* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download ASHI U Module Chapter II: DNA Based Testing Section: Application
Bisulfite sequencing wikipedia , lookup
Polycomb Group Proteins and Cancer wikipedia , lookup
Gene expression profiling wikipedia , lookup
Epigenetics of human development wikipedia , lookup
Point mutation wikipedia , lookup
Primary transcript wikipedia , lookup
Cell-free fetal DNA wikipedia , lookup
Nucleic acid analogue wikipedia , lookup
Therapeutic gene modulation wikipedia , lookup
Microevolution wikipedia , lookup
History of genetic engineering wikipedia , lookup
Site-specific recombinase technology wikipedia , lookup
SNP genotyping wikipedia , lookup
Human leukocyte antigen wikipedia , lookup
Designer baby wikipedia , lookup
Vectors in gene therapy wikipedia , lookup
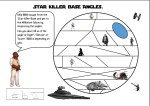
ASHI U Module Chapter II: DNA Based Testing Section: Application Modules Module (H): Killer-cell Immunoglobulin-like Receptor (KIR) Genotyping Authors: Joel Y. Sun, Stanford Hospital and Clinics, [email protected] Laima Gaidulis, City of Hope National Medical Center: [email protected] T U David Senitzer, City of Hope National Medical Center: [email protected] T Date Prepared: 08/23/2006 Date Updated: 07/04/2012 U UT OBJECTIVES Understand KIR components, gene location and standard nomenclature. Be familiar with currently available methodologies for KIR genotyping and understand how to determine the genotype.Understand the steps involved in identification of KIR genes using a simple multiplex PCR-SSP method as an example. Understand and identify the ASHI standards that pertain to the compliance of the assay, and the quality control measures incorporated in the test system. U 2 INTRODUCTION Natural killer (NK) cells are increasingly recognized as an important immune component involved in immune surveillance, anti-infection and alloimmune response. Killer cell immunoglobulin-like receptors (KIRs) are the major receptor cluster expressed on human NK cells and a subset of T cells. A KIR molecule consists of two or three extracellular immunoglobulin-like domains, a transmembrane stem and a long (L) or short (S) cytoplasmic tail (Fig. 1). Standard nomenclature describes these features with a number followed by the letter D for the extracellular domains (2D or 3D), the letter L or S in the third digit for the cytoplasmic tail and a number in the forth digit to distinguish loci (in most cases). The letter P in the third digit refers to pseudogenes. Generally, long tail KIRs transmit inhibitory signals and short tail KIRs transmit stimulatory signals. Some inhibitory KIRs (iKIRs) specifically recognize HLA-A, B or -C allotypes on target cells as iKIR ligands (iKIRLs, Fig.1). The interaction of iKIRs and HLA class I iKIRLs controls NK cell function [Ref. 1-3]. The recognition of KIR and its ligands is a complex issue. For example, it was a consensus that 3DL1 recognizes HLA-Bw4 allotypes but not those HLA-A sharing the same epitope [Ref. 4]. However, a recent study using HLA-A tetramers demonstrated the binding of HLA-A and 3DL1, but the functional implication of this binding was undetermined [Ref. 5]. A full presentation of the knowledge is out of the scope of this module. KIR is another highly polymorphic system, like the notorious HLA system. Its diversity is generated by both gene content (a variation in the number of genes present on individual haplotypes) and allelic variation. The KIR gene cluster is located on chromosome 19q13.4 (Fig. 1). The most common KIR haplotype is haplotype A, defined by the presence of only one short tail KIR 2DS4 and a fixed number of nine KIR genes 3DL3-2DL3-2DP1-2DL1-3DP1-2DL4-3DL1-2DS4-3DL2. Haplotype B harbors more than one short tail KIR (except some very rare haplotypes) and varies greatly in gene content. 3 Some KIR gene loci exist in almost every haplotype and are called framework genes. They are 3DL3 in the centromeric end, 3DP1 and 2DL4 in the middle and 3DL2 in the telomeric end of the KIR gene cluster. The IPD database (http://www.ebi.ac.uk/ipd/kir/index.html) named 614 KIR alleles in the 15 April 2011 TU UT release, and that number is increasing quickly. Most of the allelic variants do not change KIR function. However, some do affect either KIR protein expression or receptor-ligand interaction. For example, the proteins of alleles KIR2DS4*003/4/6-10/12/13, differing from KIR2DS4*001 by a 22bp deletion in exon 5, are transcribed but not expressed on the cell surface due to the absence of a transmembrane and cytoplasmic domain. The frequency of these alleles is very high [Ref. 1, 6]. There is a growing body of literature that has addressed the effects of KIR and its ligand on transplantation (both bone marrow [Ref. 7-9, 24] and solid organ [Ref. 10, 11, 25]), infectious [12] and autoimmune diseases [Ref. 13]. KIR genotyping was widely performed in these studies. 4 Figure 1. Killer Ig-like Receptors (KIRs), their Ligands and Genes Ligand KIR D0, Gene arrangement D1, D2 Haplotypes: A, -S-S- -S-S- 2DL1 -S-S- 2DL2 & 2DL3 HLA-Clys80, Cw*02,04,etc. B1, B2, B3, … 3DL3 2DS2 HLA-Casn80, Cw*01,03,etc. -S-S- 2DL2/3 HLA-Clys80, 3 2 3 2 2DL5B Cw*02,04,etc. -S-S- -S-S- 2DS1 2DS3/5 Unknown -S-S- -S-S- 2DS2 2DP1 Unknown -S-S- -S-S- 2DS3 2DL1 Unknown -S-S- -S-S- 2DS4 Unknown -S-S- -S-S- 2DS5 3DP1 2DL4 19 HLA-G -S-S- -S-S- 2DL4 Unknown -S-S- -S-S- 2DL5 HLA-Bw4 -S-S- -S-S- -S-S- 3DL1 HLA-A*03,*11 -S-S- -S-S- -S-S- 3DL2 Unknown -S-S- -S-S- -S-S- 3DL3 Unknown -S-S- -S-S- -S-S- 3DS1 3 3DL/S1 L L S S 2DL5A 2DS3 2DS5 2DS1 NK cell 2DS4 3DL2 U 5 METHODOLOGIES KIR genotyping methods rely on molecular biology techniques, such as PCR (polymerase chain reaction). The currently developed methods include SSP (sequencespecific primers) [Ref. 15, 16], direct sequencing [Ref. 26] or SSOP (sequence-specific oligonucleotide probes) [Ref. 17]. Another direction of methodologies is based on single nucleotide extension and the mass spectrometry. A research group has reported a method that uses a matrix-assisted laser desorption/ionization time-of-flight mass spectrometer (MALDI-TOF) [Ref. 18] to detect single nucleotide extension products of KIR templates. This method holds promise for high-throughput testing, but needs expensive instruments. The real time PCR platform has also been utilized to do KIR genotyping [Ref. 23]. Real time PCR needs more expensive reagents, but could be easily automated. Although commercial kits are supplied with detailed protocols, most of them require reagents and technical support. Laboratories are required to validate the assay prior to clinical use. Alternately, the assays for KIR genotypes can be developed in the laboratory; however, this requires extensive quality control and expertise. In the research area, especially disease association and large-scale gene frequency studies, most laboratories [Ref. 11-14, 19-22] used in-house-developed methods due to budget limits. Commercial kits may be suitable for clinical laboratories when KIR genotyping becomes a clinical practice. U 6 Section : Click here to link to the web based ASHI U Procedure Manual FREQUENTLY ASKED QUESTIONS 7 Question: Why do we need mineral oil in a modern PCR machine with a heated lid? Answer: Even with commonly used machines, such as those listed in the protocol, evaporation still occurs with a 10l volume in a 0.3/0.5 ml PCR tube/well. Mineral oil may be omitted for samples of 20l or more. However, mineral oil is necessary for this protocol. Question: Does any other hot start DNA polymerase work in this protocol? Answer: No. DNA polymerase must be AmpliTaq Gold LD because all the experimental conditions were optimized with this enzyme. One of the hot start enzymes was tried in the conditions established with AmpliTaq Gold, but it did not work. Other laboratories may optimize different hot-start enzymes. Question: Is template DNA concentration flexible? Answer: Yes. We have tested the template range, and the 15ng human genomic DNA per 10l PCR volume is at the relative low end. Usually, when the template DNA is increased up to 3 times, the specific bands will be stronger without increasing the nonspecific bands. U 8 ASHI STANDARDS The ASHI standards sited in this document are from the version noted at the top of the page. Revisions to the ASHI standards may have taken place since the development of this document. Laboratories and individuals should always reference the most current ASHI approved standards. D.2.2.4 Laboratories performing amplification of nucleic acids must: D.2.2.4.1 Use physical and/or biochemical barriers to prevent nucleic acid contamination (carry-over). D.2.2.4.2 Perform pre-amplification procedures in a work area that excludes amplified nucleic acid that has the potential to serve as a template in any other amplification assays performed in the laboratory (e.g., PCR product, plasmids containing HLA genes or relevant STR/VNTR sequences). Restricted traffic flow is recommended. D.2.2.4.3 Use dedicated lab coats, gloves and disposable supplies in the preamplification area. D.4.1 Laboratories performing nucleic acid testing must have written criteria or protocols for: D.4.1.1 Accepting the validity of each molecular assay. D.4.1.2 Preventing DNA contamination using physical and/or biochemical barriers for assays involving amplification of templates. D.4.6 Test systems, equipment, instruments, reagents, materials, supplies, nucleic acid sequence databases, and clinical requirements (systems, applications). D.4.6.1 Test systems must be selected by the laboratory. The testing must be performed following the manufacturer's instructions or as modified and validated by the laboratory and in a manner that provides test results within the laboratory's stated performance specifications for each test system. D.4.6.2 The laboratory must define and follow criteria for those conditions that are essential for proper storage of reagents and specimens, accurate and reliable test system operation, and test result reporting. The criteria must be consistent with the manufacturer's instructions, if provided. These conditions must be monitored and documented and, if applicable, include the following: D.4.6.2.1 Water quality D.4.6.2.2 Temperature D.4.6.2.2.2 Ambient temperatures must be monitored every working day. D.4.6.2.2.3 Refrigerator and freezer temperatures must be monitored continuously and the temperature recorded each day of testing. D.4.6.2.2.4 Refrigerators and freezers must be monitored to ensure maintenance of optimal temperatures for storage of each type of sample or reagent. The laboratory’s storage and maintenance of both critical reagents and relevant transplant candidate specimens must use an audible or centrally monitored temperature alarm system and have an emergency plan for alternative storage. D.4.6.2.3 Humidity D.4.6.2.4 Protection of equipment and instruments from fluctuations and interruptions in electrical current that adversely affect patient test results and test reports. D.4.6.4 Reagents, solutions, culture media, control materials, calibration materials, and other supplies whether commercially purchased or prepared in-house 9 must not be used when they have exceeded their expiration date, have deteriorated, or are of substandard quality. D.4.6.4.1 There must be a documented system in place for identifying which lots and shipments of reagents were used for each assay. D.4.6.4.2 Prior to reporting results obtained with new lots or shipments of reagents, satisfactory performance must be verified and documented. D.4.6.11 Laboratories performing nucleic acid testing must: D.4.6.11.2. Ensure that the laboratory has criteria for accepting each lot and shipment of primers or probes. D.4.6.11.3 Have acceptable limits of signal intensity for positive and negative results. If these are not achieved, acceptance of the results must be justified and documented. D.4.6.11.4 Have an independent review of the data and its interpretation. D.4.6.11.5 Include in each electrophoretic process, controls that verify that the specific targets can be detected. D.4.6.11.6 If the size of a nucleic acid is a critical factor in the analysis of the data: D.4.6.11.6.1 In each gel, include size markers that produce discrete electrophoretic bands spanning and flanking the entire range of expected fragment sizes. D.4.6.11.6.2 The amount of DNA loaded in each lane must be within a range that ensures equivalent migration of DNA in all samples, including size markers. D.4.6.11.7 Ensure that each lot and shipment of primers or probes is monitored to confirm stability and performance of the primers or probes. D.4.6.11.11 Ensure and document acceptable electrophoretic conditions used for each gel electrophoresis. D.4.6.11.13 Laboratories performing amplification-based methods must: D.4.6.11.13.4 Ensure that thermal cycling instruments achieve the appropriate target temperatures during cycling. D.4.6.11.13.5 Ensure that all batches of aliquotted reagents (solutions containing one or multiple components) utilized in the amplification assay are demonstrated to be free of contamination. D.4.6.11.13.6 Ensure that reagents used for primary amplification are not exposed to post- amplification work areas. D.4.6.11.13.8 Verify that the conditions for primer extension (e.g. polymerase type, polymerase concentration, primer concentration, concentration of nucleotide triphosphates) are appropriate for the template (e.g. length of sequence, GC content). D.4.6.11.13.9 Ensure that for each set of primers, conditions that influence the specificity or quantity of amplified product have been demonstrated to be satisfactory for the range of samples routinely tested. D.4.6.11.13.10 Ensure that template quantity and quality are sufficient to provide interpretable data for a locus (or loci) or allele(s). D.4.6.11.13.11 Ensure that the amount of amplification template in each amplification reaction is in an acceptable range. D.4.6.11.13.12 Define and document the specificity and sequence of primer targets. The genetic designation (e.g. locus) of the target amplified by each set of primers must be defined and documented. For each locus analyzed, the laboratory must have documentation that includes the chromosome location, the approximate number of alleles, and the distinguishing characteristics (e.g. sizes, sequences) of the alleles that are amplified. D.4.6.11.15 Laboratories performing SSP methods must: 10 D.4.6.11.15.1 Ensure that an internal control, that produces a product distinguishable from the specific typing product, is included for each primer mixture. D.4.6.11.15.2 Ensure that the amplification conditions are acceptable for the primers used. D.4.6.11.15.3 Include a negative (no nucleic acid) or contamination control in each assay. D.4.6.11.15.4 Ensure that primers used produce adequate amounts of amplification products to be visualized. D.4.9.2 For thermal cycling instruments, the appropriate target temperatures must be achieved. Accuracy of these temperatures must be verified and documented at least every six months. 11 References: 1. Marsh SG, Parham P, Dupont B,et al. Killer-cell immunoglobulin-like receptor (KIR) nomenclature report, 2002. Hum Immunol 2003: 64: 648-54. 2. Norman PJ, Parham P. Complex interactions: the immunogenetics of human leukocyte antigen and killer cell immunoglobulin-like receptors. Semin Hematol. 2005;42:65-75. 3. Middleton D, Williams F, Halfpenny IA. KIR genes. Transpl Immunol. 2005;14:135-42. 4. Vilches C, Parham P. KIR: diverse, rapidly evolving receptors of innate and adaptive immunity. Annu Rev Immunol. 2002;20:217-51. 5. Thananchai H, Gillespie G, Martin MP, et al., Allele-specific and peptidedependent interactions between KIR3DL1 and HLA-A and HLA-B. J Immunol. 2007;178:33-7. 6. Hsu KC, Chida S, Geraghty DE, Dupont B. The killer cell immunoglobulin-like receptor (KIR) genomic region: gene-order, haplotypes and allelic polymorphism. Immunol Rev. 2002; 190:40-52. 7. Ruggeri L, Mancusi A, Capanni M, et al. Donor natural killer cell allorecognition of missing self in haploidentical hematopoietic transplantation for acute myeloid leukemia: challenging its predictive value. Blood. 2007;110:433-40. 8. Sun JY, Dagis A, Gaidulis L, et al. Detrimental effect of natural killer cell alloreactivity in T-replete hematopoietic cell transplantation (HCT) for leukemia patients. Biol Blood Marrow Transplant. 2007;13:197-205. 9. Morishima Y, Yabe T, Matsuo K, et al.; Japan Marrow Donor Program. Effects of HLA allele and killer immunoglobulin-like receptor ligand matching on clinical outcome in leukemia patients undergoing transplantation with T-cell-replete marrow from an unrelated donor. Biol Blood Marrow Transplant. 2007;13:315-28. 10. Cirocco RE, Mathew JM, Burke GW 3rd, Esquenazi V, Miller J. Killer cell immunoglobulin-like receptor polymorphisms in HLA-identical kidney transplant recipients: lack of 2DL2 and 2DS2 may be associated with poor graft function. Tissue Antigens. 2007;69 Suppl 1:123-4. 11. Leung W, Handgretinger R, Iyengar R, et al. Inhibitory KIR-HLA receptor-ligand mismatch in autologous haematopoietic stem cell transplantation for solid tumour and lymphoma. Br J Cancer. 2007;97:539-42. 12. Martin MP, Qi Y, Gao X, et al. Innate partnership of HLA-B and KIR3DL1 subtypes against HIV-1. Nat Genet. 2007 Jun;39(6):733-40. 13. Karlsen TH, Boberg KM, Olsson M, et al. Particular genetic variants of ligands for natural killer cell receptors may contribute to the HLA associated risk of primary sclerosing cholangitis. J Hepatol. 2007;46:899-906. 14. Schellekens J, Rozemuller EH, Petersen EJ, et al. Patients benefit from the addition of KIR repertoire data to the donor selection procedure for unrelated haematopoietic stem cell transplantation. Mol Immunol. 2008;45:981-9. 15. Gomez-Lozano N, Vilches C. Genotyping of human killer-cell immunoglobulinlike receptor genes by polymerase chain reaction with sequence-specific primers: an update. Tissue Antigens 2002: 59: 184-93. 16. Sun JY, Gaidulis L, Miller MM et al. Development of a multiplex PCR-SSP method for Killer-cell immunoglobulin-like receptor genotyping. Tissue Antigens 2004; 64: 462-468. 17. Halfpenny IA, Middleton D, Barnett YA, Williams F. Investigation of killer cell immunoglobulin-like receptor gene diversity: IV. KIR3DL1/S1. Hum Immunol. 2004;65:602-12. U U 12 18. Houtchens KA, Nichols RJ, Ladner MB, et al. High-throughput killer cell immunoglobulin-like receptor genotyping by MALDI-TOF mass spectrometry with discovery of novel alleles. Immunogenetics. 2007;59:525-37. 19. Poggi A, Negrini S, Zocchi MR, et al. Patients with paroxysmal nocturnal hemoglobinuria have a high frequency of peripheral-blood T cells expressing activating isoforms of inhibiting superfamily receptors. Blood. 2005;106:2399408. 20. Norman PJ, Abi-Rached L, Gendzekhadze K, et al. Unusual selection on the KIR3DL1/S1 natural killer cell receptor in Africans. Nat Genet. 2007;39:1092-9. 21. Yawata M, Yawata N, Draghi M, Little AM, Partheniou F, Parham P. Roles for HLA and KIR polymorphisms in natural killer cell repertoire selection and modulation of effector function. J Exp Med. 2006;203:633-45. 22. Hou LH, Steiner NK, Chen M, Belle I, Ng J, Hurley CK. KIR2DL1 allelic diversity: four new alleles characterized in a bone marrow transplant population and three families. Tissue Antigens. 2007;69:250-4. 23. Hong HA, Loubser AS, de Assis Rosa D, et al. Killer-cell immunoglobulin-like receptor genotyping and HLA killer-cell immunoglobulin-like receptor-ligand identification by real-time polymerase chain reaction. Tissue Antigens. 2011 78:185-94. 24. Cooley S, Weisdorf DJ, Guethlein LA, et al. 2010, Donor selection for natural killer cell receptor genes leads to superior survival after unrelated transplantation for acute myelogenous leukemia, Blood. 2010 116: 2411-9. 25. van Bergen J, Thompson A, Haasnoot GW, et al. 2011, KIR-ligand mismatches are associated with reduced long-term graft survival in HLA-compatible kidney transplantation, Am J Transplant 11, 1959-1964. 26. Hou L, Chen M, Steiner N, et al. Killer cell immunoglobulin-like receptors (KIR) typing by DNA sequencing. Methods Mol Biol. 2012 882: 431-68. 27. Kulkarni S, Martin MP, Carrington M. KIR genotyping by multiplex PCR-SSP. Methods Mol Biol. 2010 612: 365-75. 28. Abalos AT, Eggers R, Hogan M, et al. Design and validation of a multiplex specific primer-directed polymerase chain reaction assay for killer-cell immunoglobulin-like receptor genetic profiling. Tissue Antigens. 2011 77:143-8. Recommended Reading: 1. Carrington, M. and Norman, P. The KIR Gene Cluster. Bethesda (MD): National Library of Medicine (US), National Center for Biotechnology Information; 2003. (Available on www.ncbi.nlm.nih.gov/books/bv.fcgi?call=bv.View..ShowTOC&rid= mono_003.TOC&depth=2). 2. IPD-KIR Database: http://www.ebi.ac.uk/ipd/kir/introduction.html 3. Parham P, Norman PJ, Abi-Rached L, Guethlein LA. Human-specific evolution of killer cell immunoglobulin-like receptor recognition of major histocompatibility complex class I molecules. Philos Trans R Soc Lond B Biol Sci. 2012 19 367(1590): 800-11. U TU UT TU UT U 13