* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Bacteria/Viruses and Disease - UCO
Hospital-acquired infection wikipedia , lookup
Typhoid fever wikipedia , lookup
Epidemiology of HIV/AIDS wikipedia , lookup
African trypanosomiasis wikipedia , lookup
Human cytomegalovirus wikipedia , lookup
Yellow fever wikipedia , lookup
Hepatitis C wikipedia , lookup
Onchocerciasis wikipedia , lookup
Schistosomiasis wikipedia , lookup
Rocky Mountain spotted fever wikipedia , lookup
History of biological warfare wikipedia , lookup
Herpes simplex wikipedia , lookup
Poliomyelitis wikipedia , lookup
Sexually transmitted infection wikipedia , lookup
Hepatitis B wikipedia , lookup
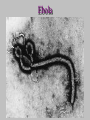
Ebola virus disease wikipedia , lookup
Leptospirosis wikipedia , lookup
West Nile fever wikipedia , lookup
Herpes simplex virus wikipedia , lookup
Henipavirus wikipedia , lookup
Coccidioidomycosis wikipedia , lookup
Middle East respiratory syndrome wikipedia , lookup
Orthohantavirus wikipedia , lookup
Marburg virus disease wikipedia , lookup
Lymphocytic choriomeningitis wikipedia , lookup
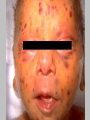
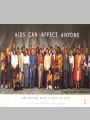
Viruses Smallpox The Year Was 1777 • It was a bold executive decision. Faced with a bio-terrorist threat, the commander in chief issued an order that every soldier be inoculated against smallpox, despite serious concerns about the medical risks involved. • The Commander in Chief of the Continental Army was George Washington. • Hearing of possible enemy plans to infect his troops with the dreaded smallpox virus, the future president had all recruits to his ragtag army “vaccinated” with infected material • This was especially daring because it was during the period that the church was condemning innoculation. • Washington’s call proved to be right. He subsequently lost no soldiers in the great smallpox epidemic that swept the Colonies, and indeed some historians believe this decision in large part determined the outcome of the War of Independence. The distribution of the smallpox rash is usually similar to that shown here. It is most dense on the face, arms and hands, legs and feet. The trunk has fewer pocks than the extremities. Smallpox on Infant Smallpox • Believed to have originated over 3,000 years ago in India or Egypt • Considered to be one of the most devastating diseases known to humanity. • In some ancient cultures, smallpox was such a major killer of infants that custom forbade the naming of a newborn until the infant had caught the disease and proved it would survive. • Fatal Infectious Disease (severe rash which leaves scars, fever, headache, vomiting and diarrhea. ) • No Treatment / No Cure •Vaccination Available • Direct Person-to- Person Contact • Used in Biological Warfare during French and Indian War • In 1763 Sir Jeffrey Amhurst, commander in chief of the British forces fighting a North American Indian uprising west of the Allegheny mountains, wrote to Colonel Bouquet: "Could it not be contrived to send the Smallpox among those disaffected tribes of Indians?" • Bouquet replied: "I shall try and inoculate them with some blankets, and take care not to get the disease myself. Smallpox Cycle • The rash appears 2 to 4 days after the patient first becomes ill with fever Smallpox Cycle • On the second day of rash, more papules appear. Although they differ somewhat in size, note that they all have a very similar appearance. Smallpox Cycle • By day 3, the rash has become more distinct and raised above the skin surface. Fluid is accumulating in the papules to form vesicles. Smallpox Cycle • By day 4, the vesicles are more distinct. Although they contain fluid, they feel very firm to the touch. When broken, they do not collapse because the fluid is contained in many small compartments. Smallpox Cycle • By day 5, the fluid in the vesicles has become cloudy and looks like pus. At this stage, the pocks are called pustules. At this time, the fever usually rises and the patient feels more ill than before. Smallpox Cycle • On day 7, the rash is definitely pustular. Note that the pocks, although varying somewhat in size, all resemble each other in appearance. The rash is now so characteristic that there should be no mistake in diagnosis. Smallpox Cycle • During days 8 and 9, the pustules increase somewhat in size. They are firm to the touch and deeply embedded in the skin. Smallpox Cycle • Gradually the pustules dry up and dark scabs form. The scabs begin to appear between 10 and 14 days after the rash first develops. The scabs contain live smallpox virus. Until all scabs have fallen off, the patient may infect others. Smallpox Cycle • By day 20, the scabs have come off and lightcoloured or depigmented areas are observed. The skin seldom returns to its normal appearance. Scars which last for life, often remain (especially on the face). Such scars are an indication of previous infection with smallpox. • Smallpox had two main forms: – Variola Major – Variola Minor. • The two forms showed similar lesions. The disease followed a milder course in variola minor, which had a case-fatality rate of less than 1%. • The fatality rate of variola major was around 30%. • There are two rare forms of smallpox: – Hemorrhagic – Malignant. • Hemorrhagic is invariably fatal, the rash is accompanied by hemorrhage into the mucous membranes and the skin. • Malignant smallpox is characterized by lesions that did not develop to the pustular stage but remained soft and flat. • It was almost invariably fatal. • Smallpox is transmitted from person to person by infected aerosols and air droplets spread in face-to-face contact with an infected person after fever has begun, especially if symptoms include coughing. • The disease can also be transmitted by contaminated clothes and bedding, though the risk of infection from this source is much lower. • Ro = 5 to 7 from an Index Case Ro = Reproductive Ratio • When – Ro < 1 • the infection will die out in the long run (provided infection rates are constant). But if – Ro > 1 • the infection will be able to spread in a population. Large values of R0 may indicate the possibility of a major epidemic. Values of R0 of well-known infectious diseases Desease Mode of Transmission Measles Airborne Pertussis Airborne droplet Diphtheria Saliva Smallpox Social contact Polio Fecal-oral route Rubella Airborne droplet Mumps Airborne droplet HIV/AIDS Sexual contact SARS Airborne droplet Influenza (1918 Strain) Airborne droplet Ro 12–18 12–17 6–7 5–7 5–7 5–7 4–7 2–5 2–5 2-3 Smallpox Vaccine • Edward Jenner's demonstration, in 1798, that inoculation with cowpox could protect against smallpox brought the first hope that the disease could be controlled. • “Pox Type” Virus • Live Virus Vaccine • Reactions Vary to Vaccine • 15-52 Persons Experience Severe Reactions • 1-2 People will Die • Bifurcated (TwoPronged) Needle Accidental autoinoculation of cheek with vaccine virus, approximately 5 days old. Primary take on arm, 10-12 days old. Accidental auto-inoculation of eyelid with vaccine virus West Nile Virus West Nile virus was first isolated from a febrile adult woman in the West Nile District of Uganda in 1937. WNV • • • • • • • Mosquito-borne Virus Causes Encephalitis or Meningitis Bird Mosquito Horse or Man No Treatment No Human Vaccine 1% Case Fatality Rate Epidemiologists Use Sentential Surveillance Transmission Cycle of West Nile Virus Horses and Humans are Accidental Dead End Hosts Mosquito to Bird Bird to Mosquito 1999 – 25 Cases 2000 – 60 Cases 2001 – 738 Cases 2002 – 15,257 Cases 2003 – 5,181 Cases Hantavirus Hantavirus • Fatigue, Fever, Muscle Aches • Lungs Fill with Fluid • Respiratory Failure • Cardiac Failure • 1990’s in Four Corners N.M. • Virus Shed in Mouse Droppings • No Treatment, No Cure • No Vaccine / High Case Fatality Hemorrhagic Fevers • • • • Ebola Denge Lassa Marburg Ebola Transmission? • Researchers do not know exactly how Ebola is spread. However, they have strong reason to believe that the first patient becomes infected through contact with an infected animal. • The Ebola virus is then spread from human to human by: 1. direct contact with the blood and/or secretions of an infected person. 2. contact with objects (fomites), such as needles, that have been contaminated with infected secretions. Volunteers in protective clothing remove the infected bodies and disinfect the houses to prevent the spread of Ebola. Ebola – Level 4 CDC Outbreak—Ebola “Odoch Walter [seated], 21, was vomiting blood. An ambulance driver is spraying him before he puts him in the vehicle. In case he did have Ebola, they were trying to keep him and the ambulance ‘clean.’ “To be sprayed like that in the face, by this person who’s completely covered in plastic and rubber and treats you as a threat to their life—it’s all pretty horrible. He died two days later.” “At Lacor Hospital, the head nurse and Matthew Lukwiya, a doctor, are looking out at nurses who are grieving coworkers who’ve died. They’re terrified to go back into the hospital because of the virus. Lassa Fever • • • • • • Acute Viral Illness / West Africa / 1969 Endemic in Africa 50% Case Fatality Rate / Deafness Multimammate Rat is Reservoir Aerosolized Rodent Urine and Droppings Fever, Pain in Chest, Back Pain, Cough, Abdominal Pain, Vomiting, Diarrhea, Facial Swelling, Bleeding from all Mucosal Membranes • No Treatment, No Vaccine Dengue Hemorrhagic Fever • Mosquito-borne / Aedes Mosquito • Tropical and Sub-Tropical Regions • 1950’s Epidemics in Philippines and Thailand / Today Asia • 2/5 of World’s Population at Risk • 50 Million Cases Yearly • 50% to 90% Exposed Become Diseased • Case Fatality Rate 20% • Flu-Like Disease / Photophobic/ Hemorrhagic Phenomena / Liver Enlargement Resulting in Circulatory Failure • No Treatment / No Cure / No Vaccine Marburg Fever • Marburg Virus Disease, and previously also known as green monkey disease due to its primate origin. Also found in Fruit Bats in some areas. • Marburg originated in Central and East Africa, and infects both human and nonhuman primates. • The disease is spread through bodily fluids, including blood, excrement, saliva, and vomit. Bioterrorism? • The two viruses considered to be the greatest bioterrorism threats are Ebola and Marburg, the two members of the filovirus family, which are categorized as category A bioweapon agents. These viruses characteristically cause high mortality and morbidity, are person to person spread, are highly infectious at a low dose by the aerosol route, are stable in the environment, and large-scale production is feasible. Cold or Influenza If you have: Do you have a cold? Or Influenza? Fever Probably not Likely - Especially if it’s high Headache Probably not Likely Body Aches If they are minor Likely - If they are severe Fatigue If it is mild Likely – Exhaustion Sneezing Probably so, if no fever Possibly, if with fever Stuffy Nose Probably so, if no fever Possibly, if with fever Sore throat Probably so, if no fever Possibly, if with fever Cough If it is mild Possibly - If it is severe Chickenpox 1. Varicella 2. Very Contagious 3. Shingles Later in Life 4. Infectious From 1 Day Before Rash till 5 Days After Rash Appears 5. Body, Throat, Mouth, Ears 6. Encephalitis / Pneumonia Chickenpox Classic case of chickenpox of the newborn Chickenpox, hemorrhagic Infant with necrotizing fasciitis, a complication of varicella Secondary Staph Infection in Chickpox lesions Confused with Smallpox? Shingles • Shingles (sometimes called herpes zoster) is a painful, blistering skin rash due to the varicellazoster virus, the virus that causes chickenpox. • After you get chickenpox, the virus remains inactive (becomes dormant) in certain nerves in the body. Shingles occurs after the virus becomes active again in these nerves years later. • Risk Increases If: 1. You are older than 60 2. You had chickenpox before age 1 3. Your immune system is weakened by medications or disease Roseola • 6 Months to 2 Years • 1 Week Duration • High Fever • Irritability • Sore Throat / Runny Nose • Swollen Lymph Nodes • Can Trigger Febrile Seizures • Encephalitis Other Symptoms • bulging of the fontanel, or soft spot, in the head of an infant • cough • mild diarrhea • mild sore throat • puffy eyelids • runny nose Rubeola (Measles) • Measles is a highly contagious - but rare respiratory infection that's caused by a virus. It causes a total-body skin rash and flu-like symptoms, including a fever, cough, and runny nose. • May see Koplik’s Spots in Mouth Koplik’s Spots small, white spots (often on a reddened background) that occur on the inside of the cheeks early in the course of measles. Rubella / German Measles / 3 Day Measels • Rubella — commonly known as German measles or 3-day measles — is an infection that primarily affects the skin and lymph nodes. • It is usually transmitted by droplets from the nose or throat that others breathe in. • It can also pass through a pregnant woman's bloodstream to infect her unborn child. • A generally mild disease in children, the primary medical danger of rubella is the infection of pregnant women, which may cause congenital rubella syndrome in developing babies. Maternal Infection • In the first 12 weeks of pregnancy results in birth defects in up to 85 percent of cases • From 13 to 16 weeks of gestation results in birth defects in 54 percent of cases • At the end of the second trimester results in birth defects in 25 percent of cases Complications • Miscarriage • Stillbirth • • • • Blindness Deafness Heart Abnormalities Mental Retardation Polio Polio • • • • Virus Shed in Feces 1950’s Closed Swimming Pools 95% Unapparent Infections 4% to 8% Minor Illness / Respiratory Infections with Complete Recovery • 1% to 2% Result in Aseptic Meningitis with Stiff Neck, Back and Legs Involved with Complete Recovery • <2% Result in Permanent Partial Paralysis or Death Iron Lungs • The iron lung was the first effective treatment for patients paralyzed by polio that couldn't breathe. • The first model consisted of a tank and a pair of vacuum cleaner blowers. • Because patients lived inside the respirators for weeks, months or even years at a time, later models had portholes through which clinicians could give care. • The respirator shown here was used in the early 1930s. Los Angeles Polio Ward with Iron Lungs in Use 1952 Two children with polio receiving physical therapy The Salk vaccine, was developed by Dr. Jonas Salk in 1952. Kurt Achenbach, 7, a first-grader in 1954, bucks up his courage for his polio immunizatoin. Kurt was one of 1.8 million “polio pioneers” who volunteered to test the Salk vaccine. Aerial view of a crowd awaiting polio immunization, San Antonio, 1962 Did You Know? • When the first, injectable polio vaccine was tested on some 1.8 million children in the United States in 1954, within 9 days there was huge epidemic of paralytic polio in the vaccinated and some of their parents and other contacts. The US Surgeon General discontinued the trial for 2 weeks. Oral vaccine prevents the vaccinee from acting as a carrier of wild type poliovirus, and as stated, confers long-lasting immunity. The OPV is also easily administered by giving children a sugar cube or sugar liquid containing the vaccine, neither of which requires extensive medical training to be administered. This 1963 poster featured CDC’s national symbol of public health, the "Wellbee", encouraging the public to receive an oral polio vaccine. Chronic Fatigue Syndrome • As immunization with the Salk vaccine got underway the polio epidemics came to a halt, and in 1979, the disease was declared eradicated in the U.S. But the polio story isn't over. Some 70 percent of survivors now suffer from postpolio syndrome, or weakness in previously unaffected muscles. Hot Spots Still Exist • Today about the only polio we see in the United States is in children adopted from other countries. Herpes • Herpes is a general term for two different diseases: one that affects the area around the mouth (oral herpes, also known as cold sores) and another that affects the area around the genitals (genital herpes). Herpes • Two Kinds 1. HSV Type 1 - Fever Blisters and Cold Sore - Genital Herpes - 50% to 80% Americans Carry Antibodies 2. HSV Type II - Usual Cause of Genital Herpes Congenital Herpes • Herpes cannot be cured. • Once either virus is inside the body and settles itself into the nerve cells, it cannot be eliminated. However, herpes sores can be treated. • Treatment can speed up healing time, reduce pain, and delay or prevent additional flare-ups. Typically, treatment is used only during a flare-up. HIV / AIDS "One of the most recognized AIDS posters every produced" USA, 1987 2007 1970-1980 • We do not know how many people developed AIDS in the 1970s, or indeed in the years before. Neither do we know, and we probably never will know, where the AIDS virus HIV originated. But what we do know is: • "The dominant feature of this first period was silence, for the human immunodeficiency virus (HIV) was unknown and transmission was not accompanied by signs or symptoms salient enough to be noticed. 1981 • Kaposi's Sarcoma (KS) was a rare form of relatively benign cancer that tended to occur in older people. • At about the same time there was an increase, in both California and New York, in the number of cases of a rare lung infection Pneumocystis carinii pneumonia (PCP)3. • "A doctor was treating a gay man in his 20s who had pneumonia. Two weeks later, he called to ask for a refill of a rare drug that I handled. This was unusual-nobody ever asked for a refill. Patients usually were cured in one 10-day treatment or they died" 1982 • We definitely had a new disease that was linked to it's initial occurrence in gay men, with the Lancet calling it the 'gay compromise syndrome', whilst at least one newspaper referred to it as GRID (gay-related immune deficiency) and another as “gay cancer.” • In June a report of a group of cases amongst gay men in Southern California, suggested that the disease might be caused by an infectious agent that was sexually transmitted. August 1982 • By August the disease was being referred to by it's new name of AIDS24. The word AIDS was an abbreviation of Acquired Immune Deficiency Syndrome. • " When it began turning up in children and transfusion recipients, that was a turning point in terms of public perception. Up until then it was entirely a gay epidemic, and it was easy for the average person to say 'So what?' Now everyone could relate.“ Harold Jaffe of the CDC for newsweek -34 1983 • Evidence emerged that men could pass the disease on via heterosexual transmission to women. • The sense of urgency was greatest for haemophiliacs • In May 1983, doctors at the Institute Pasteur in France reported that they had isolated a new virus, which they believed was the cause of AIDS. HIV Ward in Thailand AIDS claims so many lives that orphanages are set up for the children of the victims. Picture from Ethiopia. Early Posters / Informative Then Posters Moved to Getting the Point Across in a Few Words Today Forget Being Politically Correct Let’s Just Save Lives "During the early years of the epidemic, there was a great deal of fear over the transmission of HIV. This even extended to sharing the chalice during communion in church. The Terrence Higgins Trust produced this poster to try and quell any fears that people had." UK, 1986 HIV / AIDS • Acquired immune deficiency syndrome or acquired immunodeficiency syndrome (AIDS or Aids) is a collection of symptoms and infections resulting from the specific damage to the immune system caused by the human immunodeficiency virus (HIV) in hu.mans • The late stage of the condition leaves individuals susceptible to opportunistic infections and tumors. • Although treatments for AIDS and HIV exist to decelerate the virus progression, there is currently no known cure. • HIV, et al., are transmitted through direct contact of a mucous membrane or the bloodstream with a bodily fluid containing HIV, such as blood, semen, vaginal fluid, preseminal fluid, and breast milk. HIV / AIDS • UNAIDS estimates that 36.9 million people were living with HIV/AIDS worldwide as of the end of 2007. • Since the epidemic began, an estimated 21.8 million people have died of AIDS • 100% Case Fatality Rate • >75% of all individuals with AIDS are male. • Acquired Immune Deficiency Syndrome • Incubation Period of 5-10 Years • Increase in TB, Pneumonia, Persistent Severe Diarrhea, Skin Infections, Cancer, etc. • 13-20 Million People Infected with HIV • No Vaccine, No Cure, Drug Therapy Does Exist • STD / Needles / Body Fluid Exchange