* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download PDF
Kawasaki disease wikipedia , lookup
Neonatal infection wikipedia , lookup
Neglected tropical diseases wikipedia , lookup
Rheumatic fever wikipedia , lookup
Traveler's diarrhea wikipedia , lookup
Germ theory of disease wikipedia , lookup
Typhoid fever wikipedia , lookup
Onchocerciasis wikipedia , lookup
Infection control wikipedia , lookup
Whooping cough wikipedia , lookup
Cryptosporidiosis wikipedia , lookup
Hospital-acquired infection wikipedia , lookup
Schistosomiasis wikipedia , lookup
Gastroenteritis wikipedia , lookup
Globalization and disease wikipedia , lookup
Common cold wikipedia , lookup
Coccidioidomycosis wikipedia , lookup
Transmission (medicine) wikipedia , lookup
Childhood immunizations in the United States wikipedia , lookup
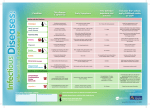
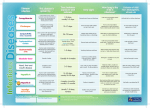
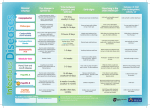
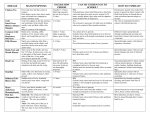
Infectious This disease is spread by Condition Early Symptoms Time between exposure and sickness Exclusion from school, early childhood centre, or work* Rashes and skin infections Coughing, sneezing and contact with weeping blisters. Fever and spots with a blister on top of each spot. 10–21 days after being exposed. 1 week from appearance of rash, or until all blisters have dried. Hand, foot and mouth disease Coughing, sneezing, and poor hand washing. Fever, flu-like symptoms – rash on soles and palms and in the mouth. 3–5 days Exclude until blisters have dried. If blisters able to be covered, and child feeling well, they will not need to be excluded. Head lice (Nits) Direct contact with an infested person’s hair. Itchy scalp, especially behind ears. Occasionally scalp infections that require treatment may develop. N/A None, but ECC/school should be informed. Treatment recommended to kill eggs and lice. Coughing and sneezing. Direct contact with an infected person. Highly infectious. Runny nose and eyes, cough and fever, followed a few days later by a rash. 7–18 days 5 days after the appearance of rash. Non-immune contacts of a case may be excluded. Contact with infected skin, bedding and clothing. Flat, ring-shaped rash. 4–6 weeks None, but skin contact should be avoided. Rubella Coughing and sneezing. Also direct contact with an infected person. Fever, swollen neck glands and a rash on the face, scalp and body. 14–23 days Until well and for 7 days from appearance of rash. Scabies Contact with infected skin, bedding and clothing. Itchy rash. 4–6 weeks (but if had scabies before it may develop within 1–4 days) Exclude until the day after appropriate treatment. Direct contact with infected sores. Blisters on the body which burst and turn into scabby sores. Variable Until sores have dried up or 24 hours after antibiotic treatment has started. Coughing and sneezing. The virus may be passed from mother to child during pregnancy. Red cheeks and lace-like rash on body. 4–20 days Unnecessary unless unwell. Until well and for 48 hours after the last episode of diarrhoea or vomiting. Cryptosporidium – do not use public pool for 2 weeks after symptoms have stopped. Salmonella - Discuss exclusion of cases and contacts with public health service. Chickenpox Measles Ringworm (German Measles) School sores (Impetigo) Slapped cheek (Human parvovirus infection) Diarrhoea & Vomiting illnesses Campylobacter Cryptosporidium Giardia Salmonella Undercooked food, contaminated water. Direct spread from an infected person or animal. Stomach pain, fever, nausea, diarrhoea and/or vomiting. Campylobacter 1–10 days Cryptosporidium 1–12 days Giardia 3–25 days Salmonella 6–72 hours Hepatitis A Contaminated food or water, direct spread from an infected person. Nausea, stomach pains, general sickness. Jaundice a few days later. 15–50 days 7 days from the onset of jaundice. Norovirus Contact with secretions from infected people. Nausea, diarrhoea/and or vomiting. 1–2 days Until well and for 48 hours after the last episode of diarrhoea or vomiting. Rotavirus Direct spread from infected person. Nausea, diarrhoea/and or vomiting. 1–2 days Until well and for 48 hours after the last episode of diarrhoea or vomiting. Contaminated food or water, contact with an infected person. Diarrhoea (may be bloody), fever, stomach pain. 12 hours–1 week Discuss exclusion of cases and their contacts with public health service. Contaminated food or water, unpasteurised milk. Direct contact with animals or infected person. High incidence of bloody diarrhoea, stomach pain. High rate of hospitalisation and complications. 2–10 days Discuss exclusion of cases and their contacts with public health service. Influenza and Influenza-like illness (ILI) Coughing and sneezing. Direct contact with infected person. Sudden onset of fever with cough, sore throat, muscular aches and a headache. 1–4 days (average about 2 days) Until well. Streptococcal sore throat Contact with secretions of a sore throat. (Coughing, sneezing etc.) Headache, vomiting, sore throat. An untreated sore throat could lead to Rheumatic fever. 1–3 days Exclude until well and/or has received antibiotic treatment for at least 24 hours. Coughing. Adults and older children can pass on the infection to babies. Runny nose, persistent cough followed by “whoop”, vomiting or breathlessness. 5–21 days Five days from commencing antibiotic treatment or, if no antibiotic treatment then 21 days from onset of illness or until no more coughing, whichever comes first. Direct contact with discharge from the eyes or with items contaminated by the discharge. Irritation and redness of eye. Sometimes there is a discharge. 2–10 days (usually 3–4 days) While there is discharge from the eyes. Close contact with oral secretions. (Coughing, sneezing, etc.) Generally unwell, fever, headache, vomiting, sometimes a rash. Urgent treatment is required. 3–7 days Until well enough to return. Meningitis – Viral Spread through different routes including coughing, sneezing, faecal-oral route. Generally unwell, fever, headache, vomiting. Variable Until well. Mumps Coughing, sneezing and infected saliva. Pain in jaw, then swelling in front of ear and fever. 12–25 days Exclude until 5 days after facial swelling develops, or until well. Shigella VTEC/STEC (Verocytotoxin- or shiga toxin-producing E. coli) Respiratory Infections Whooping cough (Pertussis) Other Infections Conjunctivitis (Pink eye) Meningococcal Meningitis For further information contact: Your Public Health Nurse Vaccine-preventable and/or on National Immunisation Schedule Your Public Health Service * Seek further advice from a healthcare professional or public health service Notifiable disease (Doctors notify the Public Health Service) Pregnant women should seek advice from their maternity provider or G.P Revised March 2016. 06/2016. Code HE1214