* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download PowerPoint 演示文稿 - Shandong University
Management of acute coronary syndrome wikipedia , lookup
Coronary artery disease wikipedia , lookup
Aortic stenosis wikipedia , lookup
Cardiothoracic surgery wikipedia , lookup
Artificial heart valve wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Heart failure wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Electrocardiography wikipedia , lookup
Cardiac surgery wikipedia , lookup
Myocardial infarction wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Jatene procedure wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Ventricular fibrillation wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
Heart arrhythmia wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
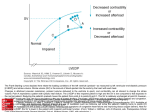
LIU Chuan Yong 刘传勇 Institute of Physiology Medical School of SDU Tel 88381175 (lab) 88382098 (office) Email: [email protected] Website: www.physiology.sdu.edu.cn CHAPTER 4 THE CARDIOVASCULAR SYSTEM Weight of the heart 300g Work: 75/min, 10000 beats /day 35 million beats /year, 2.5 billion beats/life 70ml/beat, 7200 l/day The work of the heart in one life is equivalent to lifting 30 tons to the Mount Everest The busy and hard working heart! MAIN FUNCTIONS OF THE CIRCULATORY SYSTEM Transport and distribute essential substances to the tissues. Remove metabolic byproducts. Adjustment of oxygen and nutrient supply in different physiologic states. Regulation of body temperature. Humoral communication. Systemic and Pulmonary Circulation A. Heart location in the chest B. Heart Chambers B. Heart Chambers 1. Right Heart receives venous blood from systemic circulation via superior and inferior vena cava into right atrium b. pumps blood to pulmonary circulation from right ventricle 2. Left Heart a. receives oxygenated blood from pulmonary circulation b. pumps blood into systemic circulation C. Heart Valves 1. Atrioventricular a. tricuspid--between RA and RV; three leaflets b. mitral--between LA and LV; two leaflets 2. Semilunar a. pulmonic--three leaflets b. aortic--three leaflets Heart Valves Prevent backward regurgitation Provide low resistance to forward flow Section 1 The Heart as a Pump I Cardiac Cycle The period from the end of one heart contraction to the end of the next Cardiac Cycle Diastole is longer than systole The sequence of systole and diastole Cardiac Cycle: diastole and systole Diastole Systole 2 The Phases of the Cardiac Cycle (1) Period of isometric (isovolumetric or isovolumic) contraction Events: ventricular contraction ventricular pressure rise atrioventricular valve close the ventricular pressure increase sharply Period: 0.05 sec Importance: enable the ventricular pressure to rise from 0 to the level of aortic pressure (after-load) (2) Period of ejection Events: ventricular contraction continuously the ventricular pressure rise above the arterial pressure semilumar valves open blood pours out of the ventricles Rapid ejection period (0.10s, 60% of the stroke volume) Reduced ejection period (0.15s, 40% of the stroke volume) (3) Period of isometric (isovolumic) relaxation Events: ventricular muscle relax the ventricular pressure fall lower than the aortic pressure aortic valve close the ventricular pressure fall sharply Period: 0.06-0.08 s Importance: Enable the ventricular pressure fall to the level near the atrial pressure (4) Period of filling of the ventricles Events: Ventricular muscle relax continuously the ventricular pressure is equal or lower than the atrial pressure atrioventricular valve open blood accumulated in the atria rushes into the ventricular chambers quickly from the atrium to the ventricle. Period of rapid filling. (0.11s, amount of filling, 2/3) Period of reduced filling (0.22s, little blood fills into the ventricle) (5) Atrial systole Significance, 30% of the filling Be of major importance in determining the final cardiac output during high output states or in the failing heart LEFT VENTRICULAR PRESSURE (mmHg) LEFT VENTRICULAR PRESSURE/VOLUME P/V LOOP 120 F E D 80 40 A 0 50 B C 100 150 LEFT VENTRICULAR VOLUME (ml) 2) Pressure changes in the atria, the a, c, and v waves. a wave, the atrial contraction c wave, bulging of the A-V valves when the ventricles begin to contract v wave, at the end of ventricle contraction, caused by the accumulated blood in the atria while the A-V valves are closed Heart Sounds The sounds heard over the cardiac region produced by the functioning of the heart. Heart Sounds S1- first sound Atrioventricular valves and surrounding fluid vibrations as valves close at beginning of ventricular systole S2- second sound closure of aortic and pulmonary semilunar valves at beginning of ventricular diastole S3- third sound vibrations of the ventricular walls when suddenly distended by the rush of blood from the atria Mitral Closes :>D S2 Atrial Systole Reduced Ventricular Filling Rapid Ventricular Filling Isovolumic Relax. Reduced Ejection Rapid Ejection Isovolumic contract. Atrial Systole :>O CARDIAC CYCLE Aortic opens Aortic closes Mitral opens S1 II Cardiac Output Stroke Volume – The volume pumped by the heart with each beat, = end diastole volume – end systole volume, about 70 ml 2. Ejection Fraction – Stroke volume accounts for the percentage of the end diastolic volume, = stroke volume / end diastole volume X 100%, normal range, 55-65% II Cardiac Output 3. Minute Volume, or Cardiac Output – the volume of the blood pumped by one ventricle, = stroke volume X heart rate. It varies with sex, age, and exercise 4. Cardiac Index, the cardiac output per square meter of body surface area. the normalized data for different size individuals, the normal range is about 3.0 – 3.5 L/min/m2 Determinants of Cardiac Output (CO) Contractility Preload Heart Rate Stroke Volume Cardiac Output Afterload Definitions Preload amount of stretch on the ventricular myocardium prior to contraction Afterload the arterial pressure (or some other measure of the force) that a ventricle must overcome while it contracts during ejection impedance to ventricular ejection Definitions Contractility myocardium’s intrinsic ability to efficiently contract and empty the ventricle (independent of preload & afterload) Determinants of Cardiac Output 1. Preload Determinants of Cardiac Output- Preload Preload = ventricular filling or volume Determinants of Cardiac Output - Preload Preload approximated by measuring: 1. Central venous pressure (CVP) = right atrial pressure. 2. Pulmonary capillary diastolic wedge pressure (PCWP) = LVEDP Parameters: 1. CVP 3mm Hg (normal range 1 - 5) 2. PCWP 9mm Hg (normal range 2 - 13) Frank-Starling Mechanism of the Heart The intrinsic ability of the heart to adapt to changing volumes of inflowing blood the Frank - Starling mechanism of the heart: Left ventricle (LV) function curve, or Frank - Starling curve (1914): Normal range of the LVEDP, 56 mmHg Optimal initial preload, 15-20 mmHg (Sarcomere, 2.0 – 2.2 µm When the LVEDP > 20 mmHg, LV work is maintained at almost the same level, does not change with the increase of LVEDP Mechanism Factors determining the preload (LVEDP) Period of the ventricle diastole (filling) – heart rate Speed of the venous return (difference between the venous pressure and atrial pressure) Importance of the heterometeric regulation In general, heterometric regulation plays only a short-time role, such as during the body posture change, artery pressure increase, unbalance of ventricular outputs. In other conditions, such as exercise, cardiac output is mainly regulated by homometric regulation. Determinants of Cardiac Output - Afterload Short time change of the arterial pressure Transit arterial pressure rise isovolumetric contraction phase become longer period of ejection shorter stroke volume less more blood left in the ventricle left LVEDP increase through heterometeric regulation stroke volume return to normal in next beat. Long time high arterial pressure through neural and humoral regulation the stroke volume is maintained at normal level pathogenesis of the cardiovascular system Determinants of Cardiac Output - Contractility Contractility (neural and humoral regulation) Sympathetic nerve (norepinephrine) or the epinephrine and norepinephrine (adrenal gland) enhance the strength and the velocity of the cardiac contraction. The change of myocardial property is independent of the preload. We call it the contractility. Importance: exert a long – time influence on the cardiac output. Definitions Contractility myocardium’s intrinsic ability to efficiently contract and empty the ventricle (independent of preload & afterload) Action of Sympathetic Stimulation Sympathetic nerve stimulation increases cardiac contractility. At rest the heart is under sympathetic tone. Noradrenaline enhances calcium entry into cardiac cells. Parasympathetic stimulation has little affect on contractility due to the innervation pattern of the heart. PRESSURE/VOLUME RELATIONSHIPS UNDER DIFFERENT CONDITIONS PRELOAD AFTERLOAD CONTRACTILITY Determinants of Cardiac Output - The heart rate Normal range of the heart rate 60 – 100 beats/min Within physiological limit?, the higher the heart rate, the more blood that the heart pump. 1, at rest (without any regulation) 2, during exercise (with humoral and neural regulation) IV Cardiac Output Reserve The maximal cardiac output subtracts the normal value. It reflects the ability of the heart to adapt the change of environment (internal or external) Normal range End diastole volume 145ml – end systole volume 75ml = stroke volume 70 ml Heart rate 75 beats/min Normal cardiac output = 70 X 75 = 5.25 L /min Maximal level Maximal diastole volume 160 ml (reserve 15ml); Maximal systole residual volume 20 ml (reserve 55ml) Maximal heart rate (without the stroke volume decrease )180 beats/min (reserve 105 beats/min) Maximal cardiac output (160 – 20) X 180 = 25.2 L/min