* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download 2-Pathology of non-atherosclerotic vascular diseases_1
Acute pancreatitis wikipedia , lookup
Hygiene hypothesis wikipedia , lookup
Anti-nuclear antibody wikipedia , lookup
Inflammation wikipedia , lookup
Psychoneuroimmunology wikipedia , lookup
Rheumatic fever wikipedia , lookup
Cancer immunotherapy wikipedia , lookup
Autoimmunity wikipedia , lookup
Rheumatoid arthritis wikipedia , lookup
Monoclonal antibody wikipedia , lookup
Polyclonal B cell response wikipedia , lookup
Ankylosing spondylitis wikipedia , lookup
Multiple sclerosis signs and symptoms wikipedia , lookup
Autoimmune encephalitis wikipedia , lookup
Neuromyelitis optica wikipedia , lookup
Sjögren syndrome wikipedia , lookup
Behçet's disease wikipedia , lookup
Atherosclerosis wikipedia , lookup
Immunosuppressive drug wikipedia , lookup
Multiple sclerosis research wikipedia , lookup
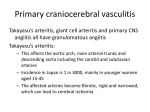
Pathology of Non-Atherosclerotic Vascular Diseases II Prof. Dr. Gamze MOCAN KUZEY NEU Department of Pathology Vascular Lesions Atherosclerosis Arteriolosclerosis Varicose veins Trombophlebitis Lymphedema Aneurysms Dissection Vasculitis Vasculitis Vasculitis Inflammation of the walls of vessels The two most common mechanisms of vasculitis are the direct invasion of vascular walls by infectious pathogens and immune-mediated mechanisms Physical and chemical injury, such as irradiation, mechanical trauma, and toxins can also cause vascular damage. Pathogenesis of Noninfectious Vasculitis immune complex deposition, antineutrophil cytoplasmic antibodies, (ANCAs), anti-endothelial cell antibodies. Immune Complex Deposition DNA-anti-DNA complexes are present in the vascular lesions of systemic lupus erythematosusassociated vasculitis IgG, IgM, and complement in cryoglobulinemic vasculitis Antineutrophil cytoplasmic Antibodies, (ANCAs) ANCAs are a heterogeneous group of autoantibodies directed against enzymes mainly found within the azurophil or primary granules in neutrophils, in the lysosomes of monocytes, and in endothelial cells (EC) Antineutrophil cytoplasmic antibodies (ANCAs) Two main patterns are recognized by immunofluorescent staining: one shows cytoplasmic localization of the staining (c-ANCA), and the most common target antigen is proteinase-3 (PR3), a neutrophil granule constituent. The second shows perinuclear staining (p-ANCA) and is usually specific for myeloperoxidase (MPO). Antineutrophil cytoplasmic antibodies (ANCAs) c-ANCA is typically found in Wegener granulomatosis p-ANCA is found in most cases of microscopic polyangiitis and Churg-Strauss syndrome ANCAs The disorders characterized by circulating ANCAs are called the ANCA-associated vasculitides. ANCAs serve as useful quantitative diagnostic markers and their levels may reflect the degree of inflammatory activity Anti-endothelial Cell Antibodies Antibodies to ECs, perhaps induced by defects in immune regulation, may predispose to certain vasculitides, such as those associated with SLE and Kawasaki disease Classification of Vasculitis The systemic vasculitides are classified on the basis of the size and anatomic site of the involved blood vessels histologic characteristics of the lesion, and clinical manifestations. There is considerable clinical and pathologic overlap among them Giant cell (temporal) arteritis Rare in persons younger than age 50, extraordinary trophism for a single arterial site remains unexplained high incidence in populations of Nordic origins. The diagnosis depends on biopsy and histologic confirmation, Because of the segmental nature of the involvement, adequate biopsy requires at least a 2to 3-cm length of artery, and negative or atypical findings on biopsy do not rule out the condition. Giant cell (temporal) arteritis the most common form of systemic vasculitis in adults, acute and chronic, often granulomatous, inflammation of arteries of large to small size affects principally the arteries in the headespecially the temporal arteries, but also the vertebral and ophthalmic arteries and the aorta, where it may cause thoracic aortic aneurysm. Giant cell (temporal) arteritis Pathogenesis The morphologic alterations suggest an immunologic reaction against a component of the arterial wall, such as elastin The granulomatous nature of the inflammation, association with certain human leukocyte antigens (HLA-DR), and the response to corticosteroid therapy, are consistent with T cellmediated and antigen-driven injury TAKAYASU ARTERITIS granulomatous vasculitis of medium and larger arteries, described in 1908 by Takayasu, characterized by ocular disturbances and marked weakening of the pulses in the upper extremities (pulseless disease). The pathologic findings are vasculitis and subsequent fibrous thickening of the aorta, particularly the aortic arch and its branches, with narrowing or virtual obliteration of the origins or more distal portions TAKAYASU ARTERITIS- MORPHOLOGY Classically involves the aortic arch, but in one third of cases it also affects the remainder of the aorta and its branches, in half the cases, it affects the pulmonary arteries. When the aortic arch is involved, the orifices of the major arteries to the upper portion of the body may be markedly narrowed or even obliterated by intimal thickening The coronary and renal arteries may be affected TAKAYASU ARTERITIS- MORPHOLOGY The changes range from an adventitial mononuclear infiltrate with perivascular cuffing of the vasa vasorum to intense mononuclear inflammation in the media. Granulomatous inflammation in some cases may be indistinguishable from those in giant cell (temporal) arteritis. Thus, distinctions among active giant cell lesions of the aorta are based largely on the age of the patient, and most giant cell lesions of the aorta in young patients are designated Takayasu arteritis. POLYARTERITIS NODOSA (PAN) PAN is a systemic vasculitis of small or medium-sized muscular arteries (but not arterioles, capillaries, or venules), typically involving renal and visceral vessels but sparing the pulmonary circulation. Clinical manifestations result from ischemia and infarction of affected tissues and organs. POLYARTERITIS NODOSA (PAN)MORPHOLOGY Classic PAN occurs as segmental transmural necrotizing inflammation of arteries of medium to small size, in any organ with the possible exception of the lung, and most frequently kidneys, heart, liver, and gastrointestinal tract Individual lesions may involve only a portion of the vessel circumference and have a predilection for branching points and bifurcations POLYARTERITIS NODOSA (PAN)MORPHOLOGY Particularly characteristic of PAN is that all stages of activity may coexist in different vessels or even within the same vessel. About 30% of patients with PAN have hepatitis B antigen in their serum. There is no association with ANCA. KAWASAKI DISEASE (MUCOCUTANEOUS LYMPH NODE SYNDROME) arteritis that often involves the coronary arteries, usually in young children and infants (80% of cases are <4 years old), and is the leading cause of acquired heart disease in children in North America and Japan. It is associated with the Mucocutaneous Lymph Node Syndrome Mucocutaneous Lymph Node Syndrome Epidemic in Japan, also been reported in Hawaii & increasingly in the continental United States. 20% of patients develop cardiovascular sequelae, ranging in severity from asymptomatic vasculitis of the coronary arteries, coronary artery ectasia, or aneurysm formation to giant coronary artery aneurysms (7 to 8 mm) with rupture or thrombosis, myocardial infarction, or sudden death. Mucocutaneous Lymph Node Syndrome an acute but usually self-limited illness manifested by fever, conjunctival and oral erythema and erosion, edema of the hands and feet, erythema of the palms and soles, a skin rash often with desquamation, enlargement of cervical lymph nodes KAWASAKI DISEASE MORPHOLOGY The vasculitis is PAN-like, with necrosis and pronounced inflammation affecting the entire thickness of the vessel wall, but fibrinoid necrosis is usually less prominent KAWASAKI DISEASE Pathogenesis vasculitis results from an immune reaction characterized by T-cell and macrophage activation to an unknown antigen, secretion of cytokines, polyclonal B-cell hyperactivity, and the formation of autoantibodies to endothelial cells and smooth muscle cells, leading to acute vasculitis MICROSCOPIC POLYANGIITIS (MICROSCOPIC POLYARTERITIS, HYPERSENSITIVITY ANGIITIS, LEUKOCYTOCLASTIC VASCULITIS) This type of necrotizing vasculitis generally affects arterioles, capillaries, and venulesvessels smaller than those involved in PAN. In contrast to PAN, all lesions tend to be of the same age. MICROSCOPIC POLYANGIITIS It typically presents as: "palpable purpura" involving the skin, involvement of the mucous membranes, lungs, brain, heart, gastrointestinal tract, kidneys, muscle. Skin biopsy is often diagnostic MICROSCOPIC POLYANGIITIS In contrast to PAN, necrotizing glomerulonephritis (90% of patients) and pulmonary capillaritis are particularly common The major clinical features are hemoptysis, arthralgia, abdominal pain, hematuria, proteinuria, hemorrhage, and muscle pain or weakness. MICROSCOPIC POLYANGIITIS In many cases, an immunologic reaction to an antigen such as drugs (e.g., penicillin), microorganisms (e.g., streptococci), heterologous proteins, tumor antigens are the precipitating cause In 70% of patients, p-ANCAs are present. MICROSCOPIC POLYANGIITIS-MORPHOLOGY histologically similar to PAN In contrast to PAN, muscular and large arteries are usually spared;macroscopic infarcts similar to those seen in PAN are uncommon. It has the same spectrum of manifestations as Wegener granulomatosis, granulomatous inflammation is absent. MICROSCOPIC POLYANGIITIS-MORPHOLOGY Histologically, segmental fibrinoid necrosis of the media may be present, but in some lesions the change is limited to infiltration with neutrophils, which become fragmented as they follow the vessel wall (leukocytoclasia). The term leukocytoclastic angiitis (LCA) is given to such lesions, most commonly found in postcapillary venules Disseminated vascular lesions of hypersensitivity angiitis may also appear in; Henoch-Schönlein purpura, essential mixed cryoglobulinemia, vasculitis associated with some of the connective tissue disorders, vasculitis associated with malignancy. Churg-Strauss syndrome In allergic granulomatosis and angiitis (Churg-Strauss syndrome), necrotizing vasculitis accompanied by granulomas with eosinophilic necrosis. p-ANCAs are present in approximately 50% of patients. Churg-Strauss syndrome There is a strong association with allergic rhinitis, bronchial asthma, and eosinophilia Vessels in the lung, heart, spleen, peripheral nerves, and skin are frequently involved by intravascular and extravascular granulomas, infiltration of vessels and perivascular tissues by eosinophils is striking. WEGENER GRANULOMATOSIS 1. 2. 3. Wegener granulomatosis is a characterized by the triad of necrotizing vasculitis acute necrotizing granulomas of the upper respiratory tract (ear, nose, sinuses, throat), the lower respiratory tract (lung), or both; necrotizing or granulomatous vasculitis affecting small to medium-sized vessels (e.g., capillaries, venules, arterioles, and arteries), most prominent in the lungs and upper airways but affecting other sites as well; renal disease in the form of focal necrotizing, often crescentic, glomerulitis. WEGENER GRANULOMATOSIS In some patients the disease is restricted to the respiratory tract "limited" Wegener granulomatosis Widespread Wegener granulomatosis affects the eye, skin, and (rarely) other organs, notably the heart, the clinical syndromes may be very similar to PAN with the addition of respiratory involvement. WEGENER GRANULOMATOSIS Upper respiratory tract lesions range from inflammatory sinusitis resulting from mucosal granulomas to ulcerative lesions of the nose, palate, or pharynx, rimmed by necrotizing granulomas and accompanying vasculitis.