* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download 03_CLIN_PHARM_ANTIBACTERIAL
Pharmacogenomics wikipedia , lookup
Discovery and development of tubulin inhibitors wikipedia , lookup
Discovery and development of ACE inhibitors wikipedia , lookup
Discovery and development of neuraminidase inhibitors wikipedia , lookup
Pharmaceutical industry wikipedia , lookup
Prescription costs wikipedia , lookup
Discovery and development of integrase inhibitors wikipedia , lookup
Neuropharmacology wikipedia , lookup
Psychopharmacology wikipedia , lookup
Discovery and development of proton pump inhibitors wikipedia , lookup
Drug interaction wikipedia , lookup
Drug discovery wikipedia , lookup
Pharmacognosy wikipedia , lookup
Ciprofloxacin wikipedia , lookup
Levofloxacin wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
Discovery and development of cephalosporins wikipedia , lookup
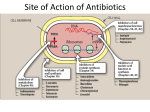
CLINICAL PHARMACOLOGY OF ANTIBACTERIAL AND ANTIVIRAL AGENTS ANTIBACTERIAL DRUGS. Mechanisms of Action 1. Inhibition of bacterial cell wall synthesis or activation of enzymes that disrupt bacterial cell walls (eg, penicillins, cephalosporins, vancomycin) 2. Inhibition of protein synthesis by bacteria or production of abnormal bacterial proteins (eg, aminoglycosides, clindamycin, erythromycin, tetracyclines). These drugs bind irreversibly to bacterial ribosomes, intracellular structures that synthesize proteins. When antimicrobial drugs are bound to the ribosomes, bacteria cannot synthesize the proteins necessary for cell walls and other structures. 3. Disruption of microbial cell membranes (eg, antifungals) 4. Inhibition of organism reproduction by interfering with nucleic acid synthesis (eg, fluoroquinolones, rifampin, anti–acquired immunodeficiency syndrome antivirals) 5. Inhibition of cell metabolism and growth (eg, sulfonamides, trimethoprim) Actions of antibacterial drugs on bacterial cells • Beta-Lactam Antibiotics PENICILLINS THE PENICILLINS ARE CLASSIFIED AS BETA-LACTAM DRUGS BECAUSE OF THEIR UNIQUE FOUR-MEMBERED LACTAM RING. THEY SHARE FEATURES OF CHEMISTRY, MECHANISM OF ACTION, PHARMACOLOGIC AND CLINICAL EFFECTS, AND IMMUNOLOGIC CHARACTERISTICS WITH CEPHALOSPORINS, MONOBACTAMS, CARBAPENEMS, AND -LACTAMASE INHIBITORS, WHICH ALSO ARE -LACTAM COMPOUNDS. A penicillin culture PENICILLINS Indications for Use Clinical indications for use of penicillins include bacterial infections caused by susceptible microorganisms. As a class, penicillins usually are more effective in infections caused by gram-positive bacteria than those caused by gramnegative bacteria. However, their clinical uses vary significantly according to the subgroup or individual drug and microbial patterns of resistance. The drugs are often useful in skin/ soft tissue, respiratory, gastrointestinal, and genitourinary infections. However, the incidence of resistance among streptococci, staphylococci, and other microorganisms continues to grow. Aminopenicillins Piperacillin CEPHALOSPORINS & CEPHAMYCINS Cephalosporins and cephamycins are similar to penicillins chemically, in mechanism of action, and in toxicity. Cephalosporins are more stable than penicillins to many bacterial β-lactamases and therefore usually have a broader spectrum of activity. Cephalosporins are not active against enterococci and Listeria monocytogenes. Cephalosporins Indications for Use Cefepime is indicated for use in severe infections of the lower respiratory and urinary tracts, skin and soft tissue, female reproductive tract, and infebrile neutropenic clients. It may be used as monotherapy for all infections caused by susceptible organisms except P. aeruginosa; a combination of drugs should be used for serious pseudomonal infections. MONOBACTAMS These are drugs with a monocyclic -lactam ring . They are relatively resistant to lactamases and active against gram-negative rods (including pseudomonas and serratia). They have no activity against gram-positive bacteria or anaerobes. Aztreonam is the only monobactam available in the USA. It resembles aminoglycosides in its spectrum of activity. Aztreonam is given intravenously every 8 hours in a dose of 1–2 g, providing peak serum levels of 100 g/mL. The half-life is 1–2 hours and is greatly prolonged in renal failure. BETA-LACTAMASE INHIBITORS (CLAVULANIC ACID, SULBACTAM, & TAZOBACTAM) These substances resemble beta-lactam molecules but themselves have very weak antibacterial action. They are potent inhibitors of many but not all bacterial lactamases and can protect hydrolyzable penicillins from inactivation by these enzymes. CARBAPENEMS The carbapenems are structurally related to beta-lactam antibiotics. Ertapenem, imipenem, and meropenem are licensed for use in the USA. Imipenem has a wide spectrum with good activity against many gram-negative rods, it is administered together with an inhibitor of renal dehydropeptidase, cilastatin, for clinical use. Meropenem is not significantly degraded by renal dehydropeptidase and does not require an inhibitor. Ertapenem is less active than meropenem or imipenem against Pseudomonas aeruginosa and acinetobacter species. It is not degraded by renal dehydropeptidase. CHLORAMPHENICOL Chloramphenicol is a potent inhibitor of microbial protein synthesis. It binds reversibly to the 50S subunit of the bacterial ribosome. CHLORAMPHENICOL. TOXICITY FOR NEWBORN INFANTS Newborn infants lack an effective glucuronic acid conjugation mechanism for the degradation and detoxification of chloramphenicol. Consequently, when infants are given dosages above 50 mg/kg/d, the drug may accumulate, resulting in the gray baby syndrome, with vomiting, flaccidity, hypothermia, gray color, shock, and collapse. TETRACYCLINES MACROLIDES Erythromycin Clarithromycin (is derived from erythromycin) Azithromycin (differs from erythromycin and clarithromycin mainly in pharmacokinetic properties). The drug is slowly released from tissues (tissue half-life of 2–4 days) to produce an elimination half-life approaching 3 days. These unique properties permit once-daily dosing and shortening of the duration of treatment in many cases. Ketolides (Telithromycin) is approved for clinical use. Many macrolide-resistant strains are susceptible to ketolides Aminoglycosides Streptomycin, neomycin, kanamycin, amikacin, gentamicin, tobramycin, sisomicin, netilmicin The pharmacodynamic properties of aminoglycosides are: Concentration-dependent killing Significant post-antibiotic effect Lincosamides Clindamycin is indicated for treatment of anaerobic infection caused by bacteroides and other anaerobes that often participate in mixed infections. Clindamycin is now recommended rather than erythromycin for prophylaxis of endocarditis in patients with valvular heart disease who are undergoing certain dental procedures. Clindamycin plus primaquine is an effective alternative to trimethoprimsulfamethoxazole for moderate to moderately severe Pneumocystis jiroveci pneumonia in AIDS patients. It is also used in combination with pyrimethamine for AIDS-related toxoplasmosis of the brain. Oxazolidinones Linezolid is a member of the oxazolidinones, a new class of synthetic antimicrobials. It is active against gram-positive organisms including staphylococci, streptococci, enterococci, gram-positive anaerobic cocci, and gram-positive rods such as corynebacteria and Listeria monocytogenes. Empirical ‘blind’ therapy Most antibiotic prescribing, especially in the community, is empirical. Even in hospital practice, microbiological documentation of the nature of an infection and the susceptibility of the pathogen is generally not available for a day or two. Initial choice of therapy relies on a clinical diagnosis and, in turn, a presumptive microbiological diagnosis. Such ‘blind therapy’ is directed at the most likely pathogen(s) responsible for a particular syndrome such as meningitis, urinary tract infection or pneumonia. Examples of ‘blind therapy’ for these three conditions are ceftriaxone, trimethoprim and amoxicillin + erythromycin, respectively. Initial therapy in the severely ill patient is often broad spectrum in order to cover the range of possible pathogens but should be targeted once microbiological information becomes available. SULFONAMIDES Sulfonamides are infrequently used as single agents. SULFONAMIDES. ORAL NONABSORBABLE AGENTS Sulfasalazine (salicylazosulfapyridine) is widely used in ulcerative colitis, enteritis, and other inflammatory bowel disease Fluoroquinolones Quinolones Ciprofloxacin, enoxacin, lomefloxacin, evofloxacin, ofloxacin, and pefloxacin comprise a second group of similar agents possessing excellent gram-negative activity and moderate to good activity against grampositive bacteria. Gatifloxacin, moxifloxacin, sparfloxacin, and rovafloxacin comprise a third group of fluoroquinolones with improved activity against gram-positive organisms, particularly S.pneumoniae and to some extent staphylococci. The fluoroquinolones side effects Fluoroquinolones are approved for use only in people older than 18. They can affect the growth of bones, teeth, and cartilage in a child or fetus. The fluoroquinolones side effects Phototoxicity. Exposure to ultraviolet A rays from direct or indirect sunlight should be avoided during treatment and several days (5 days with sparfloxacin) after the use of the drug. The degree of phototoxic potential of fluoroquinolones is as follows: lomefloxacin > sparfloxacin > ciprofloxacin > norfloxacin = ofloxacin = levofloxacin = gatifloxacin = moxifloxacin.