* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download 07_01 - Assessment of Cardiovascular System
Remote ischemic conditioning wikipedia , lookup
Cardiovascular disease wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Coronary artery disease wikipedia , lookup
Heart failure wikipedia , lookup
Rheumatic fever wikipedia , lookup
Aortic stenosis wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Jatene procedure wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Artificial heart valve wikipedia , lookup
Myocardial infarction wikipedia , lookup
Cardiac surgery wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Atrial fibrillation wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Electrocardiography wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
Assessment of
Cardiovascular
System
By B.Lokay, MD, PhD
Lecture Objectives:
Anatomy and physiology of cardiovascular
system.
Developmental considerations
Transcultural considerations
History taking and physical examination
Main disorders of cardiovascular system:
Congenital heart defects.
Valvular defects.
Heart failure.
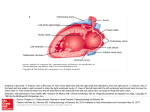
Structure of the
Cardiovascular system
Anatomical Structure of
the Heart
Common abbreviations
used to refer to chambers:
RA – right atrium AV – atrioventricular
valve
RV – right ventricle
Left AV – left
LA – left atrium
atrioventricular valve
Right AV - right
LV – left ventricle
atrioventricular valve
SL – semilunar valve
NB: No valves are
present between
major veins and
atria.
Hyperpressure leads
to signs of
Topographical Landmarks
of the Heart
Topographical Landmarks
of the Heart
Precordium – the part of the ventral surface of the body
overlying the heart and stomach and comprising the
epigastrium and the lower median part of the thorax
Topographical Landmarks
Each area corresponds to one of the hearts 4
valves.
Aortic area - 2nd ICS to right of sternum (closure of the
aortic valve loudest here).
Pulmonic area - 2nd ICS to left of sternum (closure of the
pulmonic valve loudest here).
Tricuspid - 5th ICS left of sternal border (closure of
tricuspid valve).
Mitral - 5th ICS left of the sternum just medial to MCL
(closure of mitral valve). When cardiac output is increased
as in anemia, anxiety, HTN, fever, the impulse may have
greater force - inspect for lift or heave.
Normal Heart Sounds
The first heart sound - systolic S1:
Signals the closure of AV valves and the
beginning of systole.
Consists of mitral M1 and tricuspid T1
components.
Is loudest at the apex
The second heart sound - diastolic S2:
Signals the closure of semilunar valves
and the end of systole.
Consists of aortic A2 and pulmonic P2
components.
Is loudest at the base.
S1 & S2 correspond respectively to the
familiar "lub dub" often used to describe the
sounds.
Effect of respiration:
MoRe to the Right heart
Less to the Left
A split S2 – when the aortic valve closes
significantly earlier than the pulmonic valve,
you can hear the two components separately.
Other Heart Sounds
Extra Heart Sounds:
S3
is the result of vibrations produced during
ventricular filling.
is normally heard only in some children and young
adults, but it is considered abnormal in older
individuals.
S4
is caused by the recoil of vibrations between the
atria and ventricles following atrial contraction, at
the end of diastole.
is rarely heard as a normal heart sound; usually it is
considered indicative of further cardiac evaluation.
Other Heart Sounds
Murmurs:
are produced by vibrations within the heart
chambers or in the major arteries from the
back and forth flow of blood.
are classified as:
1. Innocent, occurring in individuals with no
anatomic or physiologic abnormality.
2. Functional, occurring in individuals with no
anatomic cardiac defect but with a physiologic
abnormality such as anemia.
3. Organic, occurring in individuals with a cardiac
defect with or without a physiologic abnormality.
The conduction system of
the heart consists of four
structures:
1. The sinoatrial (SA) node, located within the rig atrial
wall near the opening of the superior vena cava
2. The atrioventricular (AV) node, also located within
the right atrium but near the lower end of the septum
3. The atrioventricular bundle (bundle of His), which
extends from the atrioventricular node along each side
of the interventricular septum
4. Purkinje fibers, which extend from the
atrioventricular bundle into the walls of the ventricles.
The electric impulses from this conduction system can
be recorded on an electrocardiogram.
Conduction System
Electrocardiography (ECG)
records the electrical impulses generated
from the heart muscle and provides a
graphic illustration of the summation of
these impulses and their sequence and
magnitude.
The ECG waves
P wave represents the electric activity associated with the
sinoatrial node and the spread of the impulse over the atria.
It is a wave of depolarization.
QRS complex (wave) is composed of three separate waves:
the Q wave, the R wave, and the S wave. They are all
caused by currents generated when the ventricles
depolarize before their contraction. Because ventricular
depolarization requires septal and right and left ventricular
depolarization, the electrical wave depicting these events is
more complex than the smooth P wave.
P-R interval is measured from the beginning of the P wave
to the beginning of the QRS complex. It is termed P-R
instead of PQ because frequently the Q wave is absent.
This interval represents the time that elapses from the begin
Q-T intervalning of atrial depolarization to the beginning of
ventricular depolarization.
The ECG waves
The T wave represents repolarization of the ventricles.
The Q-T interval begins with the QRS complex and
ends with the completion of the T wave. It represents
ventricular j depolarization and repolarization. This
interval varies with j the heart rate. The faster the rate,
the shorter the Q-T interval. Therefore in children this
interval is normally shorter than in adults.
The S-T segment is normally an isoelectric (flat) line
that I connects the end of the S wave to the beginning
of the T wave.
The T-P interval represents atrial and ventricular
polarization in anticipation of the next cardiac cycle.
Pumping Ability
4 to 6 L of blood per min throughout the
body
Preload – venous return
Afterload – the opposing pressure the
ventricles must generate to open aortic
valve.
Developmental Considerations
Infants:
Transition from fetal circulation to postnatal
circulation. By 9 months anatomical closure
of foramen ovale occurs.
S1 and S2 sounds similarly on auscultation.
Pulse rate 120/min.
Horizontal position of the heart (till 7-yearsold).
Developmental Considerations
Infants:
Apex impulse is
located at the 4th
intercostal space 1 to
2 cm outward from
left midclavicular line.
Developmental Considerations
The pregnant female:
By the end of pregnancy blood volume
increases by 30 to 40 %.
Stroke volume and cardiac output are
increased.
BP decreases due to vasodilation.
Pulse rate increases of 10 to 15 beats/min.
Developmental Considerations
Developmental Considerations
An aging adult:
The incidence of CV diseases increases with
age: coronary artery disease, HBP, heart
failure.
Transcultural considerations
Smoking: widely spread in some societies.
HBP: Afro-Americans, Mexican-Americans and Native
Americans have higher risk of hypertension.
Serum cholesterol: during childhood (4-19 yrs) AfroAmerican children have higher total cholesterol than
Euro- and Mexican-Am. Children. This difference
reverse during adulthood.
Obesity: more than 50% of Am. population are
overweight.
Diabetes: the prevalence of diabetes increases in all
groups in USA.
Physical Examination
Objectives:
Subjective data.
Health history data.
Preparation.
Inspection: general appearance, precordium.
Palpation: peripheral pulses, apical impulse.
Percussion.
Auscultation: heart sounds, murmurs.
Summary checklist.
Subjective data
Chest pain:
Angina – an important
cardiac symptom.
“Clenched fist” sign is
characteristic of angina.
Onset, location, character, aggravating
and/or relieving factors
Character: crashing, stabbing, burning,
vise-like.
Associated symptoms: sweating, ashen
gray or pale skin, shortness of breath,
nausea or vomiting, racing of heart, heart
skips beat.
Subjective data
Dyspnea:
Paroxysmal nocturnal dyspnea (PND)
occurs with heart failure.
Classically, the person awakens after
2 hrs. of sleep, arises, and flings
open the window with the perception
of needing fresh air.
Cause, onset, duration, affection by position,
Does shortness of breath interfere with
activities of daily living?
Orthopnea:
Is the need to assume a more upright
position to breathe.
Note the exact number of pillows used.
Subjective data
Hemoptysis is often a
pulmonary problem,
but also occurs with
mitral stenosis
Cough: duration, frequency, type,
coughing up sputum (color, odor, blood
tinged, aggravating and/or relieving
factors.
Fatigue: onset, relation to time of day?
Cyanosis or pallor: occurs with
myocardial infarction or low cardiac
output.
Subjective data
Edema:
Swelling of legs or dependent body part due
to increased interstitial fluid.
Onset, recent change, relation to time of day,
relieving factors, associated symptoms.
Nocturia:
Occurs with heart failure in the person who
is ambulatory during the day.
History taking.
Past cardiac history:
! Last ECG, stress ECG, serum chilesterol
measurements, other heart tests?
Family cardiac history:
Family history of hypertension, diabetes,
heart problems, coronary artery disease
(CAD), sudden death at younger age?
Personal habits (cardiac risk factors):
nutrition, smoking, alcohol, exercise,
drugs.
Additional history
For infants: mother’s health during pregnancy,
feeding habits, growth, activity.
For children: growth, activity, any joint pains or
unexplained fever, frequent headaches or
nosebleedings, streptococcal infection
(tonsillitis).
For pregnant female: any high PB during this
or previous pregnancies, associated signs
(weight gain, proteinuria), dizziness.
For aging adult: any symptoms of heart
diseases (HTN, CAD) or COPD, any recent
changes, medications (digitalis), side effects;
environment.
Preparation
Bring to lab:
Watch with second hand,
Stethoscope,
Marking pen and small centimeter ruler,
Alcohol swab (to clean endpiece).
Wear:
loose T-shirt or some other garment
that allows for practice of physical
assessment
Inspection
Skin colour (cyanosis, pallor) and condition
Any obvious bulging on anterior thorax at the
left
Edema
Orhtopnea
Palpation
Palpate the apical impulse (the point of
maximal impulse, or PMI):
Location: one intercostal space (usually 5th
ICS) at left MCL,
Size: normally 1 cm 2 cm,
Amplitude: normally a shot, gentle tap,
Duration: short, normally occupies only first
half of systole.
Ask the client “to exhale then hold it” or turn
him to the left side.
Palpation
Palpation
Palpate across the precordium for:
Other pulsations,
Thrill – palpable vibration due to strong heart
murmur (like a purring cat),
Pericardial friction rubs are scratchy, highpitched grating sounds, similar to pleural
friction rubs, except that they are not
affected by changes in respiration.
Accentuated S1 and S2.
A diffuse impulse (lift, heave).
Palpation
Percussion
Is used to estimate approximately heart
borders and configuration.
Recently is displaced by the chest x-ray
or EchoCG.
Helps to detect heart enlargement
Heart (cardiac) enlargement is
due to increased ventricular
volume or thickening of heart
wall.
Occurs with HTN, CAD, heart
failure, cardiomyopathy
Auscultation
Auscultation
A Z-pattern is recommended.
Before beginning alert the person for long
duration of procedure.
Begin with diaphragm endpiece and use
the following routing:
Note the rate
the rhythm
Identify S1 and S2
Listen for extra heart sounds
Listen for murmurs
Auscultation (cont.)
Rhythm:
Regular
Irregular:
Synus arrythmia – common variation. Rate ↑
on inspiration and ↓ on expiration.
Regularly irregular
Irregularly irregular – no pattern to the sounds,
beats come rapidly and at random intervals.
Pulse deficit – occurs with atrial fibrillation,
heart failure, detects weak heart contractions.
Auscultation (cont.)
Identify S1 and S2
Location and amplitude,
Correlation with peripheral pulses, PMI
Correlation with ECG waves
“Lub” or “dup”
Give description of origin.
Listen to sounds separately:
accentuation, split (fixed, paradoxical).
Auscultation (cont.)
Extra heart sounds:
Midsystolic click
S3: normal, pathological (ventricular gallop)
S4: atrial gallop
Listen for murmurs:
Characteristics: timing, loudness, pitch,
pattern, quality, location, radiation, posture
Grading murmurs
Grade I-VI:
Refers to the severity of a heart murmur (blowing,
whooshing, or rasping sound), which is the result of
vibrations caused by turbulent blood flow patterns.
Murmurs are classified ("graded") depending on
their ability to be heard by the examiner. The
grading is on a scale with grade I being barely
detectable.
An example of a murmur description is a "grade II/VI
murmur." (This means the murmur is grade 2 on a
scale of 1 to 6).
Murmurs are classified according to their
timing within the cardiac cycle.
Systolic Between S1and S2.
Diastolic Between S2 and S1).
Systolic ejection Begin after the first heart sound,
attain a peak during midsystole, and terminate
before the second heart sound.
Pansystolic or holosystolic During all of systole.
Pandiastolic or holodiastolic During all of
diastole.
Prodiastolic Early diastolic.
Presystolic Late diastolic.
Continuous Continue through all of systole and all
or part of diastole.
Timing of murmurs
Conclusion
Function can be assessed to a large degree by findings in
the history: shortness of breath (SOB), edema of
ankles/legs, pain, pulse rate and rhythm; vital signs, signs
and symptoms of oxygen deficit.
Location: Heart lies behind and to the left of the sternum.
The upper portion or atria (BASE) lies to the back; the
ventricles (APEX) points forward, the apex of the left
ventricle actually touches the anterior chest wall near the
left midclavicular line at or near the 5th left ICS. Known as
point of maximal impulse (PMI) and is where apical beat is
assessed. Impulse is a good index of heart size.
Landmarks for assessment: The precordium is the area on
the anterior chest overlying the heart. Hearts sounds are
heard throughout the precordium, but there are 4 major
areas for examining heart sounds.
Techniques of Assessment:
Inspection- look for lift at apex.
Auscultation- Client should be assessed
in supine position with head up to 45
deg.; examiner stands at right side. Use
diaphragm for basic sounds; bell for
murmurs and extra sounds.
Identify the heart rate, rhythm; bell for
murmurs aortic, pulmonic, mitral.
Heart Sounds
There are 2 basic normal heart sounds and several
abnormal ones. Normal:
S1 (produced by closure of the atrioventricular valves,
mitral and tricuspid)- at mitral area and tricuspid area S1 is
louder than S2. The sound is a dull, low pitched “lub.”
S2 (produced by closure of aortic and pulmonic valve) is
higher pitched, shorter and is the “dub” sound. Heard best
at the base (aortic and pulmonic areas) where S2 is louder
than S1
Systole begins with the 1st sound. As ventricles start to
contract, pressure within exceeds the atria, shutting the
mitral and tricuspid valves. Blood is forced into the great
vessels.
When the ventricles have emptied themselves, the
pressure in the aorta and pulmonary arteries force the
semilunar valves shut (aortic/pulmonic), which is the 2nd
sound and diastole (ventricular relaxation) begins.
Other heart sounds
S3 – rapid filling of the ventricle with blood; heard
following S2. Can be normal in young adults and
children; pathologic in elderly.
S4 – atrial contraction and thought to result from
stiffened left ventricle; directly precedes S1. Heard
in elderly.
Extra sounds: snaps and clicks are associated
with valves: aortic and mitral stenosis, prosthetic
valves.
Murmurs: S1 or S2 is a swishing or blowing
sounds caused by
Forward flow through a stenotic (narrowed) valve
Increased flow through a normal valve
Backward flow through a valve that fails to close
(insufficiency).
Murmurs should be identified as systolic
(S1) or diastolic (S2). Murmurs are common
in children and occur often in the elderly.
Try to identify grade of murmur: Grade I
(barely audible) to Grade VI (loud and may
be heard with the stethoscope not quite on
the chest or barely touching the chest).
Documentation: Normally, you should be
able to note that S1, S2 heard without extra
sounds.