* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Lecture 3 LRC
Remote ischemic conditioning wikipedia , lookup
Electrocardiography wikipedia , lookup
Cardiovascular disease wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Heart failure wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Jatene procedure wikipedia , lookup
Cardiac surgery wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
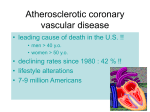
MEDICAL EMERGENCIES Lecture 3 Objectives Recognize Medical Emergencies Explain protocol to handle medical emergencies Be able to follow emergency management protocol Describe how to manage the patient experiencing a medical emergency Discuss Angina Pectoris, Myocardial Infarction, Heart Failure and Acute Pulmonary Edema Objectives List specific signs and symptoms associated with CVA Explain the steps needed to prepare an office for a patient experiencing CVA Describe the procedure for the management of dental patient experiencing Myocardial Infarction, Cardiac Arrest, Acute Pulmonary Edema and Heart Failure in the dental setting Objectives List signs and symptoms associated with pacemaker and ICD malfunction Explain the special precautions that should be taken to prevent a patient from experiencing a pacemaker or ICS malfunction Introduction Coronary artery disease (CAD): also called coronary heart disease: most often the cause of chest pain originating in the heart. Results in the greatest number of deaths per year. A medical history is critical prior to the initiation of any dental treatment. RDH should be able to identify risk factors for CAD. Chances of survival increases if emergency procedures are activated at the onset of symptoms. 4-14 Risk factors for CAD Atherosclerotic heart disease = CAD Atherosclerosis is a slow, complex inflammatory arterial disease that starts in childhood and progresses with age. Major risk factor in the development of all forms of cardiovascular disease and is most likely the cause of myocardial ischemia. Starts when the inner lining of an artery is injured or damaged by: high cholesterol, tobacco, diabetes, high BP, infectious microorganisms. 4-14 Coronary artery disease (CAD) Atherosclerosis characterized by a buildup of yellowish plaques on the inner walls of arteries. The plaque is composed of cholesterol, lipids, platelets, calcium, and cellular debris. As the plaque size increases, it starts to restrict blood flow and oxygen to the heart and brain. Closing off an artery or occlusion of an artery can result in silent ischemic episodes, angina pectoris, acute myocardial infarction (AMI), or strokes. 4-14 Atherosclerosis 4-14 Risk factors for CAD: Gender Historically considered to affect males more than females However, CAD and stroke is the leading cause of death among women in the US. Diabetes, high cholesterol- increased risk of CAD in women more than in men. Post-menopausal women higher risk for CAD than premenopausal women. Hormone replacement therapy may reduce risk. 4-14 Risk factors for CAD: Age Increasing age in men and women increases the risk of developing CAD. New onset CAD occurs after 65 yrs of age. Modifying risk factors or the prevention of developing risk factors directed to the age groups between 65-75. 4-14 Heredity Including Race Family history of premature CAD, high blood pressure, high cholesterol. Patients with a family history of premature heart disease is at a higher risk. African Americans have the highest CAD mortality rates. Non-Hispanic whites have the 2nd highest mortality rates followed by Hispanics, Native Americans, and Asians. African American women have a higher CAD mortality rate compared to non-Hispanic women. 4-14 Tobacco Use Smokers 2-4 times more like to develop CAD than non-smokers. Smoking is a major independent risk factor for sudden cardiac death in patients with CAD. Smoking accelerates the development of coronary plaques and promotes plaque rupture and coronary thrombosis. Tobacco cessation quickly and significantly reduces the risk for a heart attack. Cigarette smoking is the most preventable cause of death in the US. 4-14 Hypertension Individuals over the age of 50 with a systolic BP greater than 140 mmHg is a more important risk factor in the development of cardiovascular disease than diastolic blood pressure. Dental professionals will encounter patients who have undiagnosed or uncontrolled BP. Referral to a MD may be necessary prior to treatment. Always take and record BP and vitals at every appointment. 4-14 Hypercholesterolemia High Cholesterol – waxy, fat-like substance made in the liver. Found in foods derived from animals including meat, dairy, eggs, cheese, and milk. A small amount of cholesterol is needed to help digest fat. Cholesterol attaches to a lipoprotein and is carried throughout the bloodstream. Too much cholesterol results in atherosclerosis and CAD. 4-14 Lipoproteins Low-density lipoprotein (LDL): cause atherosclerosis. Optimal levels are less than 100 mg/dL. 160-189mg/dL are considered high High-density lipoproteins (HDL): help rid the body of LDLs. High levels of HDLs prevent CAD. Triglycerides: another form of fat found in the bloodstream. Increased levels of 150-200mg/dL or > may increase the risk for CAD 4-14 4-14 Diabetes Most common complication of diabetes type I and II is cardiovascular disease due to atherosclerosis and hypertension. Atherosclerosis in diabetics is accelerated and more severe. Macroangiopathy: is the damage done to the large blood vessels in diabetics as a result of atherosclerosis. Microvascular damage due to hyperglycemia diminshes vascular function making the consequences of atherosclerosis and hypertension more difficult to withstand. 4-14 Macroangiopathy: narrowing of the arteries 4-14 Obesity and Physical Activity Obesity and lack of physical exercise negatively impact CAD due to their effect on major risk factors. Obesity often results in Type 2 Diabetes. Weigh control, diet, and exercise can reduce hypertension and hypercholesterolemia 4-14 Angina Pectoris Chest pain due to angina is one of the more common medical emergencies in the dental office. Angina due to inadequate supply and/or increased demand for oxygen to the myocardium (myocardial ischemia). Clinicians should be aware of the patient’s whose medical hx indicate past incidences of angina. CAD, presenting as angina or AMI, is the leading cause of sudden death in the US. 4-14 Angina Pectoris As plaque deposits increase in size they restrict the opening of the artery= atherosclerosis Occlusion of the artery can result in an infarction Common medical emergency in dental office Forms of Angina Stable Unstable Variant (Prinzmetal’s) 4-14 Signs and Symptoms of Stable Angina Generalized chest discomfort: pressure, burning, heaviness, squeezing, or choking** Radiates from thoracic area to left shoulder, down the arm, and to the neck, lower jaw, or tongue. Patient may present symptoms such as diaphoresis or a cold sweat, nausea and pallor. Attacks can vary in intensity; lasting from 1 to 15 minutes. 4-14 Stable Angina AKA typical, chronic, classic, exertional Usually related to CAD and is the most common form of angina. Usually induced by physical activity or stress and symptoms are worse in cold weather or after a large meal. May radiate to shoulders, arms, neck, mandible, or epigastric.** Pain associated with a pressing feeling, crushing, burning, or squeezing.** Usually discomfort in left area of chest lasting from 1-15 minutes. 4-14 Stable Angina Stable angina responds to rest and nitroglycerine within 10 to 15 minutes. Angina considered stable if there has been no change in frequency, etiology, or duration of symptoms in last 60 days. Can receive dental care – appointments should be short and minimally stressful. Medications for angina: calcium channel blockers, nitrates, and beta-adrenergic blocking agents. Regular exercise reduces frequency of symptoms and increases functional capacity of the heart 4-14 Signs and Symptoms of Stable Angina In acute anginal episodes, pts may be apprehensive and may press their fist to their sternum called the Levine sign. Pts may have an increase in HR and BP. 4-14 Levine sign 4-14 Prevention of an Anginal Episode A complete, comprehensive medical history to identify patients who may be at risk for or have CAD. Patients with unstable angina (UA) should only get Tx if ok by physician. Do not use vasoconstrictors. Patients with stable angina can be tx in the office, but the emotional, environmental, and physical stresses of the dental appt may cause an anginal episode. Modify dental tx to reduce stress: shorter appt times and end tx when pt starts to show signs of fatigue, stress, or anxiety. Schedule patients for late morning or afternoon appts. 4-14 Prevention Local anesthetics containing a vasoconstrictor on a pt with stable angina is generally not contraindicated; but the max dosage of epi for a cardiac-risk pt is .04mg. Which amounts to approx 2 cartridges of anesthesia containing 1:100,000 epi. Pts treated with b-adrenergic blockers for management of angina should not be given vasoconstrictors. Pts with unstable angina should NOT receive local anesthetics with vasoconstrictors. 4-14 Prevention Angina pts may benefit from supplemental oxygen at a flow rate of 3-5 L/min via nasal cannula. Minimizes the risk of inadequate oxygenation of the myocardium during treatment. Have pts bring their own nitroglycerin spray or tablets to the dental appt. Better to use pts Rx because the dosage will be correct for the pt. Medical ER kit should contain nitroglycerin (nitrolingual spray) preferred because it is more stable than tablets. 4-14 Treatment of Angina Terminate treatment Semi-supine or upright position Assess ABC’s Administer oxygen, 3-6L/minute Monitor vital signs Administer sublingual or transmucosal nitroglycerine – dilates coronary blood vessels resulting in decreased cardiac workload Treatment of Angina Use patient’s own medication if current Will feel tingling sensation on tongue if fresh Administer one table every 5 minutes up to 3 doses – usually alleviates symptoms in 2-4 minutes Nitro contraindicated in hypotensive patients Treatment of Angina Following administration of nitroglycerine, patient may experience tachycardia, flushing, pounding in head, hypotension. Nitroglycerine is not effective if it is expired or if patient is experiencing an acute heart attack. If pts pain is more severe than previously experienced, EMS should be called immediately. If pt has no known history of angina and chest pain lasts for 2 minutes or longer, call 911 immediately. 4-14 Figure 10.3 Nitroglycerin Figure 10.2 Anginal patient with nasal cannula to deliver oxygen Figure 10.4 Blockage of coronary arteries Heart Attack 4-14 Acute Myocardial Infarction (AMI) Necrosis of a portion of the myocardium due to total or partial occlusion of a coronary artery. Occlusion caused by atherosclerosis, thrombus, or a coronary spasm. May form rapidly or over a period of time. MI can lead to cardiac arrest: when the heart fails to beat. Providing basic life support prior to EMS arriving could save a life. 4-14 Acute Myocardial Infarction (AMI) Cardiac dysrhythmia may occur after MI and is a high risk for death Dysrhythmia may present as: ◦ Bradycardia: slow heart rate ◦ Ventricular tachycardia – rapid contraction with inadequate ventricular filling ◦ Ventricular fibrillation – disorganized, irregular contraction of ventricles ◦ Asystole – absence of heart contractions 4-14 Signs and Symptoms of AMI Classic symptom: chest pain lasting 20 minutes or longer** Pressure, tightness, heaviness, burning, squeezing, crushing sensation in middle of chest and/or lower 1/3 of epigastrium Pain may radiate down arms, shoulders, jaw, or back.** Pt may also experience weakness, dyspnea, diaphoresis and an irregular pulse. If pain is intense, pt may have nausea and vomiting. 4-14 Signs and Symptoms of AMI Pts may feel a sense of impending doom, clutching their fist to their chest (Levine Sign). Women show different symptoms: indigestion, back pain, breathlessness, back pain, deep throbbing in left or right bicep or forarm.** Diabetics suffer silent MIs. The elderly show signs of shortness of breath, dizziness, pulmonary edema, and/or an altered mental status or an arrhythmia. Always important to treat chest pain as cardiac related until a cardiac cause can be ruled out. Pg.105, Table 10.4 4-14 Treatment of AMI ** Stop hygiene treatment, alert staff and dentist, call EMS. Place patient in a comfortable position. Monitor vitals Administer high-flow oxygen and BLS. Patient can take one nitroglycerin tablet every 3-5 minutes, no more than 3 doses in a 15 minute time period. 4-14 Treatment of AMI Initiate fibrinolysis: breaking down of fibrin, part of a process designed to dissolve a clot or prevent a clot from forming. Administer aspirin chewed 325 mg. – antithrombotic effect – clinical effect reached in 20 minutes. Aspirin should be chewed to enter bloodstream quicker. Make sure the patient is not allergic to aspirin. Manage pain to prevent cardiogenic shock with nitrous oxide, if available. If cardiac arrest occurs, perform CPR with AED. According to the AHA, the immediate initiation of CPR and use of AED within the first 3-5 minutes, pts have the highest chance for survival. 4-14 Figure 10.5 Baby aspirin for anticoagulation Heart Failure Occurs when heart muscle is impaired and no longer pumps sufficient blood to body tissues and organs Can result from almost any kind of CVD Congestive heart failure now called heart failure by the American Heart Association due to the broad spectrum of the disease 4-14 Heart Failure MI and hypertension most frequent etiology Can be associated with other underlying factors Initially presents during exertion As disease progresses symptoms occur even when at rest Heart Failure 3 cardinal symptoms of HF: dyspnea, edema, and fatigue; though not necessarily diagnostic of HF. Symptoms of HF initially start during exertion, as disease progresses shortness of breath and fatigue are present even when pt is at rest. Physiological and/or psychological stress with dental tx can exacerbate symptoms. Could lead to life-threatening acute pulmonary edema. Very important for clinician to recognize signs and symptoms, know how to modify and manage dental tx, and be prepared to respond to a medical emergency. 4-14 Clinical Manifestations of Heart Failure Left ventricular HF Right ventricular HF Both left and right ventricular HF 4-14 Figure 11.2 Left-side and right-side heart failure The Heart Left atrium collects newly oxygenated blood from the lungs and the left ventricle pumps the oxygen-rich blood out to the body. Right atrium collects oxygen-poor blood from the body, the right ventricle pumps it to the lungs where the blood picks up oxygen and gets rid of carbon dioxide. Heart failure can be classified according to the side of the heart that is affected. Long term heart failure usually involves both sides. Pg. 115, figure 11.2 and pg.114, figure 11.1 4-14 4-14 Signs and Symptoms of Left Heart Failure Cardiac asthma – wheezing due to congestion of bronchial mucosa Pale and cool to touch Diaphoresis Increased BP Pulse rapid and thready – may alternate between strong and weak LV failure usually occurs before RV failure. Signs and Symptoms of Left Heart Failure Heart failure patients with moderate to severe breathing difficulty are classified as ASA III or IV. Often require supplemental oxygen via nasal cannula. Dental tx must be modified: shorter appt times, placing the pt in an upright position during treatment, a standing prophy. LV pts may also cough due to congestion in the lungs; a dry, nonproductive, chronic cough occurring with dyspnea and during exertion or lying in a supine position. 4-14 Signs and Symptoms of Right Heart Failure Usually develops after left heart failure. Causing the effect of increased fluid pressure ultimately damages the right side of the heart. RV failure results in the inability of the heart to pump oxygen-poor blood from the systemic venous circulation to the lungs for oxygenation. Results in congestion in systemic venous system. RV pts feel: fatigue and weakness. Classic symptom – peripheral edema. Pitting edema in lower legs and ankles, a depression that remains in the tissue for a few seconds after release of pressure to the area. 4-14 Signs and Symptoms of Right Heart Failure Reduction in renal blood flow resulting in a decrease in the excretion of sodium, so causes the retention of fluids. ◦ During the day patient’s activity increases degree of HF – less urine production ◦ At night – less active – renal and cardiac function may improve ◦ Nocturia may result – increased urination at night Distended external jugular veins while lying or sitting. Normally the jugular veins are collapsed while standing or sitting. 4-14 Signs and Symptoms of Right Heart Failure In RV heart failure, engorgement of the liver and spleen occurs. As the disease progresses, edema in the abdomen becomes evident. Congestion in the gastrointestinal tract can cause nausea, vomiting and anorexia. Edema in the central nervous system can manifest clinically with pt experiencing headaches, insomnia, and irritability. Pg 117, Table 11.1 4-14 Signs and Symptoms of Later Stages of Heart Failure Mental confusion, anxiety, and restlessness due to the lack of O2 to brain. Cardiac cachexia: malnutrition and wasting of tissues; may be evident in end-stage HF. Cyanosis of the skin and mucous membranes, especially in the nail beds and lips; also a sign of late-stage HF. 4-14 Treatment of Heart Failure Changes in lifestyle can lessen the symptoms of HF and prevent the disease from progressing. ◦ Smoking cessation, exercise, weight loss, diet low in fat and sodium, limited caffeine and alcohol, and stress reduction. ◦ Drug therapy differentiated between systolic and diastolic dysfunction. ◦ Diastolic dysfunction: the underlying cause of impaired diastolic function determined prior to drug therapy. 4-14 Treatment of Heart Failure Drug therapy ◦ ACE inhibitors ◦ Diurectics ◦ Vasodilators ◦ Beta blockers ◦ Calcium channel blockers Management of Heart Failure Patient in Dental Setting Questions ◦ Heart failure ◦ Swelling in feet or ankles ◦ Shortness of breath ◦ Weight gain – 3 pounds over 7 days with edema red flag – postpone treatment Management of Heart Failure Patient in Dental Setting Physical characteristics observed ◦ Cyanosis ◦ Jugular veins Vital signs prior to treatment and throughout appointment Management of Heart Failure Patient in Dental Setting ASA IV (dyspnea, orthopnea, and fatigue at all times) require medical consultation ◦ Elective treatment should be postponed until symptoms controlled Acute Pulmonary Edema Most dramatic life-threatening symptom of HF. Acute pulmonary edema is the result of a swift and abrupt accumulation of fluid in the alveolar spaces in the lungs inhibiting lung expansion and results in the decreased ability for the lungs to oxygenate the blood. Precipitating events ◦ Stress ◦ Infection ◦ Failure to take medications as prescribed ◦ Meal high in sodium 4-14 4-14 Signs and Symptoms of Acute Pulmonary Edema Gasping for air Rapid pulse Cool, moist skin Cyanotic lips and nail beds Anxiety Dyspnea with cough that may produce frothy, blood tinged sputum Loud coarse lung sounds Treatment of Acute Pulmonary Edema in the Dental Setting Life threatening Contact EMS Terminate all treatment Reduce patient anxiety to reduce cardiac and respiratory workload Position patient comfortably – probably upright to aid in breathing ABC’s Treatment of Acute Pulmonary Edema in the Dental Setting O2 10 L/minute or more Monitor vital signs every 5 minutes Nitroglycerine 2-3 tablets or sprays every 5 -10 minutes ◦ Do not use if systolic BP below 100 mmHg If consciousness lost, place in supine position and administer CPR Treatment of Acute Pulmonary Edema in the Dental Setting Maintaining the airway and breathing is the primary concern. Clinician can perform a bloodless phlebotomy using BP cuffs placed 6 inches below the groin and one 4 inches below the shoulder. One BP cuff should be removed every 5-10 minutes and reapplied to the other free extremity. Cuff should be tight enough to reduce blood flow but loose enough to feel the arterial pulse. This tx can temporarily remove blood from circulation, allowing the heart to pump the remaining blood more effectively. Resulting in reduced pulmonary congestion and improved breathing. 4-14 Figure 11.3 Bloodless phlebotomy Managing acute pulmonary edema Nitroglycerin can be given for a rapid treatment of pulmonary edema and heart failure. Morphine may be administered for patients experiencing apprehension and anxiety; increase in vasodilation, decrease in cardiac and respiratory work load. Pts with hypoxia with cyanosis, mental confusion, or delirium, the use of opioids is an absolute contraindication. In the dental office, staff would be only administering oxygen and allowing pt to sit upright to reduce respiratory distress. Cardiac Pacemaker Composed of pulse generator and leads Generator contains electronic circuitry that powers device Figure 12.1 Pacemaker Figure 12.2 Area of pacemaker Cardiac Pacemaker Used for arrhythmias Usually bradycardia leading to low cardiac output Pacemaker monitors heart rate Implantable Cardiac Defibrillator Similar device to pacemaker Used to treat harmful tachyarrhythmias (200 BPM) which usually originate in ventricles Pacemaker or ICD Malfunction All patients with pacemaker or ICD should have medical consultation prior to dental treatment Small chance of infective endocarditis Rarely is premedication recommended Greater risk of malfunction with electromagnetic interference Pacemaker or ICD Malfunction Possible etiologies of malfunction ◦ Cellular phones ◦ MRI Should be informed by physician Should carry a card Pacemaker or ICD Malfunction in Dental Office Safe procedures ◦ Radiographs ◦ Handpieces ◦ Curing lights ◦ Sonic and piezoelectric scaler Possibly unsafe procedures ◦ Older ferromagnetic ultrasonic scalers ◦ Magnetostrictive ultrasonic scalers ◦ TENS Pacemaker or ICD Malfunction in Dental Office Possibly unsafe procedures Older ferromagnetic ultrasonic scalers Magnetostrictive ultrasonic scalers TENS Units Ultrasonic baths Electrosurgical units Sonic toothbrushes – Vasoconstrictors in local anesthetics, use with caution Pacemaker or ICD Malfunction Electrical interference is interpreted by pacemaker or ICD as electrical activity and may inhibit function. Situation is temporary and does not cause permanent damage to the pacemaker. Extent of the malfunction depends on the strength, duration, and type of interference. Pacemakers and ICDs are protected from interference by shielding the circuitry inside a stainless steel or titanium case, signal filtering, interference rejection circuits, noise reversion functions and programmable parameters. 4-14 Figure 12.3 Magnetostrictive ultrasonic scaler contraindicated in pacemaker and ICD patients Figure 12.4 Ultrasonic bath contraindicated in close proximity to pacemaker and ICD patients Figure 12.5 Use of lead apron with pacemaker and ICD patients Figure 12.6 Appropriate distance of sonic toothbrush with pacemaker with ICD patients Signs and Symptoms of Pacemaker Malfunction Lightheadedness Dizziness Dyspnea Moist, pale skin Weakness Bradycardia or tachycardia Chest pain Swelling of extremities Signs and Symptoms of ICD Malfunction Inappropriate defibrillation Twitching Biting Sudden movements Treatment of Pacemaker or ICD Malfunction Turn off interference Assess level of consciousness If conscious ◦ Monitor vital signs ◦ Monitor pulse rate to determine if it has reverted to normal rhythm ◦ If rhythm is not normal – contact EMS for transport to ED Treatment of Pacemaker or ICD Malfunction If unconscious ◦ Treat for syncope ◦ Monitor vital signs ◦ If consciousness not regained – contact EMS for transport to ED Dallas! 4-14