* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download powerpoint Part 1
Survey
Document related concepts
Transcript
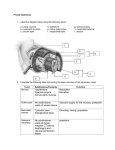
Lecture 8 The Digestive System Part I Digestive System • Two groups of organs – Alimentary Canal – Assessory organs • Tuesday (Today) – Gross and histological anatomy of organs and their function • Thursday – Chemical process, and hormona regulation, of digestion Alimentary Canal • Gastrointestinal or GI tract • Mouth to anus – Digests food and absorbs nutrients and water • Includes: Mouth, pharynx, esophagus, stomach, small intestine, and large intestine Accessory Organs • • • • • • Mouth/Teeth/Tongue Gallbladder Digestive glands Salivary glands Liver Pancreas Figure 23.1 Alimentary canal and related accessory digestive organs. Mouth (oral cavity) Tongue* Parotid gland Sublingual gland Submandibular gland Salivary glands* Pharynx Esophagus Stomach Pancreas* (Spleen) Liver* Gallbladder* Transverse colon Small intestine Duodenum Jejunum Ileum Anus © 2013 Pearson Education, Inc. Descending colon Ascending colon Cecum Sigmoid colon Rectum Appendix Anal canal Large intestine Digestion • Six essential activities – Ingestion – Propulsion – Mechanical breakdown – Digestion – Absorption – Defecation Digestive Processes • Ingestion – taking food in the mouth • Mechanical breakdown – increase surface area for digestion enzymes – chewing, mixing with saliva – churning in the stomach – segmentation – constriction or small intenstine Digestive Processes • Propulsion – swallowing (voluntary) and peristalsis (involuntary) – Peristalsis, alternating waves of contraction and relaxation Figure 23.3 Peristalsis and segmentation. From mouth Peristalsis: Adjacent segments of alimentary tract organs alternately contract and relax, moving food along the tract distally. © 2013 Pearson Education, Inc. Segmentation: Nonadjacent segments of alimentary tract organs alternately contract and relax, moving food forward then backward. Food mixing and slow food propulsion occur. Digestive Processes • Digestion – enzymatic breakdown of food into their chemical building blocks • Absorption – passage of digest end products into blood or lymph • Defecation – elimination Histology of the Alimentary Canal • Four basic layers (tunics) – Mucosa – Submucosa – Muscularis externa – Serosa Mucosa • Lines lumen • Functions – Secretes mucus, digestive enzymes, and hormones – Absorbs end products of digestion – Protects against infectious disease • Three sublayers: – epithelium – lamina propria – muscularis mucosae Three Sub layers of Mucosa • Epithelium – Simple columnar epithelium and mucus-secreting cells (most of tract) – Mucus protects digestive organs from enzymes and eases food passage Three Sub layers of Mucosa • Lamina propria – Loose connective tissue – Capillaries for nourishment and absorption – Lymphoid follicles (part of MALT) • Muscularis mucosae: smooth muscle for local movements of mucosa Figure 23.6 Basic structure of the alimentary canal. Intrinsic nerve plexuses • Myenteric nerve plexus • Submucosal nerve plexus Glands in submucosa Mucosa • Epithelium • Lamina propria • Muscularis mucosae Submucosa Muscularis externa • Longitudinal muscle • Circular muscle Mesentery Nerve Artery Gland in mucosa Vein Duct of gland outside Lymphatic vessel alimentary canal © 2013 Pearson Education, Inc. Serosa • Epithelium (mesothelium) • Connective tissue Lumen Mucosa-associated lymphoid tissue Submucosa • External to the mucosa • connective tissue filled with blood and lymphatic vessels, lymphoid follicles, and nerve fibers Muscularis externa • Responsible for segmentation and peristalsis • Inner and outer layers • Inner layer contain sphincter muscles to control food passage from one organ to next Figure 23.6 Basic structure of the alimentary canal. Intrinsic nerve plexuses • Myenteric nerve plexus • Submucosal nerve plexus Glands in submucosa Mucosa • Epithelium • Lamina propria • Muscularis mucosae Submucosa Muscularis externa • Longitudinal muscle • Circular muscle Mesentery Nerve Artery Gland in mucosa Vein Duct of gland outside Lymphatic vessel alimentary canal © 2013 Pearson Education, Inc. Serosa • Epithelium (mesothelium) • Connective tissue Lumen Mucosa-associated lymphoid tissue The Serosa • The outermost layer – Visceral peritoneum The Peritoneum • All ventral body cavities contain slippery serous membranes • Peritoneum of abdominal cavity most extensive Figure 23.5a The peritoneum and the peritoneal cavity. Abdominopelvic cavity Vertebra Dorsal mesentery Parietal peritoneum Ventral mesentery Visceral peritoneum Peritoneal cavity Alimentary Liver canal organ Two schematic cross sections of abdominal cavity illustrate the peritoneums and mesenteries. © 2013 Pearson Education, Inc. Nerve Supply • In-house nerve supply – enteric neurons • Regulates digestive activity by controlling GI tract motility – segmentation and peristalsis and other contractions Functional Anatomy • Mouth and tongue • Salivary glands – cleanses the mouth – dissolves food chemicals for taste – moistens food for a compact bolus – Contains enzymes that begin chemical breakdown • Teeth, Pharynx and Esophagus Saliva • 97-99% water – pH = 6.75-7.00 – enzymes: amylase and lipase – proteins: mucin – helps in innate immunity • lysozymes, IgG and defensins • Produce 1.5 L per day! Esophagus • Flat muscular tube from laryngopharynx to stomach • Pierces diaphragm at esophageal hiatus • Joins stomach at cardial orifice – cardiac sphincter muscle • Collapsed tube when not in use • Movement down esophagus is involuntary Figure 23.12a Microscopic structure of the esophagus. Mucosa (stratified squamous epithelium) Submucosa (areolar connective tissue) Lumen Muscularis externa • Circular layer • Longitudinal layer © 2013 Pearson Education, Inc. Adventitia (fibrous connective tissue) The Stomach • In upper left quadrant; temporary storage; digestion of bolus to chyme • Four parts – Cardial part – Fundus – Body – Pyloric part Four parts of the stomach • Cardial part (cardia) – Surrounds cardial orifice • Fundus – Dome-shaped region beneath diaphragm • Body – Midportion • Pyloric part – Antrum and canal Figure 23.14a Anatomy of the stomach. Cardia Fundus Esophagus Muscularis externa • Longitudinal layer • Circular layer • Oblique layer Serosa Body Lumen Lesser curvature Rugae of mucosa Greater curvature Duodenum © 2013 Pearson Education, Inc. Pyloric sphincter (valve) at pylorus Pyloric canal Pyloric antrum Stomach to duodenum • The pyloric canal terminates at the pylorus • Pylorus is continuous with the duodenum through the pyloric sphincter – controls emptying of stomach Holding everything in place • Two mesenteries (supporting membranes) – Lesser omentum – Greater omentum Figure 23.30b Mesenteries of the abdominal digestive organs. Liver Gallbladder Lesser omentum Stomach Duodenum Transverse colon Small intestine Cecum Urinary bladder © 2013 Pearson Education, Inc. Figure 23.30c Mesenteries of the abdominal digestive organs. Greater omentum Transverse colon Transverse mesocolon Descending colon Jejunum Mesentery Sigmoid mesocolon Sigmoid colon Ileum © 2013 Pearson Education, Inc. Stomach Histology • Contains four tunics (layers) • Modified for function • Four types of gland cells – – – – Mucous Neck Cells Parietal Cells Chief Cells Enteroendocrine Cells Figure 23.15a Microscopic anatomy of the stomach. Surface epithelium Mucosa Lamina propria Muscularis mucosae Submucosa (contains submucosal Oblique plexus) layer Muscularis Circular externa layer (contains Longitudinal myenteric layer plexus) Stomach wall Serosa Layers of the stomach wall © 2013 Pearson Education, Inc. Figure 23.15b Microscopic anatomy of the stomach. Gastric pits Surface epithelium (mucous cells) Gastric pit Mucous neck cells Parietal cell Gastric gland Chief cell Enteroendocrine cell © 2013 Pearson Education, Inc. Enlarged view of gastric pits and gastric glands Gastric Glands • Glands in fundus and body produce most gastric juice • Mucous neck cells – thin, acidic mucus of unknown function • Parietal cells – HCl and Intrinsic factor (Vit B12 absorption) • Chief cells – Pepsinogen and lipases • Enteroendocrine cells – Secrete hormones into lamina propria Figure 23.15c Microscopic anatomy of the stomach. Pepsinogen Pepsin HCI Mitochondria Parietal cell Chief cell Enteroendocrine cell Location of the HCl-producing parietal cells and pepsin-secreting chief cells in a gastric © 2013 Pearson Education, Inc. gland Stomach Filling • Stretches to accommodate incoming food – stomach can stretch without increasing its tension – stress-relaxation response intrinsic to smooth muscle Gastric Motility • Peristaltic waves move toward pylorus at rate of 3 per minute • Basic electrical rhythm (BER) set by enteric pacemaker cells – linked by gap junctions throughout muscularis externa Figure 23.19 Deglutition (swallowing). Pyloric valve closed 1 Propulsion: Peristaltic waves move from the fundus toward the pylorus. © 2013 Pearson Education, Inc. Slide 1 Pyloric valve closed 2 Grinding: The most vigorous peristalsis and mixing action occur close to the pylorus. Pyloric valve slightly opened 3 Retropulsion: The pyloric end of the stomach acts as a pump that delivers small amounts of chyme into the duodenum, simultaneously forcing most of its contained material backward into the stomach. Gastric Emptying • Stomach usually empties completely within four hours – high fat (oily) foods digest more slowly and remain in stomach longer • Chyme entering duodenum cause receptors to activate due to stretch – signals hormones to inhibit acid and pepsin secretion in stomach Small Intestine • Major organ of digestion and absorption • 2-4 m long (7-13ft); from pyloric sphincter to ileocecal valve • Subdivisions – Duodenum (retroperitoneal) – Jejunum (attached posteriorly by mesentery) – Ileum (attached posteriorly by mesentery) Duodenum • Curves around head of pancreas • Bile duct (from liver) and main pancreatic duct (from pancreas) enter at this point – Join at hepatopancreatic ampulla – Enter duodenum at major duodenal papilla – Entry controlled by hepatopancreatic sphincter Figure 23.21 The duodenum of the small intestine, and related organs. Right and left hepatic ducts of liver Cystic duct Common hepatic duct Bile duct and sphincter Accessory pancreatic duct Mucosa with folds Tail of pancreas Pancreas Jejunum Gallbladder Major duodenal papilla Hepatopancreatic ampulla and sphincter © 2013 Pearson Education, Inc. Main pancreatic duct and sphincter Duodenum Head of pancreas Jejunum and Ileum • Jejunum – Extends from duodenum to ileum – About 2.5 m (8ft) long • Ileum – Joins large intestine at ileocecal valve – About 3.6 m (12 ft)long Histology of Small Intestines • Increase surface area of proximal part for nutrient absorption • Circular folds in mucosa and submucosa layers • Villi • Microvilli Figure 23.22a Structural modifications of the small intestine that increase its surface area for digestion and absorption. Vein carrying blood to hepatic portal vessel Muscle layers Circular folds Villi © 2013 Pearson Education, Inc. Lumen Figure 23.22b Structural modifications of the small intestine that increase its surface area for digestion and absorption. Microvilli (brush border) Absorptive cells Lacteal Goblet cell Blood capillaries Mucosaassociated lymphoid tissue Intestinal crypt Muscularis mucosae Duodenal gland © 2013 Pearson Education, Inc. Villus Enteroendocrine cells Venule Lymphatic vessel Submucosa Villi and Microvilli • Epithelial cells, enterocytes, are columnar cells with a dense capillary bed (lacteal) • Microvilli create an appearance of a brush border that also help in aiding digesting – brush border enzymes Figure 23.22c Structural modifications of the small intestine that increase its surface area for digestion and absorption. Absorptive cells Goblet cells Villi © 2013 Pearson Education, Inc. Intestinal crypt Figure 23.23 Microvilli of the small intestine. Mucus granules Microvilli forming the brush border Absorptive cell © 2013 Pearson Education, Inc. Intestinal Crypts • Between villi, the mucosa is studded with intestinal crypts – secretory cells intestinal juices (mucous) • Host of other cell types (discussed 5/9) – Enteroendocrine cells – Intraepithelian lymphocytes – Paneth cells Peyer’s Patches • Aggregated lymphoid nodules located in lamina propria along the intestinal tract • Increasing abundance toward the distal end – larger bacterial load Intestinal Juice • 1-2 L per day • pH close to blood (isotonic) • Enzyme poor – enzymes are bound to brush border for optimal digestion and immediate absorption Liver and Gall bladder • Accessory organs associated with the small intestines • Digestive functions: – Liver: produce bile that breaks down fat (900ml/day) – Gallbladder: storage organ for bile Liver • Largest gland in body • Four lobes—right, left, caudate, and quadrate • Falciform ligament – Separates larger right and smaller left lobes – Suspends liver from diaphragm and anterior abdominal wall • Round ligament (ligamentum teres) – Remnant of fetal umbilical vein along free edge of falciform ligament Figure 23.24a Gross anatomy of the human liver. Sternum Nipple Bare area Liver Falciform ligament Left lobe of liver Right lobe of liver Gallbladder © 2013 Pearson Education, Inc. Round ligament (ligamentum teres) Figure 23.24b Gross anatomy of the human liver. Lesser omentum (in fissure) Left lobe of liver Porta hepatis containing hepatic artery (left) and hepatic portal vein (right) Quadrate lobe of liver Ligamentum teres Bare area Caudate lobe of liver Sulcus for inferior vena cava Hepatic vein (cut) Bile duct (cut) Right lobe of liver Gallbladder © 2013 Pearson Education, Inc. Histology of Liver • The liver is composed of sesame seed-sized structural and functional units called liver lobes – liver cells: hepatocytes • Liver’s main function is to filter and process nutrient, rich blood – central vein running through each lobe Figure 23.25a–b Microscopic anatomy of the liver. Lobule © 2013 Pearson Education, Inc. Central Connective vein tissue septum Figure 23.25c Microscopic anatomy of the liver. Interlobular veins (to hepatic vein) Central vein Sinusoids Bile canaliculi Plates of hepatocytes Bile duct (receives bile from bile canaliculi) Fenestrated lining (endothelial cells) of sinusoids Stellate macrophages in sinusoid walls Portal vein © 2013 Pearson Education, Inc. Bile duct Portal venule Portal arteriole Portal triad Gallbladder • About the size of a kiwi-fruit, on the inferior surface of the liver • Stores and concentrates bile not immediately needed • Muscular wall contracts to expel bile when stimulated Pancreas • Endocrine function – Pancreatic islets secrete insulin and glucagon • Exocrine function – Acini (clusters of secretory cells) secrete pancreatic juice – To duodenum via main pancreatic duct Figure 23.27 Activation of pancreatic proteases in the small intestine. Stomach Pancreas Epithelial cells Membrane-bound enteropeptidase Trypsinogen (inactive) © 2013 Pearson Education, Inc. Trypsin Chymotrypsinogen (inactive) Chymotrypsin Procarboxypeptidase (inactive) Carboxypeptidase Figure 23.26a Structure of the enzyme-producing tissue of the pancreas. Small duct Acinar cell Basement membrane Zymogen granules Rough endoplasmic reticulum Duct cell One acinus © 2013 Pearson Education, Inc. Pancreatic Juice • • • • 1200 – 1500 ml/day pH 8 to neutralize chyme Electrolytes (primarily HCO3–) Enzymes – Amylase, lipases, nucleases and proteases The Large Intestines • Major digestive function Is to absorb remaining water • Unique anatomy – Teniae coli • Three bands of longitudinal smooth muscle in muscularis – Haustra • Pocketlike sacs caused by tone of teniae coli – Epiploic appendages • Fat-filled pouches of visceral peritoneum (unknown function) Regions of Large Intestines • Five Regions – Cecum – Appendix (MALT) – Colon – Rectum – Anal canal Figure 23.29a Gross anatomy of the large intestine. Left colic (splenic) flexure Right colic (hepatic) flexure Transverse mesocolon Transverse colon Epiploic appendages Superior mesenteric artery Descending colon Haustrum Ascending colon IIeum Cut edge of mesentery IIeocecal valve Tenia coli Sigmoid colon Cecum Appendix Rectum Anal canal © 2013 Pearson Education, Inc. External anal sphincter Figure 23.30c Mesenteries of the abdominal digestive organs. Greater omentum Transverse colon Transverse mesocolon Descending colon Jejunum Mesentery Sigmoid mesocolon Sigmoid colon Ileum © 2013 Pearson Education, Inc. Histology • Mucosa layer is simple columnar epithelium – thicker and deeper for increased number of goblet cells for mucous secretion • Mucosa layer of anal canal is stratified squamous epithelium – increase protection against abrasion The Anal Canal • Last segment of large intestine • Muscle Sphincters – Internal anal sphincter— smooth muscle • Involuntary – External anal sphincter— skeletal muscle • Voluntary Motility in Colon • Most contractions of colon; Haustral contractions – Slow segmenting movements for 1 min, every 30 minutes • Occur in ascending and transverse colon – distension of muscle wall regulate contractions Gastrocolic reflex • Activated by presence of food in stomach • Mass movements – long, slow moving and powerful contractile waves the move over entire colon – force contents to rectum Lab Exercise 38 • Do not worry about mouth, tongue or teeth