* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Uric acid estimation in plasma
Point mutation wikipedia , lookup
Catalytic triad wikipedia , lookup
Metalloprotein wikipedia , lookup
Genetic code wikipedia , lookup
Basal metabolic rate wikipedia , lookup
Fatty acid metabolism wikipedia , lookup
Peptide synthesis wikipedia , lookup
Citric acid cycle wikipedia , lookup
Amino acid synthesis wikipedia , lookup
Nucleic acid analogue wikipedia , lookup
Fatty acid synthesis wikipedia , lookup
Biochemistry wikipedia , lookup
Biosynthesis wikipedia , lookup
Butyric acid wikipedia , lookup
15-Hydroxyeicosatetraenoic acid wikipedia , lookup
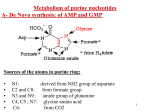
Uric acid estimation in plasma Learning Objectives Describe the principle of uric acid estimation in serum and its clinical importance Uric acid Uric acid is produced by the breakdown of purines, which are essential components of nucleic acids (DNA and RNA) as well as other important biomolecules such as ATP, cyclic AMP and NADH. Normal value The normal value of uric acid in human plasma: In males: 3.5 - 7 mg/dl. In females: 3.0 - 6 mg/dl. Procedure Blood is drawn from a vein and transferred into a centrifuge tube containing an anticoagulant. Plasma is obtained by centrifugation of blood for 10 minutes. In clean dry test tubes take 50 μl of distilled water (blank) , standard uric acid solution (standard) and plasma (test). Then add 1 ml of Monoreagent (the monoreagent is composed of: uricase enzyme, peroxidase enzyme, 4-AA, ADPS and buffer to adjust pH to 7). Mix the content of each tube and incubate for 5 min at 37 °C using a water bath. Remove test tubes from the water bath. Protocol for Colorimetric estimation of Uric acid Measure the absorbance of the final color of the sample and standard against blank at 550nm. The color is stable for 30 minutes protected from light. Calculate the concentration of uric acid in the sample using the following equation Principle of estimation Uricase Uric acid + O2 +H2O Allantoin + H2O2 Peroxidase H2O2 + 4AA + ADPS Quinoneimime + 4 H2O The method used is a colorimetric enzymatic method. Uric acid is oxidized by Uricase to allantoin with the formation of Hydrogen peroxide. Hydrogen peroxide can oxidize a mixture of ADPS and 4-aminoantipyrine (4AA) to form a quinoneamine that absorbs maximally at 550 nm. ADPS , highly water soluble aniline derivative, (N-Ethyl-N-(3-sulfopropyl)-3methoxyaniline, sodium salt, monohydrate ESPAS) PHBA (Polyhalogenated benzoic acid ) may also be used instead Lab exercise Qassim University College of Medicine Phase 2, Yr. 1 , Musculoskeletal & Integumentary Block (CMD222) Biochemistry Lab exercise Saturday, June 13, 2010 Student Name :_____________________, ID: ____________________ Exercise : Determine uric acid concentration (mg/dl) in the given sample. Mention your requirements here: Use values in the protocol below to determine the concentration of uric acid in the sample DISTILLED WATER STANDARD URIC ACID SOLUTION (50 MG/L) PLASMA SAMPLE MONOREAGENT ABSRBANCE AT λ 550nm BLANK 50 μl - STANDARD 50 μl SAMPLE 25 μl - 1 ml 0 1 ml 25 μl 1 ml Write your comment on the case: ……………………………………………………………………………………… ……………………………………………………………………………………… Describe the principle of the method …………………………………………………………………………………… ? ? Clinical significance Hyperuricemia > 7 mg/dl In some cases, the level of uric acid is higher than 7 mg/dl; this is known as hyperuricemia May be due to: High intake of purine rich diet Impaired excretion of uric acid in the kidney Chemotherapy- related side effects(due to breakdown of tumour cells and release of purines) Stress or excessive exercise Toxemia of pregnancy Hyperuricemia may lead to Formation of kidney stones: Most of uric acid is removed by the kidneys and disposed of in the urine. In hyperuricemia Uric acid crystals precipitate in the kidney and may block filtering tubules leading to renal failure. Uric acid crystals in a urine sample Sodium urate/ kidney stones Gout: A chronic type of inflammatory arthritis in which uric acid crystals accumulate in the joints causing severe inflammation. It usually affects the joint of big toe, other joints including ankles, knees and elbows may be affected X-ray of gouty uric acid deposit in the big toe Uric acid crystals in big toe joint Gout (hyperuricemia): A metabolic disease characterized by increased levels of uric acid (as urates) in the blood, hyperuricemia (above 7.0 mg/dL) accompanied with increased excretion of uric acid in the urine. - This results in the deposition of sodium urate in the form of monosodium urate needle-like crystals on the joint linings and in soft tissues around it (especialy those of the big toe) skin, kidney and other tissues. The precipitated urates are called tophi. It results in inflammatory reactions in the joints, i.e., acute gouty arthritis that progresses to a chronic form. Uric acid and urates precipitates in the kidney and urinary tract may result in stone formation. Urate in the blood could accumulate either through an overproduction and/or an under-excretion of uric acid. Types of gout: A) Primary: (inherited defect) (1) Metabolic: is due to inherited autosomal or X-linked recessive metabolic defects (congenital enzyme deficiencies) characterized by increased rate of purine synthesis and/or decreased rate of salvaging purine from the breakdown pathway, leading to overproduction of uric acid. • Lesch-Nyhan syndrome: that is a X-linked recessive complete deficiency of hypoxanthine-guanine phosphoribosyltransferase (HGPRT) that leads to increased rate of purine synthesis, breakdown and excretion with tendency of self-mutilation and uric acid stones formation. • Von Gierke's disease (The glycogen storage disease) is another example, in which absence of glucose-6-phosphatase shuttles glucose-6-phosphate to HMP-shunt with excessive production of ribose, a precursor for purine synthesis. (2) Primary renal gout: is a rare condition and is due to an inherited defect in the kidney leading to decreased secretion of urates by the renal tubules. Lack of HGPRT activity in Lesch-Nyhan Syndrome causes a buildup of PRPP, which activates the synthesis of purine nucleotides hypoxanthine-guanine phosphoribosyl transferase Guanine + PRPP Hypoxanthine + PRPP Guanylate + PPi Inosinate + PPi Purine Salvage and Lesch-Nyhan syndrome Salvage pathways collect hypoxanthine and guanine and recombine them with PRPP to form nucleotides in the HGPRT reaction Absence of HGPRT is cause of Lesch-Nyhan syndrome This increase may be due to PRPP feed-forward activation of de novo pathways the rate of purine synthesis is increased about 200X Symptoms are gouty arthritis due to uric acid accumulation and severe neurological malfunctions including mental retardation, aggressiveness, and self-mutilation B) Secondary: The levels (urates) in the body fluids are elevated as a result of: Increased uric acid production secondary to increased cell destruction and breakdown of nucleoproteins (increased turnover of nucleic acids) as malignancies, prolonged fasting, Polycythaemia, Pneumonia, Psoriasis. Decreased excretion of uric acid as in severe renal failure (secondary renal gout). Types of gout • Primary gout: Due to inherited metabolic defects leading to excessive purine production and resultant hyperuricemia. e.g. altered function of PRPP synthase Clinical disorder Defective enzyme Nature of Defect Manifestation Gout PRPP Synthase increased enzyme activity due to elevated Vmax Hyperuricemia Gout PRPP Synthase enzyme is resistant to feed-back inhibition Hyperuricemia Gout PRPP Synthase enzyme has increased affinity for ribose-5-phosphate (lowered Km) Hyperuricemia Gout HGPRT partially defective enzyme Hyperuricemia Lesch-Nyhan Syndrome HGPRT Complete deficiency Hyperuricemia –self mutilation Other Disorders of purine metabolism Clinical disorder Defective enzyme Nature of Defect Manifestation Severe combined Immunodeficiency ADA Complete deficiency T & B cell immunodeficiency Immunodeficiency Purine nucleoside phosphorylase Complete deficiency T & B cell immunodeficiency. Inosinuria, deoxyinosinuria, hypouricemia, guanosinuria etc Renal Lithiasis adenine Phosphoribosyltransferase Complete deficiency 2,8-dihydroxyadenine renal Lithiasis Xanthiuria Xanthine Oxidase Complete deficiency Xanthine renal Lithiasis, hypouricemia