* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download DRUG INTERACTIONS
Discovery and development of direct thrombin inhibitors wikipedia , lookup
Discovery and development of non-nucleoside reverse-transcriptase inhibitors wikipedia , lookup
Discovery and development of neuraminidase inhibitors wikipedia , lookup
Polysubstance dependence wikipedia , lookup
Compounding wikipedia , lookup
Orphan drug wikipedia , lookup
Discovery and development of proton pump inhibitors wikipedia , lookup
Theralizumab wikipedia , lookup
Drug design wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
Drug discovery wikipedia , lookup
Psychopharmacology wikipedia , lookup
Pharmaceutical industry wikipedia , lookup
Prescription costs wikipedia , lookup
Neuropharmacology wikipedia , lookup
Pharmacognosy wikipedia , lookup
Pharmacokinetics wikipedia , lookup
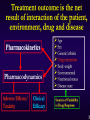
Prof Lukman Hakim PhD Department of Pharmacology and Clinical Pharmacy Faculty of Pharmacy, Gadjah Mada University References for further reading 1. 2. 3. 4. 5. Koda-Kimble MA & Young LY (1998) Hansten and Horn’s Managing Clinically Important Drug Interactions, Applied Therapeutics, Inc, Vancouver Koda-Kimble et al (2007) Handbook of Applied Therapeutics, 8th ed, Lippincott Williams & Wilkins, Philadelphia Mozayani A & Raymon LP (2004) Handbook of Drug Interactions- A Clinical and Forensic Guide, Humana Press, New Jersey Rodrigues AD (2002) Drug-Drug Interactions, Taylor & Francis, New York Stockley IH (1994) Drug Interactions, 3rd ed, Blackwell Science, London Web sites for more learning tools www.arizonacert.org (drug interactions) www.drug-interactions.com (P450-mediated drug interactions) www.torsades.org (drug-induced arrhythmia) www.penncert.org (antibiotics) www.dcri.duke.edu/research/fields/certs.html (cardiovascular therapeutics) www.sph.unc.edu/healthoutcomes/certs/index.htm (therapeutics in pediatrics) www.uab.edu (therapeutics of musculoskeletal disorders) Occurence of drug interactions In Vitro In Vivo (in patients) : Clinically expected or unexpected Clinically observed or undetected Clinical effect can be severe or light In Vitro drug interactions Drugs Interactant Result Ceftriaxone sodium Lactated Ringer's solution Ca-Ceftriaxone precipitate Daptomycin Dextrose solution Daptomycin precipitate Daptomycin 0.9% saline solution Lactated Ringer's solution Compatible Piperacillin-tazobactam Acyclovir Particle formation Amphotericin B Flocculent Mitomycin Blue colour Cefepime Cefepime degrades up to 25% Theophylline David W. Newton (2009) Am J Health-System Pharm. 66(4):348-357 Thilo Bertsche et al (2008) Am J Health-Syst Pharm. 65(19):1834-1840 Contribution of Drug Interactions to the Overall Burden of ADRs Drug interactions represent 3–5 % of in-hospital ADRs Drug interactions are an important contributor to number of ER visits and hospital admissions Leape LL et al. JAMA 1995;274(1):35–43 Raschetti R et al. Eur J Clin Pharmacol 1999;54(12):959–963 Drug may interact with 1. Another drug(s) : a. Synthetic drugs b. Herbal or traditional medicines 2. Food and drinks 3. Pollutants : insecticides, herbicides, smoke of tobacco, exhaust, industries Pasien yang berisiko mengalami efek buruk interaksi obat 1. Aplastic anemia 2. Asthma 3. Cardiac arrhythmia 4. Critical care/intensive care patients 5. Diabetes 6. Epilepsy 7. Hepatic disease 8. Hypothyroid Obat-obat yang potensial berinteraksi 1. Autoimmune disorders 2. Cardiovascular disease 3. Gastrointestinal disease 4. Infection 5. Psychiatric disorders 6. Respiratory disorders 7. Seizure disorders 10 faktor yang berkaitan dengan interaksi obat Jumlah dan jenis obat yang digunakan Jalur pemberian Kepatuhan pasien Durasi penggunaan Dosis/kadar obat Bioavailabilitas rendah Kisar Terapi Sempit Masalah non-linearitas Saat dan urutan penggunaan obat Fraksi termetabolisme Drugs with Narrow Therapeutic Window Examples : Aminoglycoside antibiotics : gentamicin, tobramycin Anticoagulants : warfarin, heparins, high protein bound Aspirin (salicylate derivatives), high PB Carbamazepine : enzyme inducer Conjugated estrogens : OC pills, enzyme inducers Cyclosporine : immunosupressant Digoxin : cardiac stimulant/tonic Esterified estrogens : OC pills, enzyme inducers Hypoglycemic agents : shock hypoglycemic ? Levothyroxine Lithium Phenytoin : nonlinear pharmacokinetics Procainamide : heart arrhythmia Quinidine : heart arrhythmia Theophylline (aminophylline) Tricyclic antidepressants Valproic acid Pharmacokinetic Drug Interactions : Absorption Alteration Drug binding in GI tract GI motility GI pH Action Iron may chelate ciprofloxacin, resulting in decreased absorption Increased GI motility caused by metoclopramide may decrease cefprozil absorption GI alkalinization by omeprazole may decrease absorption of ketoconazole GI flora Decreased GI bacterial flora caused by an antibiotic admin could decrease bacterial production of vitamin K augmenting anticoagulant effect of warfarin Drug metabolism in wall of intestine MAO in the wall of GI tract may be inhibited by MAO inhibitors resulting in increased blood pressure to phenylephrine In the GI Tract Sucralfate, some milk products, antacids, and oral iron preparations Omeprazole, lansoprazole, H2-antagonists Didanosine (given as a buffered tablet) Cholestyramine • Block absorption of quinolones, tetracycline, and azithromycin • Reduce absorption of ketoconazole, delavirdine • Reduces ketoconazole absorption • Binds raloxifene, thyroid hormone, and digoxin FOODS HIGH IN TYRAMINE Ale, Avocados (especially if over-ripe) Bananas Bean pods, lima beans, butter bean Canned Figs, Caviar Cheese (especially aged) Chicken livers Chocolate, Coffee, Cola beverages Fermented meats (salami, pepperoni, summer sausage) Herring (pickled or dry) Raspberries Soy sauce, Sour cream, Tofu Wines (especially red) Yeast preparations, Yogurt May, R.J. (1993). Adverse drug reactions. In J.T. DiPiro et al (Eds.), Pharmacotherapy: A Pathopysiologic approach (2nd ed., p. 71). Norwalk , CT, Appleton & Lange Drugs Affecting Absorption Mechanism of Action Object Drug Result Cholestyramine Binding agent Acetaminophen, diclofenac, digoxin, glipizide, furosemide, iron,lorazepam, methotrexate, metronidazole, piroxicam Decreased absorption Colestipol Binding agent Carbamazapine, diclofenac, furosemide, tetracycline, thiazides Decreased absorption Desipramine Decreased GI motility Phenylbutazone Decreased absorption Cytochrome P450 Isoforms CYP1A2 CYP3A CYP2C9 CYP2C19 CYP2D6 Enzyme CYP 2C9, 2C19 dan 2D6 dapat mengalami polymorphisme pada subyek (pasien) – terjadi pengurangan aktivitas metabolisme Terfenadin dan Astemizol berinteraksi dengan: - Antifungal imidazol (eg. ketokonazol, flukonazol) - Inhibitor CP-450 (eg ketokonazol, flukonazol, simetidin) menyebabkan aritmia jantung Terfenadine, cisapride dan astemizol masih dijual di Indonesia Terfenadin dan Astemizol telah dilarang di US market (1998/99) karena kasus interaksi obat Astemizole vs Erythromycin Erythromycin and astemizole can cause QT interval prolongation and cardiac arrhythmia due to astemizole Risk factors : Not specific Related drugs: Troleandomycin, clarithromycin and terfenadine may also inhibit astemizole metabolism Management: Avoid combination Use loratadine or cetirizine instead of astemizole Certirizine, fexofenadine, loratadine = non-sedating antihistamines Hansten & Horn (1998) p. 47 Astemizole vs Fluvoxamine Fluvoxamine inhibits astemizole metabolic enzyme and increases Cp of astemizole leading to cardiac arrhythmia Risk factors : Not specific Related drugs : Terfenadine, fluvoxamine and astemizole are metabolized by CYP3A4 Management: Avoid combination Use loratadine or cetirizine instead of astemizole Hansten & Horn (1998) p. 48 Astemizole vs Ketoconazole Ketoconazole can increase Cp astemizole leading to QT interval prolongation and cardiac arrhythmia due to astemizole Risk factors : Not specific Related drugs : Miconazole, itraconazole, and fluconazole may also inhibit astemizole metabolism. Terfenadine concentrations are increased with the antifungal agents Management : Avoid combination Use loratadine or cetirizine instead of astemizole Hansten & Horn (1998) p. 48 CYP3A Inducers Carbamazepine Phenytoin Phenobarbital Morphine Rifampin Rifabutin St. John’s wort Various herb’s extracts versus CYP 2D6 and 3A4 activities Ginkgo biloba extract (120 mg, 2x a day, PO; 14 days). Siberian Ginseng extract (485 mg, 2x a day, 14 days) Saw Palmetto extract (320 mg/day, 14 days) The valerian supplement contained a total valerenic acid content of 5.51 mg/tablet (every night, 14 days) Garlic extract (3 x 600 mg twice daily) for 14 days A decaffeinated green tea (GT; Camellia sinensis) extract (4 capsules/day, 14 days). Each GT capsule contained 211 +/- 25 mg of catechins and <1 mg of caffeine against 30 mg dextromethorphan (CYP 2D6 activity) and 2 mg alprazolam (CYP 3A4 activity) did not affect elimination of the two drugs in 11 human volunteers Proportionality of drug metabolizing enzymes Most drug-metabolizing enzymes exhibit clinically relevant genetic polymorphisms. Essentially all of the major human enzymes responsible for modification of functional groups [phase I reactions] or conjugation with endogenous substituents [phase II reactions] exhibit common polymorphisms at the genomic level. Enzyme polymorphisms that have already been associated with changes in drug effects are separated from the corresponding pie charts. ADH, alcohol dehydrogenase; ALDH, aldehyde dehydrogenase; CYP, cytochrome P450; DPD, dihydropyrimidine dehydrogenase; NQO1, NADPH:quinone oxidoreductase or DT diaphorase; COMT, catechol O-methyltransferase; GST, glutathione Stransferase; HMT, histamine methyltransferase; NAT, Nacetyltransferase; STs, sulfotransferases; TPMT, thiopurine methyltransferase; UGTs, uridine 5'-triphosphate glucuronosyltransferases. Breakdown of Genotyping and Phenotyping in FDA Survey Others 22.9% Receptors 7% Pgp 4.3% CYP 2D6 PhaseII 11.4% 72.9% CYP1A2 7.1% CYP3A4/5 14.3% CYP2C9 4.3% CYP2C19 14.3% • Genotyping and phenotyping performed in some submissions • Phase II enzymes measured: NAT-2, UGT, GSTM1, etc • Receptors: Dopamine, 5-HT, beta-adrenergic, alpha-1 adrenergic, potassium channels, etc • Others: HMC, CETP, ACE, alpha-reductase, AAG, CYP2B6, glyceraldehyde 3 -phosphate dehydrogenase, ApoE etc. Pharmacogenetics and Drug Metabolism Same dose but different plasma concentrations Patient A GCCCGCCTC Wild type Wild type Concentration CYP450 Time GCCCACCTC Mutation CYP450 Mutation Concentration Patient B Time Cytochrome P450 2D6 Absent in 7 % of Caucasians 1–2 % non-Caucasians Hyperactive in up to 30 % of East Africans (Ethiopia) Catalyzes primary metabolism of: Codeine (prodrug), Dextro-methorphan Many -blockers Many tricyclic antidepressants Inhibited by: Fluoxetine, Paroxetine (strong inhibitors) Haloperidol Quinidine Aklillu E et al. J Pharmacol Exp Ther 1996;278(1):441– 446 Scientific Basis for Using Pharmacogenetics Top 27 drugs frequently cited in ADR reports 59% (16/27) metabolized by at least one enzyme having poor metabolizer (PM) genotype 38% (11/27) metabolized by CYP 2D6 mainly drugs acting on CNS and cardiovascular systems, including nortriptyline Phillips et al, JAMA, 286 (18), 2001, Inherited Activity of CYP 2D6 and Nortriptyline Dosing Nortriptyline: 25-300 mg EM PM Dose (mg) IM 140 120 100 80 60 40 20 0 Doses need for equivalent exposure PM Nortriptyline Plasma Levels IM EM Phenotype Consequences: discontinue medication (ADR, lack of efficacy), delay to relief of symptoms (suicide), premature switch to other medications Cytochrome P450 2C9 Absent in 1 % Caucasians and African-Americans Primary metabolism of : Most NSAIDs (incl COX-2 inhibitors : Celecoxib, Rofecoxib) S-warfarin (active form) Phenytoin Inhibited by : Fluconazole Cytochrome P450 2C19 Absent in 20–30 % of Asians 3–5 % Caucasians Primary metabolism of : Diazepam Phenytoin Omeprazole Tricyclic antidepressants Clopidogrel (prodrug) Inhibited by : Omeprazole Isoniazid Ketoconazole Cytochrome P450 2C19 Absent in 20–30 % of Asians 3–5 % Caucasians Primary metabolism of Clopidogrel (antiplatelet) Clopidogrel metabolized by CYP2C19 to active metabolite (ADP receptor ; P2Y12). Clopidogrel may cause severe GI bleeding. Guideline : Clopidogrel is combined with PP Inhibitors to minimize bleeding. Inhibited by Proton-pump inhibitors : Omeprazole = Esomeprazole > Lansoprazole > Pantoprazole > Rabeprazole Cytochrome P450 1A2 Induced by smoking tobacco Catalyzes primary metabolism of : Theophylline Imipramine Propranolol Clozapine Inhibited by : Many fluoroquinolone antibiotics Fluvoxamine Cimetidine Drug-Food Interactions Tetracyclines and milk products Warfarin and vitamin K-containing foods* Grapefruit juice Fam Brassicaceae (Cruciferous) * Foods and Products High in Vitamin K Alfalfa tablets Broccoli Brussels sprouts Cabbage Cauliflower (raw) Green leafy vegetables (spinach, collard greens) Green tea Liver Soybean Vegetable oils (canola, soybean) Watercress DRUGS THAT INTERACT WITH GRAPE FRUIT JUICE Benzodiazepines : midazolam, diazepam, triazolam Cytotoxic drugs : cyclosporine, tacrolimus, sirolimus Dyhydropyridine Calcium-channel blockers : amlodipine, felodipine, nifedipine, nisoldipine, nitrendipine, verapamil Theopylline 17β-estradiol Statins : simvastatin, lorvastatin, atorvastatin Antidepressants : sertraline, buspirone, clomipramine Antiepileptics : carbamazepine Antiretroviral agents : saquinavir, indinavir Antiarrhythmics : amiodarone Misce : methadone, sildenafil GFJ increases bioavailability for felodipine by 200%, nifedipine 57% and verapamil by 36%. Inhibition of P-glycoprotein increases bioavailability of drugs. GFJ : enzyme and P-glycoprotein inhibitor South Med J. 2009;102(3):308-309. Hours after Dose Hours after Dose Effects of grapefruit juice on felodipine pharmacokinetics and pharmacodynamics. Dresser GK et al Clin Pharmacol Ther 2000;68(1):28–34 Effect of grape fruit juice on talinolol in rats Cmax (ng/mL) AUC (ug.min/mL) S R S R Control 77.5 79.5 19.3 22.2 GFJ 163.6 163.0 29.9 30.1 • GFJ administered together with a racemic 10 mg/kg (po) in rats • GFJ did not change T1/2 elimination of talinolol Spahn-Langguth & Languth - Eur J Pharm Sci. 2001 Feb;12(4):361-7 Grape fruit juice reduces talinolol bioavailability in humans Pharmacokinetics of talinolol (50 mg, PO) was determined with water, with 1 glass of GFJ (300 mL), and after repeated GFJ (900 mL/d, 6 days) in 24 healthy white volunteers Results : A glass or repeated administration of GFJ : - decreases talinolol AUC, Cmax, and Fel (p < 0.001) decreases bioavailability of talinolol. - does not affect CLr, T1/2 elimination, Tmax. Schwarz et al - Clin Pharmacol Ther. 2005 Apr; 77(4): 291-301 Grape fruit juice vs oral digoxin Digoxin: a P-glycoprotein substrate, not metabolized by CYP 3A4. 7 subjects received a single dose of digoxin 1mg with water or GFJ (3x/day, 5 days) before digoxin admn to maximize any effect on P-glycoprotein. • GFJ reduces digoxin absorption rate constant and increases absorption lag time (p<0.05). • GFJ does not affect Cmax, AUC, T1/2 elim, or CLr digoxin. • Inhibition of intestinal P-glycoprotein by GFJ does not play an important role in drug interactions. Parker et al - Pharmacotherapy. 2003 Aug;23(8):979-87 Daya analgetik parasetamol sebelum dan setelah pemberian brokoli 7-kali pada mencit jantan BALB/C 1. Parasetamol mempunyai daya analgetik 54, 74 % 2. Brokoli menaikkan % daya analgetik parasetamol Daya analgetik salisilat sebelum dan setelah pemberian brokoli 7-kali mencit jantan BALB/C 1. Salisilat mempunyai daya analgetik 56,84% 2. Brokoli menaikkan % daya analgetik salisilat Onset dan durasi fenobarbital sebelum dan setelah pemberian jus brokoli 7-kali pada mencit jantan 1. Brokoli memperlama onset fenobarbital tetapi tidak signifikan (P > 0,05) 2. Brokoli mempercepat durasi fenobarbital (P <0,05) Chlorpropamide vs Ethanol Excessive ethanol intake may lead to hypoglycemia. An “antabuselike reaction” may occur in patients taking sulfonylureas. Risk factors : Not specific (can be to anyone/any case) Related drugs : Insulin and other oral hypoglycemic agents, including tolbutamide, cause hypoglycemia. Taking phenformin may develop lactic acidosis when consuming ethanol Management : Avoid combination. Hansten & Horn (1998) p. 99 Cigarette smoking vs Oral contraceptive Risk of OC-induced adverse cardiovascular events is increased by smoking Risk factors: Women aged > 35 years old are at greater risk Smoking > 15 cigs/day places women at greater risk Management: Avoid combination. Women on OC are adviced not to smoke, or use another contraception method Hansten & Horn (1998) p. 107 Drug-Herbal Interactions St John’s Wort Ginkgo biloba Kava Garlic Izzo and Ernst (2009) Adis data information BV After St. John’s Wort Mean plasma concentration time course of indinavir. Pengaruh SJ Wort terhadap Digoxin, Fenoxfenadine, Irinotecan : memodulasi Pglycoprotein kadar obat ↓ Cyclosporin, OC pills, Ritonavir, Venlafaxine : induksi CYP3A4 & modulasi Pgp kadar obat ↓ Alprazolam, Amitriptyline, Imatinib, Indinavir, Midazolam, Omeprazol, Simvastatin, Tacrolimus, Verapamil : induksi CYP3A4. Warfarin : induksi CYP2C9 Ginkgo biloba (40-60 mg; 2x sehari; 2-3 bulan) Efek: antioksidan, menghambat agregasi platelet (ginkgolide = inhibitor PAF), menyembuhkan Alzheimer Efek samping : Perdarahan okular & intraserebral Interaksi Obat : next slide Effect of Ginkgo biloba on various drugs Drugs Effect Carbamazepine Valproic acid High dose GB decreases anticonvulsant effect Aspirin, clopidogrel, dipyridamole, heparin, ticlopidine, warfarin. Anticoagulation increases Cylosporine GB protects cell membranes from damage (beneficial effect) Phenelzine , tranylcypromine GB enhances antidepressant effect of MAO (serotonin reuptake) inhibitors Kava (Piper methysticum) Zat aktif : kavapiron Efek : penenang, sedatif ES : disorientasi, gangguan kendali otot Penggunaan kronis : gangguan kimia darah, hipertensi paru, nafas pendek, mata merah, berat badan turun Interaksi obat : CNS depressants, L-dopa, nembutal, barbiturat, Xanax => efek aditif Izzo and Ernst (2009) Adis Data Garlic Drugs Indications Clinical results Chlorpropamide Diabetes mellitus Hypoglycemia Fluindione (co-meds : enalapril, furosemide, pravastatin) Chronic atrial fibrilation Decreased anticoagulation Warfarin Not reported Increased anticoagulation Dextromethorphan Debrisoquine Healthy subjects; CYP2D6 No effect on elimination Alprazolam, Midazolam Docetaxel Healthy subjects; CYP3A4 No effect on elimination Ritonavir 400-600 mg bid HIV infection Severe GI toxicity Izzo and Ernst (2009) Adis Data Drug-Drug Interactions: A Stepwise Approach 1. Take a medication history 2. Remember high risk patients • Any patient taking 2 medications • Anticonvulsants, antibiotics, digoxin, warfarin, amiodarone, etc 3. Check pocket reference 4. Consult pharmacists/drug info specialists 5. Check up-to-date website • www.epocrates.com*