* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Mechanic work of the heart.
Management of acute coronary syndrome wikipedia , lookup
Heart failure wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Coronary artery disease wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Jatene procedure wikipedia , lookup
Cardiac surgery wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Myocardial infarction wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
Atrial fibrillation wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Mechanic work of the heart.
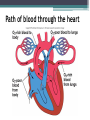
• The pumping of the heart sends out blood
under pressure to the arteries.
• Blood pressure is greatest in the aorta; the
wall of the left ventricle is thicker than
that of the right ventricle and pumps
blood to the entire body.
• Blood pressure then decreases as the
cross-sectional area of arteries and then
arterioles increases.
Path of blood through the heart
Cardiac cycle
• The cardiac cycle refers to the repeating pattern of
contraction and relaxation of the heart. The phase of
contraction is called systole, and the phase of relaxation
is called diastole.
• When these terms are used without reference to specific
chambers, they refer to contraction and relaxation of the
ventricles. It should be noted, however, that the atria also
contract and relax. There is an atrial systole and diastole.
Atrial contraction occurs toward the end of diastole, when
the ventricles are relaxed; when the ventricles contract
during systole, the atria are relaxed.
Cardiac cycle
Cardiac Output
• Volume of blood pumped per unit time from the
ventricle
• In mammals this is the volume ejected from
either the left or right ventricle, not the
combined total
• Volume of blood ejected per beat is the stroke
volume
• Stroke volume determined by dividing cardiac
output by heart rate
• Stroke Volume = end diastolic volume - end
systolic volume
• Cardiac Output = SV X heart rate (HR)
• Determinants of EDV
▫
▫
▫
▫
1. venous filling pressure
2. atrial contraction pressure
3. dispensability of the ventricular wall
4. time for filling
• Determinants of ESV
▫ 1.ventricular pressure during contraction
▫ 2. pressure in the outflow channels
(arterial)
Frank Starling Mechanism
• increased work due
to increased EDV
based on increased
venous filling pressure and the concurrent length-tension
changes in cardiac
muscle
The Heartbeat
• Each heartbeat is called a cardiac cycle.
• When the heart beats, the two atria contract
together, then the two ventricles contract;
then the whole heart relaxes.
• The heart sounds, lub-dup, are due to the
closing of the atrioventricular valves,
followed by the closing of the semilunar
valves.
Heart rate
•
•
•
•
•
- Normal range is 60-100 beats per minute
- Tachycardia is greater than 100 bpm
- Bradycardia is less than 60 bpm
- Sympathetic system INCREASES HR
- Parasympathetic system (Vagus) DECREASES
HR (CBQ)
Intrinsic Control of Heartbeat
• The SA (sinoatrial) node, or pacemaker,
initiates the heartbeat and causes the atria to
contract on average every 0.85 seconds.
• The AV (atrioventricular) node conveys the
stimulus and initiates contraction of the
ventricles.
• The signal for the ventricles to contract
travels from the AV node through the
atrioventricular bundle to the smaller
Purkinje fibers.
Conduction system of the heart
Extrinsic Control of Heartbeat
• A cardiac control center in the medulla
oblongata speeds up or slows down the heart
rate by way of the autonomic nervous system
branches: parasympathetic system (slows
heart rate) and the sympathetic system
(increases heart rate).
• Hormones epinephrine and norepinephrine
from the adrenal medulla also stimulate
faster heart rate.
ECG
• The way of excitation which spreads through the
heard wall consists of changes in the electrical
activity of the membrane of cardiac muscle cells.
Like nerve and skeletal muscle, the outer surface of
active cardiac muscle is electrically negative to the
resting cardiac muscle ahead of the zone of excitation.
The electrical currents generate lines of force similar to
those produced by a magnet and are conducted through
the salty water-like body fluids to the surface of the body
and can be received, amplified and recorded by
electrodes of an instrument – an electrocardiograph.
The record obtained is an electrocardiogram (ECG).
The Electrocardiogram
• An electrocardiogram (ECG) is a
recording of the electrical changes
that occur in the myocardium
during a cardiac cycle.
• Atrial depolarization creates the P
wave, ventricle depolarization
creates the QRS wave, and
repolarization of the ventricles
produces the T wave.
Electrocardiogram
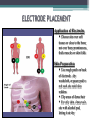
ELECTRODE PLACEMENT
Application of Electrodes
Choose site over soft
tissues or close to the bone;
not over bony prominences,
thick muscles or skin folds
Skin Preparation
Use rough patch on back
of electrode , dry
washcloth, or gauze pad to
rub each site until skin
reddens
Clip areas of dense hair
For oily skin, clean each
site with alcohol pad,
letting it air dry
• An ECG depicts electrical activity as
waves, segments, and intervals. By
convention, upward deflection of the
waves is defined as positive (+), and
downward deflection as negative (!). The
electrical activity associated with atrial
depolarization is defined as the Pwave
("0.3mV, "0.1 s). Repolarization of the
atria normally cannot be visualized on the
ECG since it tends to be masked by the
QRS complex. The QRS complex ("0.1 s)
consists of one, two or three components:
Q wave (mV " 1/4 of R, "0.04 s), Rwave
and/or S wave (R+S #0.6 mV).
• The potential of the mean QRS vector
is the sum of the amplitudes of the Q, R
and Swaves (taking their positive and
negative polarities into account). The
voltage of the mean QRS vector is higher
(in most leads) than that of the P wave
because the muscle mass of the
ventricles is much larger than that of the
atria. The Rwave is defined as the first
positive deflection of the QRS complex,
which means that R waves from
different leads may not be synchronous.
The QRS complex represents the
depolarization of the ventricles, and the
T wave represents their repolarization.
• Although opposing processes, the T
wave usually points in the same
direction as the R wave (+ in most
leads). This means that depolarization
and repolarization do not travel in the
same direction (QRS and T: vector
arrows point in the same direction
despite reversed polarity during
repolarization). The PQ (or PR)
segment (complete atrial excitation)
and the ST segment (complete
ventricular excitation) lie approx. on
the isoelectric line (0 mV).
• The PQ (or PR) interval (!0.2 s) is
measured from the beginning of the
Pwave to the beginning of the Q wave (or
to the R wave if Q wave is absent) and
corresponds to the time required for
atrioventricular conduction. The QT
interval is measured from the start of
the Q wave to the end of the T wave. It
represents the overall time required for
depolarization and repolarization of the
ventricles and is dependent on the heart
rate (0.35 to 0.40 s at a heart rate of 75
min–1).
ECG
During each cardiac cycle 2 heart sounds can be heart through a
stethoscope applied to the chest wall.
Auscultation
The sounds may be represented phonetically:
These sounds repeated with every cardiac cycle i.e. about 70 times per
minute in the average healthy adult at rest.
If the valves have been damaged by disease additional sounds (murmurs)
can be heart as the blood flows forwards through narrowed valves or leaks
backwards through incompetent valves. Systolic murmurs occure between
LUBB and DUP. Diastolic murmurs occur between DUB and the next
LUBB.