* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download INOTROPIC AGENTS - Dr Ted Williams
Silencer (genetics) wikipedia , lookup
Lipid signaling wikipedia , lookup
Protein–protein interaction wikipedia , lookup
Ultrasensitivity wikipedia , lookup
Signal transduction wikipedia , lookup
Two-hybrid screening wikipedia , lookup
G protein–coupled receptor wikipedia , lookup
Metalloprotein wikipedia , lookup
Secreted frizzled-related protein 1 wikipedia , lookup
Biochemical cascade wikipedia , lookup
Proteolysis wikipedia , lookup
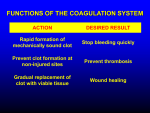
Phar 753, W07 PHARMACY 753, WINTER-2006 MEDICINAL CHEMISTRY/PHARMACOLOGY ANTICOAGULANTS AND FIBRINOLYTIC/THROMBOLYTIC AGENTS Dr. J.F. Stevens -1- Reading assignment: Wilson and Gisvold 11th ed., pp. 663 - 668 1 Phar 753, W07 ANTICOAGULANTS BLOOD COAGULATION PROCESS 1) Platelet Aggregation: Platelets – non-nucleated cells; contain RNA, clotting factors, serotonin, ADP, PAF, Thromboxane etc. – normally do not adhere to smooth intact endothelial cells They do stick to subendothelial tissue exposed by vessel damage Triggers release of compounds stimulating more platelets to adhere Serotonin release promotes local vasoconstriction to close off small, bleeding vessels This aggregate of platelets form a large mass called primary hemostatic plug alone can stop bleeding in areas of minor damage Platelets also stimulate local activation of blood coagulation cofactors leads to fibrin clot formation primary plug also acts as a ‘net’ to catch the procoagulants and serves as a catalytic surface for clot formation 2) Fibrin Clot Formation: Formed by a series of zymogen activations Each step involves a protease converting an inactive precursor protein (zymogen) into another catalytically-active protease. Non-enzyme protein cofactors and Ca2+ are also required at most steps Also need organizing surface provided by platelet plug One example of an enzyme cascade 2 Phar 753, W07 New bonds crosslinking fibrin strands soluble fibrin monomers 3 Phar 753, W07 Partial Pathway of Blood Coagulation and Clot Hydrolysis The blood coagulation process can be activated by one of two pathways. The tissue factor pathway (formerly known as the extrinsic pathway) and the contact activation pathway (known as the intrinsic pathway). Factor X can be activated by either pathway Factor X (inactive) Factor Xa (active) Vitamin k dependent Ca2+, Va Platelet Factor-3 Prothrombin (inactive) Thrombin (active) Vitamin k dependent Fibrinogen Fibrin (soluble) Fibrin Stabilizing Factor (Factor XIIIa) Fibrin Clot (insoluble) Fibrinase-catalyzed formation of an -lysyl--glutamyl fibrin cross link O NH H H N O H2N H N H HN NH3 NH2 O O NH N H O 4 O H H N H HN N H Phar 753, W07 Once the wound has healed, the clot is dissolved – FIBRINOLYSIS Tissue Plasminogen Activator Fibrin Clot (insoluble) Plasminogen Plasmin (inactive) (active) Fibrin Fragments (soluble) ORAL ANTICOAGULANTS AGENTS AFFECTING VITAMIN K-DEPENDENT CLOTTING PROCESS Vitamin K: fat soluble vitamin w/ crucial role in activation of coagulation factors II, VII, IX and X – each of these factors has 9-12 glutamate residues that are converted to -carboxyglutamates – Gla residues are required for these proteins to bind Ca2+ compounds such as warfarin block the fomation of Gla residues the result is a protein factor that can’t bind Ca2+ if unable to bind Ca2+ these factors do not coordinate to platelets and are not brought into proximity with other coagulation factors which is required for the enzyme cascade to function properly BACKGROUND 1924: Cattle that had eaten spoiled sweet clover died of hemorrhagic disease – cause traced to levels of prothrombin OH OH CH 2 1939: Hemorrhagic agent identified as a bishydroxycoumarin: O 1948: More potent synthetic agent developed as a rodenticide: O O O Dicouma rol OH 5 O O CH 3 O Warfarin Phar 753, W07 1951: Person survives suicide attempt from warfarin O.D. 1955: Dwight D. Eisenhower receives warfarin after heart attack Mechanism of Vitamin K-Dependent Coagulation Cofactor Activation Inactive coagualtion factor Active coagualtion factor CH2 CH2 CH2 -O C 2 CO2- CH CO2- -carboxyglutamate (Gla) Glutamate (Glu) Vitamin K-dependent Carboxylase H2O O2, CO2 O OH CH3 CH3 O R R O OH Vitamin K Epoxide Vitamin K (reduced form) NAD+ Vit. K Epoxide Reductase X-(SH)2 Vit. K Epoxide Reductase O CH3 X-S2 R NADH O Vitamin K CH3 R= CH3 CH3 6 CH3 CH3 Phar 753, W07 CHEMISTRY Two structural classes used clinically OH O R 4 1 O R 2 O O 4-Hydroxy Coum arins 1,3-Ind andi ones Both block regeneration of reduced form of vitamin K. Termed indirect acting agents SLOW ONSET: already functional coagulation cofactors are not affected by these compounds depletion of circulating Vitamin K-dependent clotting factors must occur via normal protein catabolism clotting factor t1/2 range from 24-40 hrs full ONSET of action can take 2-7 days. DURATION after discontinuation can last 4-5 days time required for new clotting factors to reach pre-drug levels 7 Phar 753, W07 INDIVIDUAL AGENTS Warfarin (COUMADIN, ATHROMBIN-K) O OH O CH 3 O Warfarin can be adminstered orally, IV or IM WARFARIN SAR – Need H+ at C-4 in order to form salts – S-(-) enatiomer is 5-8x more potent than R-(+) enantiomer – S-isomer is metabolized more rapidly 8 Phar 753, W07 Anisindione (MIRADON) O OCH3 O anisindione Oral Pharmacologically, nearly identical to warfarin Can discolor urine to reddish-orange Non-Vitamin K Dependent Oral Anticoagulants Ximelegatran (EXANTA) Late phase III trials (AstraZeneca) O HO N H H N O N HN NH O OEt Prodrug for melagatran acts as a direct thrombin inhibitor inhibits the free and clot bound enzyme 9 Phar 753, W07 ximelegatran has no effect on human thrombin in vitro oral availability is ca. 20%, measured as melagatran in the plasma. Applying for indications to treat DVT, pulmonary embolism and stroke due to atrial fibrillation in a phase III trial vs warfarin for DVT, ximelegatran was equally effective and did not require routine coagulation monitoring or dose adjustment . IV ANTICOAGULANTS Heparin • Large polysaccharide chain – synthesized as chains of alternating D-glucuronic acid and N-Ac-D-glucosamine units – heavily O- and N-sulfated which gives heparin a high number of anionic groups – very heterogeneous mixture Antithrombin-binding structure of heparin CH2OSO3- (or –H) CH2OSO3- CO2- O O O O OH OH HO CO2- OSO3- NHCOCH3 (or –SO3-) N-acetyl glucosamine 6-O-sulfate OH glucuronic acid NHSO3N-sulfated glucosamine 3,6-O-disulfate 10 O O O O O CH2OSO3- O OSO3 - O OSO3iduronic acid 2-O-sulfate NHSO3N-sulfated glucosamine 6-O-sulfate Phar 753, W07 – commercial heparin is usually isolated from bovine lung or porcine intestinal mucosa o the unmodified polysaccharide is degraded to 5 – 30 kDa fragments during isolation – unstable at low pH and must be given IV – onset of action is immediate Mechanism of Action Heparin alone has no anticoagulant action • It serves as a catalyst to increase the rate at which antithrombin III neutralizes thrombin and factor Xa – heparin binds to antithrombin III – induces a conformational change that promotes binding to protease clotting factors – the clotting factor (protease) then cleaves a specific peptide bond in antithrombin III – a conformational change occurs that results in a very stable clotting factor/antithrombin III complex – heparin is released from complex and can go an bind to another thrombin or factor Xa molecule 11 Phar 753, W07 LOW MOLECULAR WEIGHT HEPARIN • Lower proportion of the critical pentasaccharide sequence required for antithrombin III bindings – increases action of antithrombin III on factor Xa but has less effect on thrombin o only 25-50% of LMWH molecules bind and inactivate thrombin referred to as the Factor Xa:IIa ratio – average MW is 4000 – 5000 – more predictable and higher bioavailability than heparin and longer t1/2 o HMWH is only 30% bioavailable, but up to 90% of a dose of LMWH is absorbed LMWH Marketed in U.S. Name Trade name Manufacturer Enoxaparin Lovenox Dalteparin Fragmin Tinzaparin Innohep Rhone-Poulenc Rorer Pharmacia and Upjohn Novo Ardeparin Normiflo Wyeth-Ayerst Fractionation method LMWH Used Worldwide Nadroparin Sanofi Parnaparin Opocrin Reviparin Knoll Benzylation and alkaline depolymerization Nitrous acid depolymerization Enzymatic degradation Peroxidative depolymerization Nitrous acid depolymerization Cupric acid and hydrogen peroxide degradation Nitrous acid depolymerization 12 Halflife (h) Factor Xa:IIa ratio (daltons) Average molecular 4.5 2.7:1 weight 4,500 2-4 2.0:1 4,000-6,000 1.3 2:1 4,900 1.2-3.3 2.0:1 5,600-6,500 3.5 2-4.1 4,500 4 3:1 4,500-5,000 NA 3-5:1 4,300 Phar 753, W07 Fondaparinux sodium (ARIXTRA®) • Synthetic sulfated pentasaccharide, MW = 1728 – • contains only the critical region of heparin required to bind to antithrombin III Fondaparinux is more selective for the inhibition of factor Xa than heparins and LMWH – Selectivity increases the neutralization of factor Xa by antithrombin More effective than unfractionated heparins and LMWH in preventing venous thromboembolism after orthopedic surgery for hip fracture, hip replacement, and knee replacement • well-absorbed when given by subcutaneous injection – very predictable effect and patients do not require monitoring as frequently as patients receiving other agents, Heparin Side Effects Most serious is Heparin Induced Thrombocytopenia (HIT): typically occurs 7-14 days after initiation of therapy. Results in heparin-induced platelet aggregation and the production of antibiodies directed towards platelets with heparin bound to surface platelet factor 4 (PF4). Requires terminating heparin and adminstration of antiplatelet agents and oral anticoagulants or defibrination agents 13 Phar 753, W07 Ancrod –glycosylated serine protease (234 amino acid, 35 kDa) from snake venom high specificity for fibrinogen. Rapidly removes normal fibrinogen from the blood stream w/o affecting other clotting factors. Lepirudin (REFLUDAN) – recombinant hirudin produced in yeast cells. Hirudin is a direct thrombin inhibitor, does not require antithrombin III. Lepirudin is Leu1-Thr2-63-desulfohirudin. The polypeptide is composed of 65 amino acids and has a molecular weight of 7.0 kDa. Natural hirudin is produced in trace amounts as a family of highly homologous polypeptides by the leech Hirudo medicinalis. For patients who cannot tolerate heparin. Argatroban: a new reversible direct thrombin inhibitor for treatment of HIT and for preventing HIT in patients receiving heparin. NH H2N O N H CO2H N NH O S CH3 O CH3 Hemorrhaging from heparin use is managed with protamine sulfate – highly cationic proteins (mostly arginine residues) from salmon sperm. Fairly specific for binding the anionic heparin and rendering it inactive. 14 Phar 753, W07 ANTIPLATELET AGENTS Coagulation process is slowed if platelets are prevented from aggregating Several classes of agents that affect platelet aggregation • Aspirin and other agents that block thromboxane A2 synthesis e.g., sulfinpyrazone (ANTURANE) O O aspirin • O O N N OH S O O sulfinpyrazone Inhibit cAMP phoshodiesterase > increasing platelet cAMP > decreasing AMP and ADP. e.g., dipyridamole (PERSANTINE). Use: prevent thrombus formation on prosthetic heart valves. OH N N N HO N N OH N N N OH ADP receptor antagonists. Clopidrogel/Clopidogrel (Plavix) causes irreversible inhibition of platelet function. It is a prodrug that is activated by cytochrome P450 in the liver. The active metabolite binds covalently to ADP receptor subtype P2Y2 on platelets, causing inhibition of ADP-mediated activation of GP IIb/IIIa receptors on platelet surface (no binding with fibrinogen). Use: atherosclerotic vascular disease. 15 Cl O O N S clopidrogel Phar 753, W07 GP IIb/IIIa Receptor Antagonists • Platelet aggregation is a key step in thrombus formation – • can lead to myocardial infarction and acute coronary syndrome, including unstable angina. Glycoprotein IIb/IIIa receptors are found on platelets and, when activated, bind fibrinogen which leads to the final step in platelet aggregation. Several inhibitors of GP IIb/IIIa activation have proven useful as antithrombotics and to treat unstable angina Abciximab (REOPRO®) first agent of this class to demonstrate clinical effectiveness. Used during percutaneous coronary intervention chimeric human-murine Fab fragment of a monoclonal antibody against the GP IIb/IIIa receptor – lacks high receptor-blocking specificity – can be antigenic – very expensive Need for agents with greater specificity, reduced tendency for allergic reaction and shorter half-life led to search for peptdomimetics. Numerous snake venoms known to inhibit platelet aggregation. Venom peptides and proteins provided the leads for drug development. Tirofiban (AGGRASTAT®). Used in patients undergoing PTCA (percutaneous transluminal coronary angioplasty) CO2H Developed from an anticlotting protein isolated from venom of saw-scaled viper O H HN Injectable, used to treat unstable angina Can cause bleeding 16 (CH2)4 O N H S O (CH2)3 CH3 Phar 753, W07 Eptifibatide (INTEGRILIN®) Based on barbourin – a peptide from the southeastern pygmy rattlesnake showed high specificity for GP IIb/IIIa Injectable, used to treat unstable angina and during percutaneous transluminal angioplasty Can cause bleeding Prostacyclin (PGI2) the natural antiplatelet aggregation agent stable, orally active analogs COOH O O HO COOH HO OH PGI2 = prostacyclin = Epoprostenol administered by continuous infusion 17 OH Beraprost (PGI2 analog, oral) approved in Japan Phar 753, W07 FIBRINOLYTICS AND THROMBOLYTIC AGENTS used to dissolve or break up unwanted thrombi Tissue Plasminogen Activator Fibrin Clot (insoluble) Plasminogen Plasmin (inactive) (active) Fibrin Fragments (soluble) Normally, Tissue Plasminogen Activator (t-PA) is released from endothelial cells in response to various signals t-PA binds to the fibrin clot and cleaves and activates plasminogen to plasmin t-PA cleaves fibrin-bound plasminogen 100x faster than circulating plasminogen ** shows the importance of proximity and orientation/alignment Streptokinase (KABIKINASE, Streptase): Acute pulmonary embolism, DVT, acute MI non-enzyme protein isolated from a streptococci bacterium Indirect plasminogen activator Forms a 1:1 complex with plasminogen and induces a conformational change new conformation gives the complex plasmin-like catalytic activity can cleave other plasminogen molecules to plasmin PROBLEMS: SK is a foreign protein and antibodies are produced. requires a loading dose to overcome antibodies present in system from previous streptococcal infections can not reuse SK for several months t1/2 after Ab depletion is ~80 min 18 Phar 753, W07 Major side effect is bleeding allergic response other disadvantage is poor selectivity for clot-bound vs. circulating (free) plasminogen Ideally want to localize plasminogen activation to the site of the clot Anistreplase = Anisoylated Plasminogen Streptokinase Activator Complex (APSAC) (EMINASE®), acute MI complex of streptokinase and plasminogen O Active site serine is acylated with a p-anisoyl group, which gets O Ser O hydrolyzed in vivo essentially SK prodrug has a longer t1/2 slightly higher fibrin specificity Urokinase (ABBOKINASE): Urinary Plasminogen Activator. Pulmonary embolism and DVT Originally isolated form urine, now produced by kidney cell culture Urokinase is a protease cleaves a peptide bond in plasminogen to form plasmin Advantage over streptokinase is that it is non-antigenic t1/2 = 15 min very expensive Recombinant TPA (rTPA, alteplase) (ACTIVASE) Acute MI Human gene for TPA is inserted into CHO cells and over expressed first recombinant protein approved for clinical use endogenous factor – highest fibrin specificity and non-antigenic t1/2 = 3 min some controversy regarding efficacy two early trials (40K and 22K patients) found no difference between the two drugs Genentech claimed protocol was flawed - not given soon enough 19 Phar 753, W07 Subsequent trial w/ 41K patients showed a statistically significant 1% difference in favor of rTPA study also included aspirin Tenecteplase: variant of alteplase (six point mutations) > significant increase in plasma half life (20 min). Administered by IV bolus injection. Reteplase: deletion variant of t-PA, lacks fibrin-binding sites and oligosaccharide side chains (expressed in prokaryotic E. coli.). Eliminated slower than alteplase. Given in two bolus injections 30 minutes apart. INVESTIGATIONAL THROMBOLYTICS Cost of rTPA driving search for source of low cost PA with low immunogenicity and high fibrin specificity Staphylokinase from S.aureus indirect PA like streptokinase more clot specific than SK less induction of neutralizing Abs Bat-PA recombinant form of PA isolated from vampire bat (Desmodus rotundus salivary plasminogen activator, DSPA or desmoteplase) low immunogenicity sequence is 80% homologous w/ human t-PA higher fibrin specificity than human t-PA (Developed by Professor Schleuning at PAION/Schering Berlin) 20