* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Analgesic Drugs
Discovery and development of ACE inhibitors wikipedia , lookup
Toxicodynamics wikipedia , lookup
Drug interaction wikipedia , lookup
Cannabinoid receptor antagonist wikipedia , lookup
Discovery and development of proton pump inhibitors wikipedia , lookup
Discovery and development of cyclooxygenase 2 inhibitors wikipedia , lookup
NK1 receptor antagonist wikipedia , lookup
Discovery and development of angiotensin receptor blockers wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Neuropharmacology wikipedia , lookup
Dextropropoxyphene wikipedia , lookup
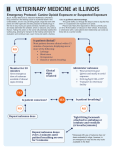
Analgesic Drugs Dr. Chameli Deb Ibn Sina Hospital, Kuwait. Pain Production • • • • • Pain is produced by mechanical or thermal damage to tissues ischemia of somatic or visceral structures spasm of smooth or striated muscles dilatation of blood vessels of at the base of the brain. Substances which produce pain • • • • H+, K+, phosphate ions Acetyl choline, histamine, 5HT, CCK, bradykinin certain prostaglandin and leukotrienes sensory neuropeptides (substance P), neurokinin A (sub K), CGRP • NK enhance hyper excitability of sensory neurons which may induce Painful sensation by light touch or pressure by A fibre. Classification of analgesics • • • • 1. Primary, general or non-specific a. Opioid analgesics - Morphine b. simple analgesics - Aspirin, Ibuprofen 2. Secondary or specific analgesics vasodilators - NTG for ischemia • Carbamazepime for Trigeminal neuralgia • antacids - acid peptic disease Opioid Analgesics • Opiate is specific term to describe drugs derived from Opium poppy (papaver somniferum). • Opioid describes naturally occurring semi-synthetic and synthetic compounds that produce analgesia by combining with Opioid receptor. • Characteristics of Opioids • stereo specific- activity is associated with levo rotatory isomer • Action is antagonised by Naloxone. • Development of highly potent opiod analgesic indicate that receptor mediated mechanism is involved. Location • Spinal Cord - Substantia gelatinosa - arrest of noceptive input. • Brain stem- area postrema, CTZ, tractus solitariusrespiratory control, cough reflex, nausea & vomiting and some autonomic effects • Hypothalamus - temperature & neuro-endocrine function • Medial thalamus- poorly localised deep pain • Limbic system- influence mood & emotional aspect of pain • others - peri-aqueductal grey matter, cerebral cortex & some peripheral site (GIT) Endogenous Opiod peptides » Receptor • • • • Enkephalin - delta Endorphin - mu Dynorphine - kappa Nociceptin - ORL 1(orphan FQ) • Endomorphine 1&2 precursor -pro Enkaphalin -pro opiomelanocortin -pro dynorphine Endogenous peptides are found in spinal cord hypothalamus, pituitary gland, limbic system, sympathetic ganglia, skin, GIT. They mediate a variety of physiological & autonomic functions. Structural classification of Opioid drugs • Naturally occurring -Morphine & codeine • Semi-synthetic Morphine analouge - Diamorphine, Hydrocodeine, Naloxone • synthetic - Meptazinal Pheny piperidine - Pethidine Anilinopiperidine - Fentanyl, Alfentanil, Sufentanil, Remifentanil Diphenylheptanes - Methadone, Dextropropoxyphene Benzomorphan derivatives - Pentazocine, Levorphanol Thebaine derivatives - Buprenorphine Functional classification of Opioid drugs Receptor Agonist Partial agonist mu Buphrenorphine Butorphanol Naloxone Naltrexone Naloxonazine B- Funaltrexamine Nalorphine Pentazocine Nalbuphine Naloxone Naltrexone B-Endorphin Endomorphine Morphine Pethidine Methadone Fentanyl kappa Dynorphin Morphine Pentazocine delta Leu-enkephalin Meta-enkephalin Antagonist Naloxone Naltrindole Mechanism of Action • Opioids bind to mu, delta or kappa receptor and acts via inhibitory G protein. • On pre synaptic terminal of primary nociceptive afferent, inhibition of calcium influx prevents excitatory neuro transmitter release • On post synaptic terminal increased potassium efflux cause hyper polarisation making it less excitable. • Inhibition of Adenyl Cyclase, decrease cAMP and decrease alteration of ion channels. • Activation of descending inhibition by stimulating the cells in PAG which relay to the Raphi Neucli of medulla thence to dorsal horn, reduces nociceptive input. Morphine • Natural alkloid • Phenanthrene derivative • Piperidine skeleton • Amphoteric molecule Action • Analgesia • Sedation - drowsiness, sleep, euphoria - dysphoria in absence of pain EEG - delta rhythm - increase voltage low frequency wave - suppress REM sleep, • Respiratory depression - decrease rate and depth, ventilatory response to Pco2 and the curve shift to the right & slope decrease. Suppression of protective reflexes. • Anti-tussive Cardiovascular System • Bradycardia • Hypotension • Vasodilatation due to decreased sympathetic drive vagal effect, no myocardial depression histamine release Histamine release - causes vasodilatation, hypotension, bronchospam, itching (nasal), pruiritis. Atropine partially antagonises these effects. Ocular miosis is caused by stimulation of Edinger Westphal nucleus, depression of supra nuclear pathway or central symphathetic activity. Pinpoint pupil are characterstic of morphine poisoning GIT • • • • Opioids cause: delayed gastric emptying constipation decreased secretions increased biliary tone Hormonal • increased ADH secretion • decreased release of ACTH, Prolactin and Gonadotrophic hormones Muscle rigidity may involve inhibition of Dopamine release & GABA pathway. True convulsions rarely occurs. Others - constipation, spasm of ureter, bladder & uterus Pharmacokinetics- Morphine • Morphine is a weak bases- highly ionised in stomach. • Bio-availability 15-50%. • Extensively metabolised by liver to Morphine 6 glucuronide & Morphine 3 glucuronide. Undergo entero-hepatic circulation. • CNS level lags behind behind the plasma level. Pharmacokinetics of opioids • Weak bases pK - 6.5 - 9.3 • Considerable first pass • • • • / lipid solubility Distribution depends on --------- degree of ionisation \ plasma protein binding predominantly inactivated in the liver by conjugation to active or inactive metabolites & are excreted in the urine or bile Most Opiods have a volume of distribution several times greater than total body water. Total clearance similar to hepatic blood flow. Entero- hepatic circulation is present for Morphine metabolites. May accumulate & cause respiratory depression. Accumulation of Norpethidine with half life 5 times that of Pethidine. May cause agitation & convulsions. Tolerance and Dependence Tolerance occurs for all opioid effects except constipation & miosis. Mechanism- decreased production of endogenous opiods down regulation of receptors Glutamate mediated transmission via NMDA Dependence - physical & psychological withdrawal symptoms - nausea, vomiting, diarrhoea - restlessness, insomnia - pupillary dilation - fever, sweating , lacremation - severe muscle cramps symptoms are maximum at 2 days and lasts for 8-10 days, but some residual symptoms lasts for several weeks. Pharmacokinetics Drug Lipid solu. Vol. Of dist Clearance t1/2 pKa % ionised prot. Binding ----------------------------------------------------------------------------------------------------------------------------- -Morphine 1 3.5 15 3 7.9 76 25-35 Pethidine 30 4 12 4 8.7 95 40-50 Diamorphine 200 0.6-0.8 31 2-3.5 7.8 ---- ---------- Fentanyl 580 4 13 3.5 8.4 91 80 Alfentanil 90 0.8 6 1.6 6.5 11 90 Sufentanil 1285 2.9 0.75 2.5 8 ---- 92 Remifentanil 50 0.4 50 0.06 7.1 35 70 Tramadol 1 3.1 6 5 4.5 0.1 Naloxone ---- 2 25 1 --- ------- --------45 Diamorphine - Diacetyl Morphine (Heroin) • Pro-drug • MAM • 1.5 - 2 times more potent Codeine (3 - Methyl Morphine) • pro drug • higher bio-availablity. • less effective against pain. 10% metabolised to parent drug by CYP 2 D6. • Used in head injury, combined with NSAID’s, anti-diarrhoeal prepartion & as an anti-tussive. Papaveretum - semi-synthatic hydrochloride mixture of natural alkloids. Morphine + Codeine + Papaverine + Noscapine. Phenylpiperidine derivatives • Pethidine, Fentanyl, Alfentanil, Sufentanil, Remifentanil & Tramadol • Except Pethidine others have similar pharmacokinetic properties. • They are pure mu agonist & highly lipophylic. • Highly potent intravenously and have faster onset of action. • Shorter duration of action ( context sensitive half life is prolonged except Remifentanil). • Minimal CVS side effects except some bradycardia. Effectively attenuates the response to larngoscopy. • All cause chest wall rigidity & respiratory depression. • Metabolised mainly in liver except Remifentanil. Clearance is largely unaffected by renal disease, but prolonged in cirrhosis. • Concomitant use with MAOI is contraindicated. Pethidine • Pethidine has anti cholinergic property - tachycardia and less miosis. • orally absorbed • less potent • elimination half life of metabolites increase with renal dysfunction. Pure Opioid antagonist Naloxone • N-allyl derivative of Oxymorphone • pure Opioid antagonist. Has high affinity for mu receptor. • No intrinsic activity • Naloxone reverses the respiratory depression & analgesia of Opioids and precipitate withdrawal in addicts. • Naloxone reversal usually lasts for 30-45 min. So repeat dosage may be needed to sustain the effect for reversal of respiratory depression. Also alleviate pruritis & urinary retention symptoms. Naltrexene • longer acting. Orally effective due to low first pass. T1/2 -8 hrs. • It is used as maintenance therapy in detoxified addicts. Spinal Epidural Opiods Advantages • • • • low dosage prolonged analgesia no hpotension no motor block Disadvantages • respiratory depression • pruritis • urinary retention NSAID s’ • Heterogeneous class of drugs with common anti inflammatory, analgesic & antipyretic properties. • Mechanism of action - by inhibition of enzyme Cyclo Oxygenase which reduces PG synthesis. • PGs’ are part of a large family of unsaturated fatty acids present in all organs. They are involved in modulation of pain at the periphery & central sites. • PGs’ sensitise primary nerve ending to analgesic action of agents. • Cyclo Oxgenase is thought to exist as two iso enzymes. • Cox -1 (constitutive) is important to physiological homeostasis • Cox -2 (induced) when tissues are exposed to inflammatory reaction. Synthesis of Prostaglandins Membrane Phospholipids | PLA2 Inactive metabolite ------Archidonic Acid --------------Leukotrienes | | |PG synthetase | | (COX) LTC4 & LTD4 Cyclic Endoperoxidase Platelet / Throboxane / synthetase / / Tx A2 | Tx B2 | Mast cell | | PG2 & PgF2 alpha \Vs. Endothelium \ Prostacyclin synthetase \ \ Prostacyclin PG I2 Classification of NSAIDs • • • • • • • • Salicylic acid derivatives. e.g. aspirin para-Aminophenol derivatives, e.g. paracetamol Arylpropionic acids, e.g. ibuprofen indole and indene acetic acids, e.g. indomethacin Heteroaryl acetic acids, e.g. diclofenac, ketorolac Anthranilic acids (fenamates), e.g. mefenamic acid Enolic acids, e.g. piroxicam, phenylbutazone Alkanones, e.g. nabumentone Pharmakokinetics of NSAIDs • • • • weak organic acids (pKa 3-5) rapidly absorbed orally low first pass & high oral bioavailablity highly protein bound & have the potential to displace other drugs from plasma proteins. So potentiating the effects of these drugs, e.g. oral anticoagulant, anticonvulsant, Lithium, oral hypoglycaemic agents. • low volume of distribution. • In general NSAIDs are eliminated by hepatic bio-transformation, followed by renal excretion Clinical effects of NSAIDs • The ubiquitous nature of PGs in the maintenance of normal homeostasis explains their diverse range of effects. CNS: NSAIDs are thought to be primarily peripherally acting drugs due to their protein binding, low lipophilicity & polar nature . • provide analgesia for moderate to severe pain • various degree of opiod sparing effect of upto 60% • adverse effects include dizziness, depression, depression, confusion & seizures Respiratory System: • Bronchospasm in susceptible individuals. • Various hypersensitivity reaction, urticaria, rashes & angiooedema have been reported Clinical effects of NSAIDs GIT • causes dyspepsia, gastroduodenal erosions, ulcerations, perforation & diarrhoea. • GI damage is common in - women, age > 60 yrs, pr. h/o of peptic ulcer, smoker & alcohol ingestion. • co-administration of PG E2 analogue, Misoprostol may be effective in preventing ulcerations. Renal • NSAIDs impair renal function & may cause acute renal ischaemia >> ATN >> Renal failure. • Risk factors - elderly, dehydration, hypovolaemia, hypotension, cardiac failure, cirrhosis & co administration of ACE inhibitors & diuretics. • Analgesic Nephropathy is a severe & often irreversible form of NSAID induced renal toxicity mostly due to long term consumption leading to ch. Nephritis & Renal papillary necrosis. Clinical effects of NSAIDs Haematologcal • NSAIDS interfere with platelet aggregation. • Coagulation time is not affected & bleeding time remains within normal range. • Bone marrow dyscrasias can occur. Antipyretic effect is a consequence of central prostaglandin inhibition in hypothalamus. Reset the thermostat at higher level. Anti inflammatory Other effects: some NSAIDs delay the closure of Ductus Arteriosus in neonate if used in pregnancy in some CDH to buy time before surgical correction. Aspirin • Rapidly absorbed from the stomach • 50% potent & toxic than Sodium salicylate. • On absorption rapidly hydrolysed to salicylate ions by esterase enzymes. • Mainly metabolised in liver to Salicylic acid & Glucuronic acid. • 60-90% is found in urine as free form when urine is alkaline. • 70% 0f patients on Aspirin lose 5-10 ml of blood per day. • Aspirin induced asthma affects 10-20% of adults with asthma & can be fatal. • Aspirin interferes with platelet aggregation & adhesion by irreversible inhibition of Cox & the effect last for the life time of platelets (7-10 days). • As low as 75 mg/day has been shown to reduce TIA, secondary MI & has been used following CABG, angioplasty. Aspirin • Salicylism: This is a syndrome of Tinnitus, dizziness, deafness, sweating, hyperventilation, nausea & vomiting due to chronic ingestion at large doses. When blood level is 300 ug/ml or more. • Aspirin is contraindicated in children <12 years (except for Juvenile Arthritis) due to malignant rise in ICP following acute viral illness. Mortality 20-40%. • Overdose of Aspirin cause complex acid base imbalance. Respiratory alkalosis by direct stimulation of respiratory centre. Respiratory acidosis Metabolic acidosis • In children hyperventilation is rare & usually present with respiratory depression( metabolic & respiratory acidosis). • Treatment - includes gastric lavage, forced alkaline diuresis, haemodialysis & charcoal haemoperfusion. Selectivity of action Drug Aspirin < 3 gm/day > 3 gm/day Paracetamol Phenylbutazone Indomethacin Ibuprofen Diclofenac Ketorolac Analgesic + +++ ++ + + + + +++ Antipyretic ++ +++ ++ + + + + + Anti inflammatory -++ -+++ +++ + +++ + Metabolism of Paracetamol 1-5% PCM ---------------------------->Toxic metabolite / \ (N-acetyl-paramino-benzoquinonine) / \ /\ 60% / \ 35% / \ Glutathione / \ / \ / / \ / \__SH group / \ / \ \ Gluoronide Sulphate / \ N-actely cysteine conjugate conjugate / \ / \ Hepatocellular conjugated & excreted damage Treatment - Paracetamol toxicity • • • • • • N-acetyl cysteine (12-15 hours) Methionine Cysteamine Gastric lavage < 4 hrs. Vit. K & other clotting factors Symptomatic care Specific Analgesics • Migraine --------------------> 5HT agonist, Ergot alkaloids, NSAIDs’ • Trigeminal neuralgia ----> Carbamazepine • Paget’s disease -------------> Calcitonin • UMN lesion torticollis ----> Baclofen Benodeanpin • Vasospasm,ischemia -----> Vasodialator