* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Slide 1
Survey
Document related concepts
Transcript
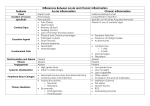
Objective • Clinical Spectrum of SIRS. • Signaling – Humoral – Neural – Hormonal • Inflammatory Mediators. • Cell Mediated Inflammatory response. • Surgical Metabolism. Introduction • Inflammatory response to injury – to restore tissue function – Eradicate invading microorganisms • Local- limited duration, restores function • Major – overwhelming inflammatory response – Potential multi-organ failure Clinical Spectrum of SIRS • Infection – Identifiable source of microbial insult • Sepsis – • SIRS = 2 or more: – – – – Temp ≥38˚C or ≤36˚C HR ≥ 90 bpm RR ≥ 20 breaths/min or PaCO2 ≤ 32 mmHg or mechanical ventilation WBC ≥ 12,000 or ≤ 4000 or ≥ 10% immature forms Infection + SIRS • Severe Sepsis – Sepsis + Organ Dysfunction • Septic Shock – Sepsis + Cardiovascular Collapse (requires vasopressors) Signaling • Humoral – inflammatory mediators in the circulation can induce fever and anorexia i.e. TNF-α • Neural – parasympathetic vagal stimulation attenuates the inflammatory response via Ach release – Reduces HR, increases gut motility, dilates arterioles, constricts pupils, and decreases inflammation – Reduces macrophage activation – Reduces macrophage release of pro-inflammatory mediators (TNF-α, IL-1, IL-18) Hormone Signaling Adrenocorticotropic Hormone • Synthesized anterior pituitary • Regulated by circadian signals • Pattern is dramatically altered in injured patients • Elevation is proportional to injury severity • Released by: pain, anxiety, vasopressin, angiotensin II, cholecystokinin, catecholamines, and pro-inflammatory cytokines • ACTH signals increase glucocorticoid Glucocorticoids • Cortisol – elevated following injury, – duration of elevation depends on severity of injury • Potentiates hyperglycemia – Hepatic gluconeogenesis – Muscle and adipose tissue –> induces insulin resistance – Skeletal m.–> protein degradation, lactate release – Adipose -> reduces release of TG, FFA, Exogenous administration • Adrenal suppression in the acutely ill – – – – Acute Adrenal Insufficiency Atrophy of the adrenal glands Weakness, n/v, fever, hypotension Hypoglycemia, hyponatremia, hyperkalemia • Immunosuppression – Decreased T-killer and NK fcn, graft vs host rxns, delayed hypersensitivity responses, inability of monocyte intracellular killing, inhibition of superoxide reactivity and chemotaxis in neutrophils Macrophage Inhibitory Factor • Glucocorticoid antagonist • produced by anterior pituitary & Tlymphocytes • Reverses immunosuppressive effects of glucocorticoids Growth Hormone • During stress -> protein synth, fat mobilization, and skeletal cartilage growth • Injury reduces IGF1 levels • IGF1 inhibited by pro-inflammatory cytokines – TNF-α, IL-1α, IL-6 Aldosterone • Synthesized, stored, released from the adrenal zona glomerulosa • Maintains intravascular volume – Conserves Na. – Eliminates potassium and hydrogen ions – Acts on the early distal convoluted tubules • Deficiency- hypotension, hyperkalemia • Excess- edema, HTN, hypokalemia, metab alkalosis Insulin • Stress inhibited release + peripheral insulin resistance = hyperglycemia • Injury has 2 phases of insulin release – Within hours- release is suppressed – Later- normal/xs insulin production with peripheral insulin resistance • Activated lymphocytes have insulin receptors -> enhanced Tcell proliferation and cytotoxicity • Tight control of glucose levels esp. in Acute Phase Proteins • • • • • Nonspecific markers Produced by hepatocytes Response to injury, infection, inflammation Induced by IL-6 C-reactive protein best reflects inflammation – No diurnal variation, not affected by feeding – Affected only by preexisting hepatic failure – Accuracy surpasses that of ESR Inflammatory Mediators • • • • • • • • Heat Shock Proteins Reactive Oxygen Metabolites Eicosanoids Fatty Acid Metabolites Kallikrein-Kinin System Serotonin Histamine Cytokines Heat Shock Proteins • Induced by hypoxia, trauma, heavy metals, and hemorrhage • Requires gene induction by a transcription factor • ACTH sensitive • Production seems to decline with age Reactive Oxygen Metabolites • Cause tissue injury by oxidation of unsaturated fatty acids within cell membranes • Produced by anaerobic glucose oxidation and reduction to superoxide anion in leukocytes • Further metabolized to hydrogen peroxide and hydroxyl radicals • Cells are protected by oxygen scavengers – glutathione and catalases • In ischemia- production of oxygen Eicosanoids Eicosanoids • Secreted by nucleated cells (not lymphocytes) • Induced by hypoxic injury, direct tissue injury, endotoxin, norepinephrine, vasopressin, ang II, bradykinin, serotonin, ACh, cytokines, histamine • Diverse systemic effects • Adverse effects include acute lung injury, pancreatitis, renal failure Fatty Acid Metabolites • Omega 6 FA – precursors of inflammatory mediators (PG, platelet activating factor) – found in enteral nutrition formulas • Substituting Omega 3 FA attenuate the inflammatory response – Reduces TNFα, IL6, PGE2 – Reduces the metabolic rater, normalizes glucose metabolism, attenuates weight loss, improves nitrogen balance, reduces endotoxin induced acute lung injury, minimizes reperfusion injury to the myocardium, small intestine, and skeletal muscles. Kallikrein-Kinin System • Bradykinins are potent vasodilators • Stimulated by hypoxic and ischemic injury – Hemorrhage, sepsis, endotoxemia, tissue injury – Magnitude proportional to severity of injury • Produced by kininogen degradation by kallikrein • Kinins increase capillary permeability Serotonin • Present in intestinal chromaffin cells & platelets • Vasoconstriction, bronchoconstriction, platelet aggregation • Myocardial chronotrope and ionotrope • Unclear role in inflammation Histamine • Stored in neurons, skin, gastric mucosa, mast cells, basophils, and platelets • H1 – bronchoconstriction, VD, increases intestinal motility and myocardial contractility • H2 – stimulates gastric parietal cell acid secretion. • H3 – downregulation of histamine release. Cytokines • Most potent mediators of inflammation • Local- eradicate microorganisms, promote wound healing • Overwhelming responsehemodynamic instability (septic shock) or (muscle wasting) • Uncontrolled- end-organ failure, death • Self-regulatory production of antiinflammatory cytokines, but Tumor Necrosis Factor α • Secreted from monocytes, macrophages, Tcells • Responds early, T ½ < 20min • Potent evocation of cytokine cascade • Induces muscle catabolism/cachexia, coagulation, PGE2, PAF, glucocorticoids, eicosanoids Interleukin-1 • Released by activated macrophages, endothelial cells • IL1α- cell membrane associated • IL1β- circulation • Synergistic with TNF- α • T ½ = 6 min • Induces febrile response by stimulating PG activity in the anterior hypothalamus • Release of β-endorphins after surgery reduce perception of pain Interleukin-2 • Promotes T-lymphocyte proliferation, Ig production, gut barrier integrity • T ½ < 10 min • Major injury or perioperative blood transfusions reduce IL-2 activity leading to a transient immunocompromised state • Regulates lymphocyte apoptosis Interleukin-4 • Produced by type 2 T Helper lymphocytes • Important in antibody-mediated switching and antigen presentation • Induces class switching to promote IgE & IgG4 – Important in allergic and antihelmintic responses • Anti-inflammatory- downregulates IL-1, TNF-α, IL-6, IL-8 and oxygen radical production Interleukin-5 • Released from T lymphocytes, eosinophils, mast cells and basophils • Promotes eosinophil proliferation and airway inflammation Interleukin-6 • Induced by IL-1 and TNF-α • Levels are detectable within 60 min of injury, peak 4-6 hours, and persist up to 10 days • Levels are proportional to extent of tissue injury • Pro-inflammatory – Induces and prolongs neutrophil activity • Anti-inflammatory – Attenuate TNF-α and IL-1 activity – Promote release of circulating TNF- α receptors & IL1 antagonists Interleukin-8 • Released from monocytes, macrophages, T lymphocytes • Activity similar to IL-6 • Chemoattractant for PMNs, basophils, eosinophils, and lymphocytes, activates PMNs Interleukin-10 • • • • Anti-inflammatory Released from T lymphocytes Down-regulates TNF-α activity Also attenuates IL-18 mRNA in monocytes • Reduces mortality in animal sepsis and ARDS models Interleukin-12 • Promotes differentiation of type 1 T Helper cells • Promotes PMN and coagulation activation Interleukin-13 • Similar to IL-4, overall anti-inflammatory • Promotes B-lymphocyte function • Unlike IL-4, has no effect on T lymphocytes • Inhibits NO production and endothelial activation Interleukin-15 • Derived from macrophages • promotes lymphocyte activation. • promotes neutrophil phagocytosis in fungal infections Interleukin-18 • Produced by macrophages • Pro-inflammatory, similar to IL-12 • Increased levels are pronounced (especially in sepsis) and can last up to 21 days • high levels found in cardiac deaths Interferon-γ • Helper T lymphocytes activated by bacterial antigens, IL-2, IL-12, or IL-18 produce IFN-γ • IFN-γ can induce IL-2, IL-12, or IL-18 • Detectable in circulation by 6 hrs and remain elevated for up to 8 days • Activate circulating and tissue macrophages • Induces acute lung inflammation by activating alveolar macrophages after surgery or trauma Granulocyte-Macrophage ColonyStimulating Factor • Delays apoptosis of macrophages and PMNs • Promotes the maturation and recruitment of PMNs in inflammation and perhaps wound healing • May contribute to organ injury such as ARDS High Mobility Group Box 1 • DNA transcription factor • Facilitates the binding of regulatory protein complexes to DNA • Secreted by macrophages, natural killer cells, and enterocytes. • Expressed 24-48 hrs after injury • Associated with weight loss, shock, SIRS and Sepsis. • Peak levels are associated with ARDS and death Cell Mediated Inflammation • Platelets – Source of eicosanoids and vasoactive mediators – Clot is a chemoattractant for PMNs/monocytes – Modulate PMN endothelium adherence – Migration occurs within 3 hrs of injury • Mediated by serotonin, PAF, PGE2 • Eosinophils – Migrate to parasitic infection and allergen challenge to release cytotoxic granules – Reside in the GI, lung, and GU tissues – Activated by IL-3, GM-CSF, IL-5, PAF, and anaphylatoxins C3a and C5a Cell Mediated Inflammation • Lymphocytes – T-helpers produce IL-3, TNF-α, GM-CSF • • • TH1: IFN-γ, IL-2, IL-12 TH2: IL-4, IL-5, IL-6, IL-9, IL-10, IL-13 Severe infection – shift toward more TH2 • Mast Cells – First responders to injury – Produce histamine, cytokines, eicosanoids, proteases, chemokines, TNF-α (stored in granules) – Cause vasodilation, capillary leakage, and Cell Mediated Inflammation • Monocytes – Downregulation of receptor TNFR is clinically and experimentally correlated with CHF, nonsurvival in sepsis • Neutrophils – – – – Modulate acute inflammation Maturation is stimulated by G-CSF Rolling (L-selectin (fast), P-selectin (slow) Adhesion/transmigration – ICAM 1, 2, PECAM 1, VCAM 1, CD18 Endothelium-Mediated Injury • Neutrophil-Endothelium Interaction – Increased vascular permeability – facilitate oxygen delivery and immunocyte migration – Accumulation of neutrophils at injury sites can cause cytotoxicity to vital organs – Ischemia-reperfusion injury potentiates this response by releasing oxygen metabolites and lysosomal enz. – Neutrophils – rolling 10-20min (p-selectin), >20min Nitric Oxide • Derived from endothelial surfaces responding to Ach, hypoxia, endotoxin, cellular injury, or shear stresses of circulating blood • T ½ = seconds • Reduces microthrombosis, mediates protein synthesis in hepatocytes • Formed from oxidation of L-arginine. Prostacyclin (PGI2) • Endothelium derived in response to shear stress and hypoxia • Vasodilator • Platelet deactivation (increases cAMP) • Clinically used to reduce pulmonary hypertension (especially pediatric) Endothelins • Produced as a response to a variety of factors – injury, anoxia, thrombin, IL-1, vasopressin • ET-1 is a potent vasoconstrictor, 10x more potent than angiotensin II Platelet Activating Factor • Phospholipid component of cell membranes, constitutively expressed at low levels • Released by PMNs, platelets, mast cells, monocytes during acute inflammation • Further activates PMNs and platelets • Increases vascular permeability • PAF antagonists reduce ischemia/reperfusion injury Metabolism During Fasting • Comparable to changes seen in acute injury • Requires 25-40 kcal/kg/day of carbs, protein, fat • Normal adult body contains 300-400g carbs (glycogen) – 75-100g hepatic, Metabolism During Fasting • A healthy 70kg adult will use 180 g /d of glucose to support obligate glycolytic cells (neurons, RBCs, PMNs, renal medulla, skeletal m.) • Glucagon, Norepi, vasopressin, AngII promote utilization of glycogen stores • Glucagon, Epi, and cortisol promote gluconeogenesis • Precursors include lactate (sk.m., rbc, pmn), glycerol, and aa (ala, glutamine) Metabolism of Simple Starvation • Lactate is not sufficient for glucose demands • Protein must be degraded (75 g/d) for hepatic gluconeogenesis • Proteolysis from decreased insulin and increased cortisol • Elevated urinary nitrogen (up to 30 g/d or more) Metabolism of Prolonged Starvation • Proteolysis is reduced to 20g/d and urinary nitrogen excretion stabilizes to 2-5g/d • Organs (myocardium, brain, renal cortex, sk.m) adapt to ketone bodies in 2-24 days • Kidneys utilize glutamine and glutamate in gluconeogenesis • Adipose stores provide up to 40% calories (approx 160 g FFA and glycerol) – Stimulated by reduced insulin and increased glucagon and catecholamines Metabolism Following Injury • Magnitude of expenditure is proportional to the severity of injury • Changes in – Lipid Absorption – Lipid Oxidation – Carbohydrate metabolism Influence of injury severity on resting metabolism Lipid Absorption • • • • • • Oxidation of 1g fat = 9 kcal energy Dietary lipids require pancreatic lipase and phospholipase to hydrolyze TG into FFA and monoglycerides within the duodenum After gut absorption, enterocytes resynthesize TG from monoglycerides + fatty acyl-CoA Long chain TG (>12 carbons) enter the circulation as chylomicrons. Shorter FA chains directly enter portal circulation and are transported via albumin Under stress, hepatocytes utilize FFA as fuel Systemically TG and chylomicrons are used from hydrolysis with lipoprotein lipase (suppressed by trauma and sepsis) Fatty Acid Oxidation • FFA + acyl-CoA = LCT are transported across the mitochondrial inner membrane via the carnitine shuttle • Medium-chain TG (MCT) 6-12 carbons long, freely cross the mitochondrial membrane • Fatty acyl-CoA undergoes β-oxidation to acetyl-CoA to enter TCA cycle for oxidation to ATP, CO2, and water • Excess acetyl-CoA is used for ketogenesis Carbohydrate Metabolism • Carbohydrates + pancreatic intestinal enzymes yield dimeric units (sucrase, lactase, maltase) • Intestinal brush border disaccharidases break them into simple hexose units which are transported into the intestinal mucosa • Glucose and galactose are absorbed via a sodium dependent active transport pump • Fructose absorption via facilitated Carbohydrate Metabolism • 1g carbohydrate = 4 kcal energy • IV/parenteral nutrition 3.4 kcal/g dextrose • In surgical patients dextrose administration is to minimize muscle wasting • Glucose can be utilized in a variety of pathways – phosphorylation to G6P then glycogenesis or glycogenolysis, pyruvic acid pathway, or pentose shunt Protein and Amino Acid Metabolism • Average adult protein intake 80-120 g/day – every 6 g protein yields 1 g nitrogen – 1g protein = 4 kcal energy • Following injury, glucocorticoids increase urinary nitrogen excretion (>30g/d), peak at 7d, persist 3-7 wks The effect of injury severity on nitrogen wasting References The material was directly adapted from: Schwartz's Principles of Surgery, 8th ed.