* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download chapter_6_ppt
Low-density lipoprotein wikipedia , lookup
Cholesterol wikipedia , lookup
Epoxyeicosatrienoic acid wikipedia , lookup
15-Hydroxyeicosatetraenoic acid wikipedia , lookup
High-density lipoprotein wikipedia , lookup
Phospholipid-derived fatty acids wikipedia , lookup
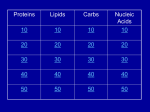
Saturated fat and cardiovascular disease wikipedia , lookup
Chapter 6: Lipids Properties of Lipids • Do not readily dissolve in water • Fats are solid at room temperature • Oils are liquid at room temperature Functions of Lipids • • • • • • • Provide energy Satiety Flavor and mouth feel Insulation Protect internal organs Transport fat-soluble vitamins Efficient storage of energy – 80% lipid, 20% protein and water Triglycerides • Triglycerides are the main form of lipids in food and body (storage) • Energy dense (9 kcal /g) Triglycerides H O H--C--OH HO-C-R H H--C--O--C-- R + H2O O H--C--OH + HO-C-R O H--C--O--C-- R + H20 O H--C--OH HO-C-R H Glycerol O O H--C--O--C-- R + H20 H + 3 FA’s Triglyceride + 3 H20 Text art 06_02 Structure • Esterification – Joining 3 fatty acids to a glycerol unit • De-esterification – Release of fatty acids-results in free fatty acids • Diglyceride – Loss of one fatty acid • Monoglyceride – Loss of two fatty acids 7 Structure of Fatty Acids • Fatty acids – Function is dependent on: • Length • Degree of saturation • Location of double bonds • Configuration/Shape – Glycerol backbone Fatty Acid Chain Length • Long chain FA: > 12 Carbons – Predominant in food (meats, fish) • Medium chain FA: 6 - 10 Carbons – Account for ~4-10% of all FA • Short chain FA: < 6 Carbons – Found in dairy products Saturated Fatty Acid Monounsaturated Fatty Acid Polyunsaturated Fatty Acid Location of Double Bonds • Omega System – Double bond closest to omega (methyl) end – Omega: refers to the last carbon (methyl group) – Omega 6 vs Omega 3 fatty acids • Delta (alpha) System – Uses the carboxyl end and indicates location for all double bonds Fatty Acid Structure H H H H H H H H H H H H H H H HHO H-C--C--C--C--C--C--C--C--C--C--C--C--C--C--C--C--C-C-OH H H H H H H H H H H H H H H H H H omega end end alpha Fatty Acid Nomenclature Configuration/Shape • cis versus trans Common Fatty Acids NAME Acetic acid Propionic acid Butyric acid Decanoic acid Palmitic acid Stearic acid Oleic acid Linoleic acid Linolenic acid Arachidonic acid STRUCTURE 2:0 3:0 PROPERTIES Formed from glucose and amino acid degradation Formed from odd-chain fatty acids and branchedchain amino acids 4:0 Found in cows’ milk and butter 10:0 Major fatty acid in milk triglycerides 16:0 End product of fatty acid synthesis in most tissues 18:0 Major fatty acid in gangliosides 18:1 (∆9) Lowers plasma LDL when substituted for saturated fatty acids 18:2 (∆9,12) Essential fatty acid and precursor of Arachidonic acid 18:3 (∆9,12,15) Essential fatty acid 20:4 (∆5,8,11,14) Precursor of most eicosanoids Saturated Fatty Acids • Fatty acids with no double bonds • Solid at room temperature • Animal fats: – Dairy: cheeses, ice cream, whole milk – Meat: beef, pork, lamb, – Plant/tropical oils (cottonseed, coconut) • Stearic, lauric, myristic, palmitic Saturated Fatty Acid Trans Fatty Acids • Essentially a saturated fat • Raise LDL • Lower HDL risk for heart disease • Intake has increased dramatically – Found in margarine, cookies, potato chips, snack chips, onion rings • Current intake is~3% of total kcals Hydrogenation of Fatty Acids • Process used to solidify an oil • Addition of hydrogen to an unsaturated fatty acid (eliminating the double bond—making it into a saturated fatty acid) • Trans fatty acids are a by product of hydrogenation • How can we limit intake of these? Figure 06_07 Trans Fatty Acid Food Labels • % Daily Value on Nutrition Facts label is sum of trans and saturated fatty acids • Quantity of trans fatty acids • “Trans fat free” has no more than 0.5 g each of trans or saturated fat • Read the food label and look for hydrogenated or partially hydrogenated oils, or trans fatty acids Trans Fatty Acids Monounsaturated Fatty Acids • One double bond • Oleic acid (Omega 9) • Olive oil, canola oil, nuts • Rate of CHD low in Mediterranean countries where diet is rich in olive oil • Diet high in MUFA equivalent to low-fat diet in ↓ LDL-C, but does not ↓ HDL-C Monounsaturated Fatty Acid Polyunsaturated Fatty Acids • 2 or more double bonds • Provides essential fatty acids (EFAs) – Omega 3 – Omega 6 • Properties differ between these EFAs Polyunsaturated Fatty Acid Figure 06_11 Essential Fatty Acids • Polyunsaturated fatty acids • Body can only make double bonds after the 9th carbon from the omega end • • Needed for – immune function – vision – cell membranes – production of hormone-like compounds Essential Fatty Acid Needs • Adequate Intake – Approximately 2-4 Tablespoons daily • Deficiency – Unlikely • Toxicity – No upper level set 32 Omega-3 Fatty Acids • Linolenic acid (α-linolenic acid) • Forms eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) • Metabolized to form eicosanoids Omega-3 Fatty Acids • Consumption of large amounts of omega-3 fatty acids decreases the ability of blood to clot • May: – Prevent stroke and heart attacks caused by clots (thrombosis) – Reduce risk of stroke caused by blood clots – Help some chronic inflammatory conditions • Asthma, rheumatoid arthritis, psoriasis Omega-3 Fatty Acids – Recommend – Shellfish intake of ~2 servings of fish/wk – Cold water/fatty fish (salmon, mackerel, sardines, tuna) • Consumption of canola or olive oil vs. other plant oils • Flaxseed oil – 2 tbsp per day • Fish oil capsules – 900 mg per day – Avoid: if have a history of bleeding disorder, on blood thinners Omega-6 Fatty Acids • Linoleic acid • Forms arachidonic acid • Metabolized to eicosanoids • Found in vegetable oils – Corn, sunflower, safflower, soybean oils, nuts, seeds, wheat germ • Only need ~ 1 tablespoon a day Eicosanoids • A group of hormone-like compounds • By-pass the blood stream and work in the area of origin • Regulators of: – – – – – Blood pressure Clotting Immune responses Inflammatory responses Stomach secretions • Prostaglandins, thromboxanes, leukotrienes, prostacyclins, lipoxins Eicosanoids Have Different Effects • Omega-3 eicosanoids, DHA, EPA – ↓ blood clotting – ↓ inflammatory responses – Reduce heart attack – Excess may cause hemorrhagic stroke • Omega-6 eicosanoids; Arachidonic acid – ↑blood clotting – ↑ inflammatory responses • Eicosanoids have different effects on different tissues American Heart Association Recommendations • Total fat: <30% of total calories • Saturated fat: <10% of total calories • Monounsaturated fat: 10% of total calories • Polyunsaturated fat: 10% of total calories • Cholesterol: <300 mg/day Phospholipids • Hydrophobic and Hydrophillic Ends • Functions – Component of cell membranes – Eicosanoid synthesis – Emulsifier • Allows fats/lipids to be dispersed in water – Bile acids • Sources – Synthesized by the body as needed – Built on a glycerol backbone • At least one fatty acid replaced with phosphorus compound – Food: egg yolks (lecithin), wheat germ and peanuts 43 Emulsifier Hydrophilic end (attracts water) Hydrophobic end (attracts lipid) 45 Sterols • Multi-ringed structure, most known is cholesterol • Functions – Bile acids, cell membranes – Precursor of steroid hormones, sex hormones, adrenal hormones, Vitamin D • Sources – Synthesized by the liver – Food: animal origin 46 Lipid Digestion • Mouth – Lingual lipase (inactive until reaches stomach) • Stomach – Gastric lipase (digests primarily SCFAs) – Muscular contractions mix fat with digestive enzymes – Fats generally remain in stomach 2-4 hours Lipid Digestion • Small intestine – Cholecystokinin (CCK) and Secretin • Released due to presence of fat in duodenum • CCK stimulates release of – Pancreatic lipase – Bile (to help emulsify fat) • Secretin stimulates release of – Bicarbonate » Raises pH for activation of lipases Bile • Composed of bile acids, bile pigments, phospholipids (lecithin) • Synthesized from cholesterol in the liver • Function is to emulsify fat – Allows fat to be suspended in watery digestive juices – Large fat globules broken down to smaller ones, surface area for lipase action increases – Micelles are formed Bile • Once used for emulsification, can go through 1 of 2 routes: – Reabsorbed in small intestine and recycled – Binds to fiber in large intestine and excreted • This is how fiber (in particular soluble fiber) helps lower blood cholesterol levels Enterohepatic Circulation End Products of Lipid Digestion • • • • Glycerol Fatty acids Cholesterol Lecithin Lipid Absorption • Micelles – Emulsified fat droplets – Absorbed across intestinal mucosal cells by diffusion • Distal duodenum, jejunum • End products of dietary lipid digestion – Repackaged into chylomicrons – Released into lymph system • Bile salts absorbed in the ileum – Returned to liver via portal vein to be reused – “Enterohepatic circulation” Emulsification Lipid Transport • Water (blood) and oil (fat) are incompatible • Unique system of fat transportation needed for lipids to travel in bloodstream Lipid Transport • Lipoproteins – Transport lipids through bloodstream – Composed of: • Triglycerides, protein, phospholipids, cholesterol – 4 different types • Chylomicrons • VLDL (Very-low density lipoprotein) • LDL (Low density lipoprotein) • HDL (High density lipoprotein) Lipoprotein Chylomicrons • Large in size • Triglyceride–rich (80-90% TG) • Transport dietary (exogenous) fat to cells – High blood concentrations following a meal • Transported via lymph system, enter bloodstream at thoracic duct Chylomicrons • Lipoprotein lipase (LPL) breaks down TGs in chylos • Fatty acids are absorbed by cells (muscle, adipose, etc.) • Chylomicron remnants removed by the liver, broken down, and repackaged into VLDL – At this point, fats are considered ENDOGENOUS • 2-10 hours to clear from bloodstream Dietary Fat Absorption Very-Low Density Lipoproteins • Triglyceride-rich (55-65%) • Transports endogenous fats to cells – Lipids synthesized in liver • Released from liver into bloodstream Very-Low Density Lipoproteins • Lipoprotein lipase (LPL) breaks down TGs in VLDL • Fatty acids are absorbed by cells (muscle, adipose, etc.) • VLDL remnants are removed by liver, broken down, and repackaged into LDL • 10-12 hours to clear from bloodstream Low Density Lipoproteins • Cholesterol-rich (45%) • Transports cholesterol synthesized by liver • Removed from bloodstream via receptors (or scavenger pathway) – Receptors down-regulated with high saturated/trans fatty acid diet • 2-3 days to clear from bloodstream Low Density Lipoproteins Optimal <100 mg/dl Factors that raise LDL • High saturated fat diet • Diet high in trans fatty acids • Low fiber diet • Sedentary lifestyle High Density Lipoproteins • Protein rich (45-50%) • Synthesized by liver and intestine • Picks up cholesterol from dying cells and other sources • Transfer cholesterol to other lipoproteins for transport to liver for excretion • HDL can also transfer directly back to the liver Benefits of High HDL • • • • Removes cholesterol from blood May block oxidation of LDL Reduces risk of heart disease Pre-menopausal women have higher HDL High Density Lipoproteins Desirable >60 mg/dl Factors that raise HDL Low saturated fat diet Replacing saturated fats with Mono - unsaturated fats Exercise 45 minutes 4 times a week Losing excess weight, if overweight Moderate amount of alcohol Lipoproteins Composition of Lipoproteins Metabolism of Lipids • Fatty acids, monoglycerides and other lipids taken up by tissue cells • Can be used in 1 of 4 ways: – Immediate source of energy – Energy storage (adipose) – Incorporation into cell membranes – Used as raw material for synthesis of essential compounds (cholesterol) Lipids as an Energy Source • Hormone sensitive lipase (HSL) – Enzyme found in liver and adipose tissue – Key enzyme for lipolysis of stored fat – Insulin inhibits HSL (inhibits lipolysis) – Glucagon activates HSL (leads to lipolysis) Lipids as Stored Energy • Unlimited capacity for fat storage • Lipoprotein lipase (LPL) – Located in adipose and muscle cells – Facilitates uptake of FA from blood – Excess energy intake • LPL synthesis • fat stored in adipose Health Implications of Fat • Cardiovascular disease – Major cause of morbidity and mortality in US – >500,000 people die every year – ~1.5 million Americans have a heart attack every year • Obesity – Fat is a concentrated source of calories – Abdominal fat associated with risk for DM and HTN • Cancer – High fat diet associated with certain forms of cancer Heart Disease • Cardiovascular Disease (CVD) – Disease of the heart and blood vessels • Coronary Heart Disease (CHD) – Damage that occurs when blood vessels carrying blood to the heart (the coronary arteries) become narrow and occluded – Leading cause of death in US • Myocardial infarction (MI) – Accounts for ~50% of CVD deaths – Major underlying cause is atherosclerosis Development of CHD • When blood flow via coronary arteries is interrupted • Heart attack (myocardial infarction) may result leading to – Irreversible damage to heart muscle – Irregular heart beat or stopped heartbeat – 25% of people do not survive their 1st MI • Cerebrovascular accident (CVA) or stroke – When blood flow to part of brain is interrupted causing part of brain to die Myocardial Infarction (MI) Signs of a Heart Attack • • • • • • • • Intense, prolonged chest pain Shortness of breath Sweating Nausea and vomiting Dizziness Weakness Jaw, neck, shoulder pain Irregular heartbeat Risk Factors for Heart Disease Modifiable • Smoking • Hyperlipidemia – Total Chol >200 mg/dL – Low HDL-C <35 mg/dL – Hight LDL-C • • • • Obesity HTN Physical Inactivity Diabetes Mellitus Non-Modifiable • Age – Male >45 – Female >55 • Male gender • Family history of CHD Other Risk Factors • Serum Homocysteine – Amino acid – High level in blood associated with increased risk of MI – Causes damage to blood vessel wall • Reduce blood level by: – Increasing folate, B6 and B12 intake • Fruits, vegetables, etc. Other Risk Factors • C-Reactive Protein (CRP) – Acute phase protein that increases during systemic inflammation – Levels in blood increase during inflammation – Biochemical marker for CVD National Heart Lung and Blood Institute, Adult Treatment Panel III Guidelines for CHD (2001) LDL Cholesterol <100 100-129 130-159 160-189 >190 Total Cholesterol <200 200-239 >240 HDL Cholesterol <40 >60 Optimal Near optimal Borderline high High Very high Desirable Borderline high High Low High Reduce Your Risk (Primary Prevention) • ↓ dietary saturated fat, trans fatty acid, and cholesterol • ↑ MUFA and PUFA to recommended amounts • ↑ dietary fiber • Maintain healthy weight • Don’t smoke • Alcohol in moderation • Folate intake • Low glycemic index load Secondary Prevention (After a Heart Attack) • Primary prevention techniques • Medication • Megadoses of vitamin E (400-800 IU/day) Therapeutic Lifestyle Changes • • • • • • • • Total Fat SFA MUFA PUFA CHO Protein Cholesterol Fiber 25-35% of total kcals <7% of total kcals Up to 20% “ “ Up to 10% “ “ 50-60% of “ “ 10-20% of “ “ <200 mg/d 20-30 g/d Therapeutic Lifestyle Changes • Other recommendations: – Plant stanols/sterols • 2 g/d – Kcals • To maintain optimal weight, prevent weight gain – Physical activity • Expend at least 200 kcal/d Medical Therapy • Statin drugs – Lipitor, Zocor, Mevacor, etc. – Successful in reducing blood cholesterol • Benecol and Take Control – Plant stanol ester – Cholesterol-lowering effect – Compete with cholesterol in the micelle and reduce absorption of dietary cholesterol Medical Therapy • Surgical Intervention – Angioplasty – Coronary Artery Bypass Graft (CABG) Angioplasty Stent placement CABG surgery