* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download 5. Thrombocytopenia
Complement system wikipedia , lookup
Innate immune system wikipedia , lookup
Adoptive cell transfer wikipedia , lookup
Molecular mimicry wikipedia , lookup
Hygiene hypothesis wikipedia , lookup
Anti-nuclear antibody wikipedia , lookup
Polyclonal B cell response wikipedia , lookup
Guillain–Barré syndrome wikipedia , lookup
Psychoneuroimmunology wikipedia , lookup
Management of multiple sclerosis wikipedia , lookup
Autoimmunity wikipedia , lookup
Pathophysiology of multiple sclerosis wikipedia , lookup
Monoclonal antibody wikipedia , lookup
Cancer immunotherapy wikipedia , lookup
Multiple sclerosis research wikipedia , lookup
Autoimmune encephalitis wikipedia , lookup
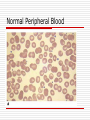
Thrombocytopenia Rahul Gladwin, MS3 University of Health Sciences-Antigua School of Medicine Thrombocytopenia Causes of Thrombocytopenia TTP/ITP Drug-induced Thrombocytopenia HIV-associated Thrombocytopenia Disseminated intravascular coagulation Pancytopenia Complications Management Case study Definition Thrombocytopenia is defined as a decrease in the number of platelets. Normal platelet counts range from 150,000-300,000/µL. Anything below 100,000/µL constitutes thrombocytopenia. Why does platelet count matter? Platelets help form blood clots. Unexplained epistaxis, petechiae, gingivorrhagia, and vaginal bleeding imply decreased platelet counts. Platelet count below 20,000/µL causes spontaneous internal bleeding. Platelet count between 20,00050,000/µL aggravates post-traumatic bleeding. Causes of thrombocytopenia Causes of thrombocytopenia can be divided into four main classes: 1. 2. 3. 4. Decreased production of platelets Decreased platelet survival Sequestration Dilutional Decreased production of platelets Bone marrow diseases e.g., aplastic anemia, Fanconi’s anemia, leukemia, disseminated cancer. Medications: alkylating agents, benzene, chloramphenicol, streptomycin, chlorpromazine, antimetabolites. Insectides: DDT, parathion Viruses: hepatitis, EBV virus, CMV. Decreased production of platelets Alcohol, thiazides, cytotoxic drugs, measles, HIV. Vitamin B12 and folic acid deficiency. Megaloblastic anemia, myelodysplastic syndromes. Decreased platelet survival Autoimmune: idiopathic thrombocytopenic purpura, systemic lupus erythematosus, hemolytic-uremic syndrome, anti-platelet antibodies. Isoimmune: post-transfusion and neonatal. Drug-associated: quinidine, heparin, sulfadrugs. Infections: infectious mononucleosis, HIV, CMV. Sequestration The spleen sequesters 30-40% of the body’s total platelets. Splenomegaly secondary to hypersplenism. Treatment is splenectomy. Bone marrow biopsy shows increased megakaryocytes. Question: What test do you order in order to differentiate between thrombocytopenia caused by decreased platelet production (ie., by cancer, drugs, autoimmune, chemotherapy, etc.) vs thrombocytopenia caused by increased sequestration? Answer: Bone marrow biopsy shows increased megakaryocytes in thrombocytopenia caused by increased sequestration. Presence of megakaryocytes implies that the bone-marrow is working over time in order to compensate for increased platelet loss. Dilutional Massive transfusions can produce thrombocytopenia because stored blood contains very little platelets. Packed blood doesn’t contain many thrombocytes. Immune Thrombocytopenic Purpura Causes autoimmune destruction of platelets secondary to HIV, SLE, viruses, and drugs. IgG antibodies target platelet glycoprotein complexes IIb-IIIa and Ib-IX. Sensitized platelets are removed by the spleen. Increased bleeding time; normal PT & PTT. Petechiae and Purpura due to ITP Acute Immune Thrombocytopenic Purpura Similar to ITP but occurs only in childhood. Abrupt thrombocytopenia due to viral cause. Resolves spontaneously within 6 months. Drug-induced thrombocytopenia Drugs involved are heparin, quinine, quinidine, sulfonamide antibiotics. Type I HIT: less severe, occurs rapidly after therapy. Type II HIT: more severe, occurs 5-16 days after therapy. HIT is caused by an immune reaction against a complex of heparin and platelet factor 4, which produces immune complexes. Heparin-induced thrombocytopenia Heparin-induced thrombocytopenia Heparin-induced thrombocytopenia HIT is not usually severe, with low counts rarely <20,000/μL. Not associated with bleeding Increases the risk of thrombosis. Caused by low-molecular weight heparin (LMWH) More commonly caused by unfractionated heparin (UFH). HIT (antiheparin/PF4) antibodies can be detected using enzyme-linked immunoassay (ELISA) with PF4/polyanion complex as the antigen. A platelet activation assay confirmatory test can also be used. Heparin given with warfarin has decreased chance of causing HIT compared to giving heparin alone. Autoimmune thrombocytopenia vs HIT Question: What test would you order in order to confirm HIT? Answer (two tests): Test for PF4 antibodies (PF4 ELISA). Serotonin release assay. Chloramphenicol-induced thrombocytopenia Chloramphenicol affects the bonemarrow causing anemia, leukopenia, thrombocytopenia. Chloramphenicol causes an idiosyncratic response manifested by aplastic anemia in patients receiving prolonged therapy. HIV-associated thrombocytopenia Decreased platelet production and increased platelet destruction. Three causes: Existence of CD4 receptor on megakaryocytes makes them prone to destruction. HIV causes hyperplasia and dysregulation of B cells, producing IgG antibodies which target platelet glycoprotein complexes IIb-IIIa and Ib-IX resulting in thrombocytopenia. Autoantibodies may cross-react with HIV-associated gp120 acting as opsonins, thus promoting phagocytosis of platelets in the spleen. TTP & HUS TTP is caused by bone marrow transplantation, cancer, chemotherapy and manifested as microangiopathic hemolytic anemia, thrombocytopenia, renal failure, neurologic findings, and fever. HUS caused by infection and is manifested as acute renal failure, microangiopathic hemolytic anemia, and thrombocytopenia. Deficiency of ADAMTS 13 produces a defective protease causing very high molecular weight multimers of vWF to accumulate in plasma promoting platelet microaggregate formation leading to thrombocytopenia. Thrombotic Thrombocytopenic Purpura Disseminated Intravascular Coagulation DIC is an acute, subacute, or chronic thrombohemorrhagic disorder occurring secondary to a variety of conditions. Begins with extrinsic (release of tissue factor) and intrinsic (factor XII activation) clotting cascade activation. Both pathways cause platelet consumption and thrombi formation leading to thrombocytopenia. Arterial thrombosis secondary to sepsis-induced DIC Endothelial injury – induced thrombocytopenia Endothelial injury can activate tissue factor, which activates TNF, which upregulates leukocyte adhesion, which damages endothelial cells and releasing free radicals and proteases causing activation of both the extrinsic and intrinsic pathways leading to thrombocytopenia. Pancytopenia Caused by bone marrow failure, radiation, auto-immune diseases, drugs, infections. Pancytopenia is a combination of anemia, leukopenia, and thrombocytopenia. Thrombocytopenia Management Rule out pseudothrombocytopenia (in vitro artifactual IgG or IgM-induced clumping of platelets). H&P (splenomegaly, liver disease). CBC. Peripheral blood smear. Medication list. Bone marrow biopsy. Drug-induced thrombocytopenia Normal Peripheral Blood Pseudothrombocytopenia Macrothrombocytopenia: Large platelets Schistocytes in microangiopathic hemolytic anemia (HUS/TTP). Complications of thrombocytopenia Intracranial hemorrhage. GI bleeding. Epistaxis. Menorrhagia. Gingivorrhagia. When do you treat? You treat thrombocytopenia when the platelet count is less than 50,000/µL. You do not treat when the platelet count is over 50,000/µL. You do a bone-marrow biopsy in patients presenting with isolated thrombocytopenia who are older than 60 years in order to rule out myelodysplasia. Related medications - Prednisone Methylprednisolone sodium succinate (SOLU-MEDROL) Used to decrease bleeding tendency. Patients with refractory ITP may respond. Dosed as 1-1.5kg/mg. Related medications - Argatroban Anticoagulant or platelet aggregation inhibitor. Prevents the activation of coagulation factors V, VIII, and XIII; protein C. Used to replace heparin in patients with heparin-induced thrombocytopenia. Related medications - Lepirudin The same as hirudin except that it contains leucine instead of isoleucine at the N-terminal end of the molecule and an absent sulfate group on the tyrosine at position 63. It binds thrombin and prevents thrombus or clot formation. Alternative to heparin in HIT. Can also cause thrombocytopenia. Related medications - Bivalirudin Used for treatment of HIT in patients who have undergone percutaneous coronary intervention (PCI). Inhibits thrombin Very short half-life. Related medications - Oprelvekin Recombinant IL-11 Produced by E. coli. Increases platelet levels which were reduced due to chemotherapy. IL-11 is a growth factor that stimulates proliferation of hematopoietic stem cells and megakaryocyte progenitor cells resulting in increased platelet production. Related medications - Eltrombopag Used to treat ITP. MOA is unknown. Oral thrombopoeitin (TPO) receptor agonist. May reduce antibodies to platelets. Related medications - IgG Used to treat ITP. Removes offending immune complexes composed of viral particles. Low-dose anti-D antibodies (Rhogam) can also be used to treat ITP. Other thrombocytopenia treatments Splenectomy: in severe cases and if there is recurrent bleeding after steroids. Plasmapheresis (TTP). Dialysis (RF). Platelet transfusion (active bleeding or severe cases). Lithium carbonate or folate. Thrombocytopenia case study A 21-year-old man with no significant PMH presents with complaints of hematuria and mucosal bleeding while brushing his teeth. The patient complains of intermittent "ringing in the ears." He denies any drug or alcohol use. He has no family history of bleeding disorders. Petechiae are noted in the oral cavity, as is dried blood in the nostrils. Hematocrit 32% | WBC 8,000/mm3 with 60% neutrophils. Platelet count 13,000; PT 13 seconds; PTT 28 seconds; LDH 1,200 U/L. Elevated indirect bilirubin. Coombs' test is positive; abdominal examination is normal. Peripheral smear shows spherocytes. A) Alport's syndrome B) Bernard-Soulier syndrome C) Felty's syndrome D) Thrombotic thrombocytopenic purpura E) Evans' syndrome F) Idiopathic thrombocytopenic purpura (ITP) Answer Answer: E Evans' syndrome is the association of autoimmune destruction of RBC, WBCs, and platelets. TX: steroids and/or splenectomy. References Robbins Pathology Harrison’s IM First Aid for USMLE The Pharmacological Basis of Therapeutics Dorland's Medical Dictionary www.usmleforum.com