* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Cardiac Failure Protocol
Remote ischemic conditioning wikipedia , lookup
Heart failure wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Cardiac surgery wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Electrocardiography wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Coronary artery disease wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
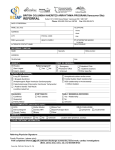
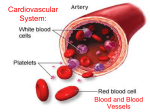
Cardiac Failure ProtocolAim To ensure that all patients with cardiac failure are appropriately investigated, treated and followed up. Objectives To confirm the diagnosis of heart failure by electrocardiography where possible. To consider all possible treatment options to improve the quality of life. To promote the use of angiotensin-converting enzyme inhibitors Identification of target population Cardiac failure is a clinical syndrome comprising breathlessness, fatigue and fluid retention due to cardiac dysfunction. All patients with suspected cardiac failure should undergo clinical examination and a 12 lead ECG. Symptoms such as breathlessness, fatigue and ankle swelling & clinical such as tachycardia, oedema and lung crepitations are non-specific. To increase the likelihood of diagnosis look for the following: Pointers in history: Ischaemic heart disease, especially previous myocardial infarction, longstanding hypertension, excessive alcohol consumption, valve disease, anaemia, thyroid disease. Pointers in examination: elevated JVP, third hear sound, displaced apex beat, murmur. Significant cardiac failure is unlikely if the ECG is normal. Disease register Patients with a firm clinical diagnosis of cardiac failure are Read-coded by the GP and entered on the computerised disease register Investigation of patients with suspected heart failure ECG Echocardiogram Full blood count, are & electrolytes and thyroid function blood tests. Frequency & content of review Once investigated, patients are reviewed by the GP to initiate appropriate drug & nondrug therapy. Frequency of review will be dictated by clinical condition & response to treatment. Management of patients with confirmed systolic dysfunction If possible, stop NSAID, calcium blockers such as nifedipine, diltazium, or if severe heart failure, stop beta blocker. Non-pharmological measures: avoid salt in diet, excess alcohol, encourage exercise, weight reduction where appropriate and smoking cessation. Start ACE inhibitor: Stop potassium supplements or potassium sparing diuretics. Advise re: possible symptomatic hypotension – lie for 4 hours after starting low dose ACE inhibitor. Increase does after 1 week and recheck urea and electrolytes. Titrate dose over 1 month, check for dizziness, cough and abnormal U&Es. Refer if urea >12, creatinine>200, Na <130, systolic BP <100mmHg or if on >80mg Furosemide, or if known renal artery stenosis. If Atrial Fibrillation present, consider referral as warfarin and digoxin may be helpful. If angina present, consider referral as CABG may be indicated If still dyspnoea or fluid retention present, increase dose of loop diuretic, add digoxin or consider referral If ACE inhibitor contraindicated or not tolerated, angiotensin 11 receptor antagonists may be used as an alternative.