* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Circulatory System
Heart failure wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Electrocardiography wikipedia , lookup
Artificial heart valve wikipedia , lookup
Coronary artery disease wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Heart arrhythmia wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
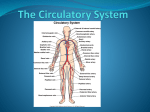
Blood, Heart, and Vascular System II. The Heart Size, Shape, Location of the Heart • Size of a closed fist • Shape – Apex: Blunt rounded point of cone – Base: Flat part at opposite of end of cone • Located in thoracic cavity in mediastinum A. Structure – 4 chambered double pump organ 1. Atria (2)– receiving chambers 2. Ventricles (2) – delivering chambers a) Atrioventricular (AV) – found between the atrium and ventricles 1. Tricuspid (on right) 2. Bicuspid or mitral (on left) 3. Chordae Tendinae (reinforce valves, attached in ventricles) b) Semilunar – found between the ventricles and the aorta 1. Aortic 2. Pulmonary c) Prevent blood from flowing back heartarteries arterioles veinsvenules capillaries The double pump 3. Heart Valves 3. Heart Valves Function of the Heart Valves 4. Heart Wall Layers a) The heart is surrounded by the pericardial cavity. The lining of the cavity, a serous membrane, is the Pericardium b) Epicardium: covers the outer surface of heart c) Myocardium: middle layer, muscular wall of the heart, and responsibility for heart contracting d) Endocardium: smooth inner lining of heart chambers 4. Heart Wall Layers Continuous with blood vessels 4. Heart Wall Layers 5. Coronary Vessels – blood vessels that supply the myocardium 6. Conducting System of Heart – specialized network of nerves supply the heart Intrinsic Control of Heartbeat • The SA (sinoatrial) node, or pacemaker, initiates the heartbeat and causes the atria to contract on average every 0.85 seconds. • The AV (atrioventricular) node conveys the stimulus and initiates contraction of the ventricles. • The signal for the ventricles to contract travels from the AV node through the atrioventricular bundle to the smaller Purkinje fibers. Extrinsic Control of Heartbeat • A cardiac control center in the medulla oblongata speeds up or slows down the heart rate by way of the autonomic nervous system branches: parasympathetic system (slows heart rate) and the sympathetic system (increases heart rate). • Hormones epinephrine and norepinephrine from the adrenal medulla also stimulate faster heart rate. Electrocardiogram - (ECG) can trace conduction of electrical signals through the heart • Action potentials through myocardium during cardiac cycle produces electric currents than can be measured • Pattern – P wave • Atria depolarization – QRS complex • Ventricle depolarization • Atria repolarization – T wave: • Ventricle repolarization Aberrant ECG patterns indicate damage B. Functions of the Heart • Delivery of oxygenated blood to the body’s tissues and deoxygenated blood to the lungs • Generating blood pressure • Ensuring one-way blood flow – Heart valves ensure one-way flow • Regulating blood supply – Changes in contraction rate and force match blood delivery to changing metabolic needs B. Functions of the Heart 1. Contraction (systole) of the ventricles 2. Relaxation (diastole) of the ventricles 3. Cardiac Cycle: The beginning of one ventricular contraction to the next; a heartbeat. a) When the heart beats, the two atria contract together, then the two ventricles contract; then the whole heart relaxes. Cardiac Cycle Events during Cardiac Cycle Blood Flow Through Heart 4. Heart Rate: Number of beats per minute. a) Average adult heart rate is 80-100 bpm b) The infant/neonatal rate of heartbeat is around 130-150 bpm, toddler’s is 100-130 bpm, older child is 90-110 bpm, adolescent is 80-100 bpm. c) Tachycardia: Heart rate in excess of 100 bpm d) Bradycardia: Heart rate less than 60 bpm 5. Heart Sounds a. Lup - Dub i. First heart sound or “lub” – Closure of the Atrioventricular valves and surrounding fluid vibrations at beginning of ventricular systole ii. Second heart sound or “dup” – Results from closure of aortic and pulmonary semilunar valves at beginning of ventricular diastole, lasts longer b. Abnormal heart sounds – Caused by turbulent blood flow into ventricles and detected near end of first one-third of diastole – The result of faulty valves Coordination of chamber contraction, relaxation Location of Heart Valves Regulation of the Heart • Intrinsic regulation: Results from normal functional characteristics, not on neural or hormonal regulation • Extrinsic regulation: Involves neural and hormonal control – Parasympathetic stimulation • Supplied by vagus nerve, decreases heart rate, acetylcholine secreted – Sympathetic stimulation • Supplied by cardiac nerves, increases heart rate and force of contraction, epinephrine and norepinephrine released Heart Homeostasis • Effect of blood pressure – Baroreceptors monitor blood pressure • Effect of pH, carbon dioxide, oxygen – Chemoreceptors monitor levels • Effect of extracellular ion concentration – Increase or decrease in extracellular K+ decreases heart rate • Effect of body temperature – Heart rate increases when body temperature increases, heart rate decreases when body temperature decreases Effects of Aging on the Heart • Gradual changes in heart function, minor under resting condition, more significant during exercise • Hypertrophy of left ventricle • Maximum heart rate decreases • Increased tendency for valves to function abnormally and arrhythmias to occur • Increased oxygen consumption required to pump same amount of blood C. Pathologies • Coronary Artery Disease – Arteriosclerosis or atherosclerosis of the vessels (plaques) that supply the myocardium (cannot deliver blood adequately) • Congestive Heart Failure – insufficiency of the ventricles to effectively pump out blood into the atria. Can result in cardiac arrest. • Mitral Valve Prolapse – failure of the left atrioventricular valve, allowing a backflow of blood into the left atria, creating abnormal heart sound or a murmur. C. Pathologies • Angina pectoris (pain) when body is not receiving adequate oxygen • Myocardial Infarction (heart attack) – a blockage of blood in a coronary blood vessel, resulting in death of a portion of the myocardium. This is usually accompanied by chest pain or angina. • Cardiac Arrest – cessation of all cardiac activity. No heartbeat. • Hypertension – high blood pressure; the arterial pressure is too high; treated with exercise, dietary changes, and medications. – Risks: sedentary lifestyle, smoking, obesity, high Na+, high cholesterol, stress, arteriosclerosis, genetic factors D. Why is exercise good for the heart? • A trained heart is bigger – pumps blood more efficiently (at a lower rate) – stroke volume increases (due to stronger contractions, allowing for lower rate) • other benefits: higher aerobic capacity (contributing to efficiency) • Note that this takes training! III. Vascular System The blood, heart, and blood vessels together make up the Cardiovascular system or circulatory system. A. Arteries and veins transport blood to tissues and allows for exchange of molecules through capillaries. 1. Arteries – carry blood from the heart to the tissues a) Carry oxygenated blood (except the pulmonary arteries carry deoxygenated blood to the lungs) b) Arteries and arterioles take blood away from the heart. c) The largest artery is the aorta. d) The middle layer of an artery wall consists of smooth muscle that can constrict to regulate blood flow and blood pressure. (thick muscular walls) e) Arterioles can constrict or dilate, changing blood pressure. f) Aorta to artery to arteriole to capillary 2. Veins – carry blood from the tissues toward the heart a) Carry deoxygenated blood (except the pulmonary veins carry oxygenated blood to the heart) b) Venules drain blood from capillaries, then join to form veins that take blood to the heart. c) Veins have much less smooth muscle and connective tissue than arteries. (thinner, less muscular walls) d) Veins often have valves that prevent the backward flow of blood when closed. e) Veins carry about 70% of the body’s blood and act as a reservoir during hemorrhage. Blood vessels 3. Capillaries – permeable network of vessels that allow the exchange of materials. a) Capillaries have walls only one cell thick (one endothelial layer) to allow exchange of gases and nutrients with tissue fluid. b) Capillary beds are present in all regions of the body but not all capillary beds are open at the same time. c) Contraction of a sphincter muscle closes off a bed and blood can flow through an arteriovenous shunt that bypasses the capillary bed. Anatomy of a capillary bed How does this system work? lungs pulmonary vein pulmonary artery head & arms aorta main vein Right Left liver digestive system kidneys legs Circulatory System Our circulatory system is a double circulatory system. This means it has two parts parts. Lungs the right side of the the left side of the system system deals with deals with deoxygenated blood. oxygenated blood. Body cells B. Vasodilatation – increase in diameter of a blood vessel 1) Decreases temperature C. Vasoconstriction – decrease in diameter of a blood vessel 1) Increases temperature D. Blood pressure – the amount of pressure the blood exerts on the vessel wall 1) Systolic – highest number reading; ventricular contraction 2) Diastolic – lowest number reading; ventricular relaxation Pathologies • Arteriosclerosis - hardening of the arteries. • Atherosclerosis - due to a build-up of fatty material (plaque) along the walls of arteries. – This fatty material thickens, hardens (forms calcium deposits), and may eventually block the arteries. – Slows down or stops blood flow; leads to chest pain (angina) or heart attack. – Atherosclerosis is a type of arteriosclerosis. The two terms are often used to mean the same thing. Pathologies • Hypertension – About 20% of Americans suffer from hypertension (high blood pressure). – Hypertension is present when systolic pressure is 140 or greater or diastolic pressure is 100 or greater; diastolic pressure is emphasized when medical treatment is considered. – A genetic predisposition for hypertension occurs in those who have a gene that codes for angiotensinogen, a powerful vasoconstrictor. • Aneurysm - a ballooning of a blood vessel, usually in the abdominal aorta or arteries leading to the brain. Pathologies • Varicose Veins - develop when the valves of veins become weak • Hemorrhoids (piles) - due to varicose veins in the rectum • Phlebitis/thombophlebitis - inflammation of a vein and can lead to a blood clot and possible death if the clot is dislodged and is carried to a pulmonary vessel. Pathologies • DVT: Deep Vein Thrombosis - a blood clot forms in a vein that is in the lower leg and thigh. – The clot can block blood flow and cause swelling and pain. Can have an embolism, break off and move through the body. An embolism can get stuck in the brain, lungs, heart, or other area, leading to severe damage. • Reynaud's Syndrome - a condition that causes some areas of your body (fingers, toes, tip of your nose and ears) to feel numb and cool in response to cold temperatures or stress. – Smaller arteries that supply blood to your skin narrow, limiting blood circulation to affected areas. – More likely in women and in those people who live in colder climates.