of the INFECTION • you can have a lot of control over getting infected • cover any cuts and abrasions with water proof dressing if giving care or dealing with blood • use of disposable plastic aprons and disposable gloves when dealing with body fluids • wash hands after removing gloves LBeattie – 2006 SKIN to SKIN and HEAD to HEAD What can we catch? • cold sores via kissing • body lice - and in clothing and bedding • fungal infections ringworm, athlete’s foot • warts and verrucaes • impetigo - and from items soiled with pus • HEAD to HEAD - head lice LBeattie – 2006 SKIN to SKIN PREVENTION • you can have some control over getting infected – make sure that all people are treated so that they are no longer infectious to others – avoid contact with infected areas either by person covering with dressing or carer using gloves – washing skin immediately after contact can reduce transmission of infection LBeattie – 2006 HEAD to HEAD PREVENTION • can be difficult to avoid getting infected during close social interaction – make sure that all children are treated to prevent re-infection – check young children’s heads after each hair wash, on wet hair, using a detection comb LBeattie – 2006 Common childhood infections you may come across • • • • • • • • Chickenpox German measles (Rubella) Measles Meningites Mumps Tonsillitis Whooping Cough (Pertussis) Gastro-enteritis LBeattie – 2006 Chickenpox • • • • droplet spread e.g. via coughing and sneezing or by direct contact with blister fluid incubation period 13-17 days infectious 4 days before onset of rash until 5 days after appearance of first spots. May return to nursery after 5 days of spots appearing if feeling well pregnant women should seek antenatal advice – first 20 weeks and last 3 weeks LBeattie – 2006 Rash of chickenpox LBeattie – 2006 Rubella (German measles) • caused by virus which causes mild fever and a rash • fever, swollen neck glands, fine rash • spread by direct contact with sneezing or coughing incubation period 16-18 days • The disease is potentially serious because of the ability to produce defects in a developing fetus if the mother is infected during early pregnancy LBeattie – 2006 Rubella syndrome is a group of physical abnormalities that have developed in an infant as a result of maternal infection with rubella virus. It is characterized by rash at birth, low birth weight, small head size, heart abnormalities, visual problems and bulging fontanelle. LBeattie – 2006 Measles • caused by a virus, rare in this country since introduction of MMR vaccine • fever, conjunctivitis, cough and/or spots on cheeks or inside mouth. 3-7 days later red, blotchy rash appears which lasts 4-7 days. Complications of pneumonia can occur. Incubation 7-14 days • spread by contact with coughing and sneezing LBeattie – 2006 Meningitis • meningitis is an inflammation of the brain membranes • caused by different bacteria and viruses • symptoms include severe headache / high pitched cry in babies, drowsiness, stiff neck, repeated vomiting, irritability, fever, dislike of bright lights • CAN CAUSE DEATH! GLASS TEST •Press the side of a glass firmly against the rash. •If the rash fades and loses colour under pressure it is not a meningitis rash. •If it does not change colour, you should contact a doctor immediately. LBeattie – 2006 Viral gastro-enteritis • • • • • can be caused by bacteria or virus sudden onset of vomiting and or diarrhoea very infectious (from spray created when ill) usually short-lasting = 24/48hrs thorough cleaning of wide area after illness episodes and isolation can reduce spread LBeattie – 2006 Viral hepatitis (can be of A, B or C type) • hepatitis is an inflammation of the liver • hepatitis A is caught by swallowing the virus (contaminated food, water and from hands soiled with faeces) • after 6 weeks - lethargy, nausea, pain in abdomen • no treatment, usually full recovery • vaccination can protect contacts and travellers LBeattie – 2006 Mumps • caused by a virus • fever, swelling of one or more salivary glands in the neck. • mumps virus can cause meningitis and deafness • passed from one person to another via droplets (sneezing, coughing) or direct contact with saliva • incubation normally 18 days but can be 12-25 days LBeattie – 2006 Fifth disease (“slapped cheek” disease) • caused by a virus. Usually mild • red rash on cheeks, followed by lace-like rash on the body and limbs for up to 3 weeks • infectious before onset of rash. Mostly spread by droplets • pregnant women should seek advice ASAP especially if in first 20 weeks LBeattie – 2006 Whooping cough (Pertussis) the signs of the disease are: coughing fits accompanied by a loud "whooping" sound as the child inhales, and vomiting. the complications of whooping cough include: pneumonia and brain damage caused by oxygen deficiency. can be treated with antibiotics or prevented by immunization. LBeattie – 2006 Tetanus • is transmitted when tetani bacillus enters open wounds • the signs of the disease are: muscle spasms throughout the entire body, lockjaw, paralysis of the respiratory muscles, irritability, fever • can be prevented by immunization. LBeattie – 2006 Preventing Infections Promote Good Practice • establish a daily cleaning routine - pay particular attention to play areas and surfaces, toilets, kitchens, highchairs and nappy changing areas • establish a rota for cleaning toys, sand, water play areas, etc. • provide suitable handwashing facilities and ensure regular use! • ensure disposable gloves and aprons are available for nappy changing and when carrying out first aid LBeattie – 2006 Raising Children’s Awareness • teach the importance of regular handwashing and supervise, especially after going to the toilet and before eating • cleaning teeth • wiping noses and disposing of tissues • covering mouths when coughing or sneezing LBeattie – 2006 Case Scenario A worried mother calls the nursery on Monday morning to inform you that her son has been admitted to hospital with suspected meningitis. Her son has been attending the nursery full time and was present the previous Friday. What should you do in this situation? LBeattie – 2006 Case Scenario 1 Answers • Don’t panic! • Ask for help: inform your supervisor; contact local NHS unit who will establish the facts and advise (including advice to parents) • If confirmed as a case of meningitis, it will be necessary for GPs to follow up close contacts • close contacts include family members, kissing contacts and those who have stayed overnight with the family during the past 10 days LBeattie – 2006 Case Scenario Answers (cont) • ensure that you are aware of the signs and symptoms of meningitis • if you suspect symptoms in another child seek medical assistance promptly • if another suspected case arises within a 4 week period then prophylactic antibiotics may be administered - the NHS unit will determine this LBeattie – 2006