* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download PEARLS IN CARDIOLOGY
Remote ischemic conditioning wikipedia , lookup
Heart failure wikipedia , lookup
Cardiovascular disease wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Electrocardiography wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Coronary artery disease wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Cardiothoracic surgery wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
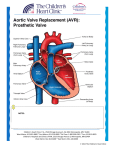
Aortic stenosis wikipedia , lookup
PEARLS IN CARDIOLOGY Sandra Rodriguez Internal Medicine 2008 Jugular venous Pulse “a” is RA contraction “c” is bulging of TV during RV systole. “x” downward displacement of TV. “v” is atrial filling at systole, TV closed. “y” is passive atrial emptying. Jugular Venous Pulse Giant “a” wave: Tricuspid stenosis Pulmonary stenosis Pulmonary hypertension Canon “a” wave: (against a closed valve): Junctional rhythm Slow ventricular tachycardia 2:1 A-V block Bigeminy Absent “a” wave: Atrial Fibrilation Jugular Venous Pulse Prominent “x” descent: Cardiac tamponade Constrictive pericarditis Absent “x” descent: RV infarction Prominent “v” wave: Tricuspid regurgitation Prominent “y” descent: Constrictive pericarditis Slow “y” descent: TS and RA mixoma. Absent “y” descent: Cardiac tamponade RV infarction Prominent x and y: Constrictive pericarditis Prominent x and absent y: Cardiac tamponade Absent x and y: RV infarct. Questions 1. A 34 year-old patient is on Ma Huang for losing weight. She presents with shortness of breath. EKG shows wide complex tachycardia. HR is 140/min. Cannon “a” waves are present. Cause? a. Sinus tachycardia with WPW b. Sinus tachycardia with aberrant conduction c. Atrial fibrilation with aberrant conduction. d. Ventricular tachycardia. Murmurs With inspiration: R side murmurs increase, L side decrease. With standing: HCM and MVP get louder. With squatting or passive leg raising: HCM and MVP become softer and delayed. With valsalva: HCM and MVP get louder and longer. With amyl nitrite inhalation (decreases LV cavity): AR, MR and VSD decrease while those of HCM and AS increase. With exercise (hand grip): HCM and AS decrease. With standing, valsalva, and inhalation of amyl nitrited (all decrease venous return or LV cavity size): Murmurs of HCM and MVP increase in intensity. All others decrease. With isometric exercise and squatting (all increase LV cavity size): Murmur of HCM is decreased. With isometric exercise and valsalva: Murmur of AS is decreased in intensity. Questions 2. Murmur of which of the following increases with valsalva and decreases with squatting: a. Mitral Regurgitation. b. Hypertrophic cardiomyopathy (HCM) c. Aortic stenosis 3. What happens to the murmur of AS with valsalva and hand-grip exercise? a. Increase, decrease b. Decrease, decrease c. Decrease, increase. Splitting of S2 INSPIRATION EXPIRATION Normal splitting s1 A2 P2 s1 A2 P2 Wide splitting (PS,MR,RBB B, VSD,PDA s1 A2 P2 s1 A2 P2 Paradoxical splitting (AS, LBBB, HCM, LVH) s1 P2 A2 s1 P2 A2 Fixed splitting (ASD) s1 A2 P2 s1 A2 P2 Questions A 44 y/o females has history of increasing SOB with exertion over the last 3 months. PE: Fixed split S2 with a murmur consistent with TR. Rest of HPI is unremarkable. CXR: increased LA, RA, RV and pulmonary circulation. What is the most likely diagnosis? a. Mitral regurgitation b. Aortic stenosis c. Hypertrophic obstructive cardiomyopathy d. Atrial septal defect e. Ventricular septal defect Questions A Wide splitting of S2 is representative of: a. Normal sinus rhythm with RBBB. b. Normal sinus rhythm with LBBB. c. Hypertrophic cardiomyopathy. Reversed splitting of S2 occurs in which: a. ASD b. RBBB c. Hypertrophic cardiomyopathy Heart sounds 2nd sound and opening snap of MS are best heard on the base. LSB: TR, AR, VSD, HCM Apex: MR, MS, AS. Below L clavicle: PS, PDA as continuous. Radiation to L axila: MR. Radiation to RSB and carotids: AS Radiation all over the precordium: VSD MS: Loud S1, Split S2, opening snap, rumbling diastolic murmur in apex. Area <2.5 cm, symptoms correlate. PR: Diastolic, decrescendo at LSB (Graham Steel) Questions 6. A 52 y/o female presents with history of increasing SOB and LE edema. CXR shows pulmonary congestion, straightening of left heart border and Kerle B lines. EKG: sinus tachycardia with LAE, RBBB. PE: Loud S1, opening snap and diastolic murmur at the apex, and SEM in precordium. What is the diagnosis? a. Aortic insufficiency b. Mitral stenosis c. Aortic stenosis d. Hypertrophic obstructive cardiomyopathy. Questions 7. A 33 y/o pregnant patient in second trimester has SOB due to MS that is not responding to medical treatment. ECHO shows MV of 0.5cm. What is next step: a. Mitral valvotomy after delivery. b. Offer pregnancy termination. c. Mitral valvotomy now. d. Mitral valve replacement now Mitral Valve Regurgitation Etiology: Myxomatous degeneration Rheumatic disease Endocarditis Grades 1 to 4 Surgical indications If symptomatic EF<60% LVES diameter >4.5cm Pulmonary pressure >55mmg Hg Questions A 41 year-old asymptomatic female with MVP and mitral regurgitation is presented. An ECHO shows severe MR with EF of 50%. CAD is ruled out. What is your advice regarding her treatment? a. Refer for valve replacement. b. Follow up closely. c. Begin a diuretic plus ACE-inhibitor. Aortic Stenosis Aortic Stenosis Location of murmur Second sound Carotid Pulse HCM Apex and R 2nd intercostal space radiating to carotids. No component A2 LSB, With thrill Not radiating Slowly rising Brisk or bifid Present A2 Aortic Stenosis Grades: Mild: Valve area of >1 cm2 or gradient < 40mmHg. Moderate: Valve area of 0.75 to 1 cm2 or gradient 4070 mmHg. Severe: Valve area <0.75 cm2 or gradient >70 mmHg. Surgery: If symptoms. Angina, syncope, dyspnea, CHF. If not, risk of death 10-20% per year. If not suitable for valve replacement valvuloplasty is alternative. Question A 71 year-old females has dizzy spells with near fainting. An echocardiogram shows calcified aortic valve with area of 0.5cm2. The peak systolic valve gradient is 90mmHg. She lives alone and wants everything done for her. What is the next step? a. Coronary arteriography b. ACE-Inhibitor c. Exercise stress test d. Exercise program with low dose diuretics e. Aortic valve replacement Question A 73 years old patient with R hip fracture, noted to have a SEM. Echo shows AV area of 0.76cm and gradient of 50mmHg, normal LV function. Pt is active and asymptomatic. What is the next step? a. Balloon valvuloplasty prior to surgery. b. Cardiac catheterization. c. Proceed with hip surgery. d. Aortic valve replacement before hip surgery. Questions A 23 y/o male presents to the ER with witnessed syncope while running to catch a bus. There was no observed postictal state. At PE brisk carotid upstroke. SEM 3/6 at LSB with a systolic thrill. Murmur increase upon standing. What is the most likeky diagnosis? a. Rheumatic mitral regurgitation b. Congenital aortic stenosis c. Hypertrophic obstructive cardiomyopathy d. Ebstein’s anomaly DVT/PE prophylaxis Start before or shortly after surgery. Total knee replacement minimum duration is 7 to 10 days with LMWH or warfarin. Total hip replacement minimum duration is 28-42 days with LMWH or warfarin. IPC only for patients at high risk of bleeding. Questions A patient with PE is in shock. Next step? a. Thrombolysis b. Embolectomy c. Heparin A 63 year old construction worker with h/o 3 episodes of DVT on coumadin, INR 2.5 comes again with DVT. What to do? a. Increase dose of coumadin b. Add low molecular weigth heparin c. Greenfield filter PAW=RA=RV=PA Cardiac Tamponade Constrictive Pericarditis Right Ventricular Infarction Present Present Present/Absent Calcification on X- Absent Ray, CT/MRI Present Absent ECHO Effusion with diastolic collapse Thick/calcified pericardium Large RV size EKG Low voltage and elect. alternans Low voltage ST elevation on Right leads Prominent X Present Present Absent Prominent Y Absent Present Absent Pericardial Knock Absent Present Absent Equal Diastolic Pressures Pulsus Paradoxus Present Absent in 2/3 of pt Absent Kussmaul sign Present Absent Absent/Present Cardiac Tamponade Causes: Viral, Metastasis, idiopathic, uremic, trauma, cardiac rupture, aortic disection. Features: Depends on the rapidity of fluid accumulation. Limited ventricular filling in diastole, absent Y Low cardiac output, hypotension, tachycardia, High jugular venous pressure with prominent x descent. Paradoxical pulse, lungs clear, faint heart sounds EKG: Electrical alternans, low voltage Cath: Equalization of pressures (RA, RV, PA, PCWP) Echocardiogram: RV, RA diastolic collapse, IVC dilation Treatment: Pericardiocentesis, IV fluids, surgery. Constrictive Pericarditis Causes: Post acute pericarditis, surgery, trauma, RA, radiation, TB, cancer, uremia. Features: Filling is reduced abruptly because thickened pericardium Stroke volume is reduced, equalization of pressures. High jugular venous pressure with prominent x and y descents, as M shape. Dip and plateau “square root” sign in L and R ventricular pressures Pericardial knock, kussmaul’s sign, R and L heart failure. EKG: Low voltage ECHO: Rapid decrease in filling velocities, abnormal septum motion, pericardial thickness in 80% of cases. Radiology: May have calcification Treatment: Pericardial resection with mortality 6-20%, diuretics, sinus rhythm, may resolve within months or after antiinflamatory tx. Restrictive Cardiomyopathy Causes: Infiltrative, storage and collagen diseases; radiation, anthracyclins. Features: Diastolic dysfunction, pulmonary congestion, may advance to systolic dysfunction. Dyspnea, JVD, Kussmaul’s, R side heart failure. EKG: L or R BBB, L or R VH. ECHO: LVH, homogeneous, dense walls, No calcification. Treatment: Diuretic, stem cell, deferoxamine, pacemaker. Acute Right Ventricular Infarction Causes: Inferoposterior infarction extension. Features: High jugular venous pressures, kussmaul sign, hepatomegaly, hypotension. Absent x and y. Cath: Low PAP, low PCWP, High RV EDP. EKG: ST elevation in RV4. Echo: Enlarged hypokinetic RV. Question A 64 year old male with history of RA, presents with 10 month history of refractory severe lower extremity and scrotal edema, ascitis despite diuretics. CXR with clear lung fields and small bilateral pleural effusions, calcific stipping of the cardiac silhouette. CVP has prominent x and y, with spike and plateau tracing in RV. ECHO showed normal septum thickness. What is the most likely diagnosis? A. Cor Pulmonale B. Cardiac tamponade C. Constrictive pericarditis D. Amyloid cardiomyopathy Question A 54 year old male one day post-uncomplicated IWMI. The nurse tells you that patient doesn’t have complains but the BP is 80/45 and the HR is 85. The neck veins are noticeable at the angle of the jaw and the lungs are clear to auscultation. At exam RR, no S3, no edema. What to do next? A. Cardiac catheterization B. IV dobutamine/lasix C. Atropine and then temporary pacemaker D. IV fluids Aortic Aneurysm Localized >50% diameter increase involving all three layers of the wall. Risk factors: Age>60 years, smoking, HTN, dyslipidemia, family history. If younger, think of Marfan, Ehler-Danlos , syphilis, Takayasu’s, trauma, bicuspid valve, aortic coartation. Most common in men, 3:1; infrarenal, mostly asymptomatic, can present with compression symptoms, distal embolism or rupture. Surgery if growth more than 0.5cm/year, abdominal >55 mm in men, >45mm in women, ascending aortic >50mm, and descending >60mm. Patients with >45mm should have f/u 3 months. Percutaneous repair is possible for infrarenal. After surgery, evaluate every 6 months with CT or MRI. Aortic dissection Diagnosis often delayed owing to failure to consider it as a possibility. Risk factors: In younger than 70 years: Turner’s, cocaine, bicuspid valve, collagen disorders-Marfan, Ehlers Danlos-, aortic coartation. In older than 70years: HTN, diabetes, vasculitis and preexisting aortic aneurysm. Blood pass between lumen and media creating a false lumen. Stanford A: Ascending aorta. 2:1. Involves aortic arch in 30%, worse prognosis, surgical emergency. Mortality with surgery 10-30% and without 50%. Stanford B: The rest of aorta. Mortality with medical management 10% per year or better. Surgery if occlusion of major branch, extension of dissection, Marfan. TX: BB, SBP 100-120, avoid strenous activity, F/u at 3, 6, 12 months. Presentation: Anterior or posterior CP, AR, MI, pleural or pericardial effusion, mental status changes; splacnic, renal, LE, spine ischemia. TEE, CT, MRI Question An elderly patient has chest pain radiating to the back. BP is lower in left arm. Diastolic murmur at LSB. EKG shows ST depression all over, BP 250/130. What is the immediate treatment? a. Thrombolysis b. Aspirin, lovenox. Abciximab. c. Metoprolol and NTG or NTP. d. Nicardipine Question What test will you do? A. CT chest w/o contrast B. MRI chest w/o contrast C. TTE D. TEE Showed aortic dissection of ascending aorta. Pain has improved. BP is normal. What to do next? Take patient for surgery Continue medical therapy unless rupture or pain. Wait for few days for patient to stabilize before surgery. Carotid Artery Disease Stroke is third leading cause of death. There are about 1 million strokes/year. Carotid duplex for all symptomatic, for asymptomatic with bruits if good candidate for revascularization, or any going for CABG. ASA has RRR 16% for fatal stroke and 28% for non fatal stroke. ASA is as good as CEA for symptomatic with <50% and for asymptomatic with <60%. Extended-release dipyridamole plus ASA superior to ASA alone for secondary prevention. Dual therapy as Clopidogrel plus ASA only for recurrent events despite therapy with ASA. Higher risk of bleed. Question A patient with recent TIA and ipsilateral 5069% carotid stenosis, you will recommend: A. Atherosclerotic risk factor modification B. Antiplatelet therapy C. Carotid endarterectomy D. Carotid Arterial Stenting E. A, B and C. Bacterial Endocarditis The fourth leading cause of life-threatening disease due to infection. Low incidence but high mortality. 2 major Duke criteria or 1 and 3 or 5 minor. CHF occurs on 8-30% of patients. Systemic embolization happens in up to half of cases, of those 65% involve CNS. Perivalvular abscess affect AV in 40%. TTE has sensitivity of 50-80% TEE has sensitivity of 95% for vegetations. Tx: From 2 to 6 weeks. DUKE CRITERIA 1. Positive blood culture for Infective Endocarditis Typical microorganism on 2 or more blood cultures: • Viridans streptococci, Streptococcus bovis (gallolyticus), or HABCEK or • Community-acquired Staphylococcus aureus or enterococci. Continuous bacteremia: • 2 positive cultures drawn >12 hours apart, or • all of 3 or a majority of 4 separate cultures of blood (with first and last sample drawn 1 hour apart) Positive blood culture for CB or IgG titer >1:800. 2. Evidence of endocardial involvement Positive echocardiogram for IE defined as : Vegetation or abscess or new partial dehiscence of prosthetic valve New valvular regurgitation (worsening or changing of preexisting murmur not sufficient) Duke criteria Minor criteria : Predisposition: predisposing heart condition or intravenous drug use Fever: temperature > 38.0° C (100.4° F) Vascular phenomena: major arterial emboli, septic pulmonary infarcts, mycotic aneurysm, intracranial hemorrhage, conjunctival hemorrhages, and Janeway lesions Immunologic phenomena: glomerulonephritis, Osler's nodes, Roth spots and rheumatoid factor Microbiological evidence: positive blood culture but does not meet a major criterion as noted above¹ or serological evidence of active infection with organism consistent with IE Echocardiographic findings: consistent with IE but do not meet a major criterion as noted above ¹ Excludes single positive cultures for coagulase-negative staphylococci, diphtheroids, and organisms that do not commonly cause endocarditis. AB Prophylaxis for BE Low risk: Secundum ASD Innocent murmur CABG surgery Pacemaker/ICD MVP without MR High risk: Prosthetic valve Cyanotic congenital heart disease Previous endocarditis Moderate risk: All other congenital heart disease. Bicuspid aortic valve Acquired valve disease HCM MVP with MR Surgery Indications in Bacterial endocarditis About 20-50% will require surgery. Hemodinamic instability due to valvular regurgitation, destruction. Cardiogenic shock Perivalvular extension, abscess Resistant infection Fungal endocarditis Vegetation >1cm in diameter Recurrent distal emboli. Question A 62 years old patient has had aortic valve replaced six months ago. He presents with endocarditis of the valve with findings of moderate CHF due to regurgitation. He is treated for CHF and antibiotics are started. He begins to improve with good response to the treatment. EKG has new prolonged PR interval. What is your next step? A. Continue 2 more weeks with IV AB. B. Surgery consult for AV reconstruction. C. Discharge pt with IV AB by HHC. D. Continue in hospital IV AB until 3 BC are negative. Stress testing Criteria for a “ Positive Treadmill Exercise Test”: ST depression of > 0.1 mV (1mm) below the baseline, and lasting longer than 0.08 msec. High Risk Ischemic Response Ischemia induced by low-level exercise* (less than 4 METs or heart rate < 100 bpm or < 70% of age-predicted heart rate) manifested by 1 or more of the following: Horizontal or downsloping ST depression > 0.1 mV ST-segment elevation > 0.1 mV in noninfarct lead Five or more abnormal leads Persistent ischemic response >3 minutes after exertion Typical angina Exercise-induced decrease in systolic BP by 10 mm Hg Stress testing Intermediate: Ischemia induced by moderate-level exercise (4 to 6 METs or HR 100 to 130 bpm (70% to 85% of age-predicted heart rate) with > 1 of the following: Horizontal or downsloping ST depression > 0.1 mV Persistent ischemic response greater than 1 to 3 minutes after exertion Three to 4 abnormal leads Low No ischemia or ischemia induced at high-level exercise (> 7 METs or HR > 130 bpm (greater than 85% of age-predicted heart rate)) manifested by: Horizontal or downsloping ST depression > 0.1 mV One or 2 abnormal leads Inadequate test Inability to reach adequate target workload or heart rate response for age without an ischemic response. For patients undergoing noncardiac surgery, the inability to exercise to at least the intermediate-risk level without ischemia should be considered an inadequate test. Un-interpretable Treadmill EKG Resting T-wave abnormalities WPW Paced rhythm LVH Digoxin MVP LBBB Question A patient with COPD,(having wheezing and ronchi), and PVD, unable to walk even one block needs a cardiac stress test. EKG has RAE. BP is normal. Which one? A. Dobutamine stress test B. Exercise echocardiogram C. Adenosine stress test D. Exercise electrocardiography Preoperative Evaluation Preoperative Evaluation Risk Stratification Procedure Examples Vascular (reported cardiac Aortic and other major vascular surgery risk often > 5%) Peripheral vascular surgery Intermediate (reported Intraperitoneal and intrathoracic surgery cardiac risk generally 1%-5%) Carotid endarterectomy Head and neck surgery Orthopedic surgery Prostate surgery Low† (reported cardiac Endoscopic procedures risk generally <1% Superficial procedure Cataract surgery Breast surgery Ambulatory surgery *Active cardiac conditions Condition Examples Unstable coronary syndromes Decompensated HF Significant arrhythmias Severe valvular disease Unstable or severe angina* (CCS class III or IV)† Recent MI‡ NYHA functional class IV; Worsening or new-onset HF High-grade atrioventricular block Mobitz II atrioventricular block Third-degree atrioventricular heart block Symptomatic ventricular arrhythmias Supraventricular arrhythmias (including atrial fibrillation) with uncontrolled ventricular rate (HR > 100 bpm at rest) Symptomatic bradycardia Newly recognized ventricular tachycardia Severe aortic stenosis (mean pressure gradient greater than 40 mm Hg, aortic valve area less than 1.0 cm2, or symptomatic) Symptomatic mitral stenosis (progressive dyspnea on exertion, exertional presyncope, or HF) Can You… 1 Met Take care of yourself? Can You… 4 Mets Climb a flight of stairs or walk up a hill? Eat, dress, or use the toilet? Walk on level ground at 4 mph (6.4 kph)? Walk indoors around the house? Do heavy work around the house like scrubbing floors or lifting or moving heavy furniture? Walk a block or 2 on level ground at 2 to 3 mph (3.2 to 4.8 kph)? Participate in moderate recreational activities like golf, bowling, dancing, doubles tennis, or throwing a baseball or football? 4 Mets Do light work around the house like dusting or washing dishes? ≥ 10 Mets Participate in strenuous sports like swimming, singles tennis, football, basketball, or skiing? Preoperative Evaluation Revised Cardiac Risk Index or Clinical Risk Factors Ischemic heart disease Congestive heart failure History of MIAngina Use of nitroglycerine Q waves History of heart failure Pulmonary edema Paroxysmal nocturnal dyspnea Peripheral edema, rales, S3 History of Stroke or TIA Diabetes on insulin therapy Creatinine>2mg/dl. Preoperative Evaluation Question Which of the following is most important pre-operative cardiac risk factor for noncardiac surgical procedures? A. S4 gallop B. S3 gallop C. MI 10 months ago D. Age over 70 years. Question A 71 year old male with h/o stable angina, now needs vascular surgery in the leg. What is your advice before clearing him for surgery? A. Proceed with surgery. B. Exercise stress test with imaging. C. Adenosine stress test D. Avoid surgery E. Cardiac catheterization Acute Coronary Syndrome Unstable Angina & NSTEMI TIMI risk score: Age 65 years or older 3 or more CAD traditional risk factors Documented CAD with stenosis of 50% ST segment deviation 2 or more anginal episodes in the last 24hr Aspirin use within the last 7 days Elevated cardiac enzymes Low risk: 0-2, Conservative approach with non-invasive stress testing Intermediate risk: 3-4 Initiate glycoprotein IIb/IIIa inhibitor and early invasive approach with angiography High risk: 5-7 or persistent pain or elevated troponin, angiography Question A 51 year old patient comes with typical chest pain, persistent after ASA, nitrates, betablocker, 02, morphine, statin, lovenox, is taken to the cath, showing proximal LAD 70%, Cx 30%, RCA 30%, normal ejection fraction. What to do next? CABG PCI Add ACEI Thrombolysis Indications for revascularization For PCI Unstable angina failing medical therapy or TIMI 3 or more Unstable angina in patient with prior revascularization CABG or PCI ST elevation MI Failed thrombolysis Unable to do thrombolysis MI complicated by shock, refractory ventricular arrythmia, CHF or sudden death. For CABG Left main disease 2 vessel disease with proximal LAD w (+) ischemia or low EF, most benefit seen in diabetic patients. 3 vessel disease Thrombolysis Indications for Tenecteplase: ST elevation >6hr or continuos pain and elevation up to 12hr or new LBBB with typical CP. Follow with CP, ST segment, reperfusion arrythmia, enzymes. Contraindications to thrombolytic therapy Any prior intracranial hemorrage Cerebral vascular lesion CNS neoplasm CVA <3 months except within 3 hours Significant closed head injury <3 months Active bleeding diathesis Suspected aortic dissection Question A 52-year old diabetic patient is subjected to coronary angiogram because of persistent unstable angina. It shows 2 vessel disease with EF of 35%. What is the treatment? a. PTCA b. CABG c. Medical treatment d. Thrombolysis Question A 61 y/o male had an uncomplicated anterior MI over 24 hours ago develop syncope. Telemetry showed V-tach, requiring electrical cardioversion. What to do next? Cardiac catheterization Electrophysiologic studies Echocardiography Holter monitor Signal-average ECG Question A diabetic patient has chest pain. Because of anterior wall MI with ST elevation, TPA and lovenox are started. Within 30min patient is feeling better ST-T segment came back to baseline but tele shows wide complex, NSVT. What is your next step? Observation only Intravenous lidocaine Emergent cardiac catheterization Intravenous amiodarone Electrophysiologic study Complications post-MI Rupture Ventricular Septum Rupture Rupture Papillary Muscle Myocardial Wall Timing 2-14 days 2-10 days 2-7 days Clinical findings Harsh loud systolic thrill LLSB Acute Pulmonary edema, MR murmur Sudden chest pain, shock, JVD, death New ST elev Diagnostic parameter 02 step-up in RV Severe MR, LAE Electromechanical dissociation Management Nitrohydralazine IAB Surgery Nitro IAB Surgery Usually no survival Questions Patient with IWMI whos BP goes down from 90/60 to 60/20. Next step?, What is the problem? A patient with acute MI, doing well by the second week after admission. Suddenly pt goes into acute CHF, and a new thrill at LLSB if found. What will the hemodynamic monitoring show? Question A 64 y/o male with history of uncomplicated AWMI 4 days ago has suddenly developed increasing SOB, hypotension, tachycardia, neck veins are distended, new gallop and a SEM. PCWP is 34 with a large V-wave. Diagnosis? Myocardial free-wall rupture Large pulmonary embolism Ventricular septal rupture Ruptured chordae tendineae Cardiac tamponade Question A patient with known hypertension, with no past h/o MI is admitted to CCU with a large Q-wave acute anterior MI. On the third day he is suddenly found in shock without any pulse or BP. EKG reveals new ST segment elevation with what appears to be sinus rhythm. What is the diagnosis? A. Free wall rupture B. Right Ventricle infarction C. Papillary muscle rupture D. Ventricular septal rupture