* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Anti-fungal drug
Survey
Document related concepts
Transcript
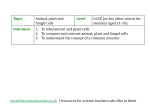
ANTI FUNGAL AGENT FUNGI • Very large and diverse group of microorganisms • Classified into yeast and molds • Yeast is single cell organism, useful for baking and alcohol beverages • Molds are multicellular, characterized by long, branching filaments called hyphae FUNGI • Fungi are eukaryotic, heterotrophic (not self sustaining) organisms that live as saprobes or parasites. • They are complex organisms in comparison to bacteria. Thus antibacterial agents are not effective against fungi. • Fungal infections are also called as mycoses • They have nucleus and well defined nuclear membrane, and chromosomes. • They have rigid cell wall composed of chitin ( N – acetylglucosamine ) • Fungal cell membrane contains ergosterol , human cell mebmrane is composed of cholesterol. FUNGAL INFECTIONS • Yeast infections • Candida species • Cryptococcus neoformats • Moulds (filamentous fungi) • • • • Aspergillus sp. Dermatophytes Trichophyton Microsporum MYCOSIS • A fungal infection of animals, including humans. • Common and a variety of environmental and physiological conditions can contribute to the development. • Initiation of persistent infections:• Inhalation of fungal spores • localized colonization of the skin • Therefore, mycoses often start in the lungs or on the skin. Epidemology:• Skin Fungal infections- the 4th most common disease in 2010 • Affecting 984 million people. CAUSES • Individuals being treated with antibiotics are at higher risk of fungal infections. • Individuals with weakened immune systems are also at risk of developing fungal infections. • This is the case of people with HIV/AIDS, people under steroid treatments, and people taking chemotherapy. • People with diabetes also tend to develop fungal infections. • Very young and very old people, also, are groups at risk. MAJOR TYPES OF MYCOSES • • • • • Superficial Cutaneous Subcutaneous Systemic Opportunistic • Symptoms vary from cosmetic to life threatening CLASSIFICATION • Classified according to the tissue levels initially colonized. Superficial mycoses • Limited to the outermost layers of the skin and hair. An example: • Tinea versicolor • Affects the skin of young people, especially the chest, back, and upper arms and legs. • Tinea versicolor • Caused by a fungus that lives in the skin of some adults. • It does not usually affect the face. • This fungus produces spots that are either lighter than the skin or a reddish brown. CUTANEOUS MYCOSES • Extend deeper into the epidermis, and also include invasive hair and nail diseases. • These diseases are restricted to the keratinized layers of the skin, hair, and nails. • Host immune responses may be evoked resulting in pathologic changes expressed in the deeper layers of the skin. • The organisms that cause these diseases are called dermatophytes. • The resulting diseases are often called ringworm (even though there is no worm involved) or tinea. • Caused by Microsporum, Trichophyton, and Epidermophyton fungi, which together comprise 41 species. • One common disease is the athlete's foot which most commonly affects children before puberty. MYCOSES DUE TO SUBCUTANEOUS MYCOSES SYSTEMIC PRIMARY PATHOGENS • Involve the dermis, • Originate primarily in subcutaneous tissues, the lungs and may muscle and fascia. spread to many organ • Infections are chronic systems. and can be initiated by piercing trauma to the • Organisms that cause skin which allows the systemic mycoses are fungi to enter. inherently virulent. • These infections are difficult to treat. • May require surgical interventions such as debridement.(the removal of damaged tissue or foreign objects from a wound.) SYSTEMIC MYCOSES DUE TO OPPORTUNISTIC PATHOGENS • These are infections of patients with immune deficiencies who would otherwise not be infected. • Examples of immunocompromised conditions include AIDS, alteration of normal flora . by antibiotics, immunosuppressive therapy, and metastatic cancer • Examples of opportunistic mycoses include • Candidiasis (infection caused by yeast Candida, common cause of vaginal infections in women. ) • Cryptococcosis (systemic infection caused by Cryptococcus that affect the lungs, skin, or other body organs ,brain and meninges.) • Aspergillosis ( infections in the ear canal, eyes, nose, sinus cavities, and lungs) ANTI FUNGAL AGENT BASED ON MECHANISM OF ACTION Fungal cell wall synthesis inhibition: • Caspofungin. Bind to fungal cell membrane ergosterol: • Amphotercin–B, Nystatin. Inhibition of ergosterol + lanosterol synthesis: • Terbinafine, Naftifine, Butenafine. Inhibition of ergosterol synthesis • Azoles Inhibition of nucleic acid synthesis • 5–Flucytosine. Disruption of mitotic spindle and inhibition of fungal mitosis • Griseofulvin. Miscellaneous • Ciclopirox, Tolnaftate, Haloprogin, Undecylenic acid, Topical azoles. ROUTE OF ADMINISTRATION SYSTEMIC: • Amphotericin Ketoconazole, Caspofungin B, Fluconazole, Itraconazole, TOPICAL: • Terbinafine, clotrimazole, grizeofulvin, nistatin BASED ON STRUCTURE 1. Antibiotics A. Polyenes: • Amphotericin B Nystatin, Hamycin (AMB), B. Echinocandins: • Caspofungin, Anidulafungin Micafungin, C. Heterocyclic benzofuran: • Griseofulvin 3. Azoles A. Imidazoles Topical: • Clotrimazole, Econazole, Miconazole, Oxiconazole Systemic: • Ketoconazole B. Triazoles: (systemic) • Fluconazole, Itraconazole, Voriconazole, Posaconazole 4. Allylamine 2. Antimetabolite:• Flucytosine (5-FC) • Terbinafine 5. Other topical agents • Tolnaftate, Undecylenic acid, Benzoic acid, Quiniodochlor, Ciclopirox olamine, Butenafine, Sod. thiosulfate. Polyenes (Disrupt membrane structure & function) Azoles inhibit Flucytosine inhibits DNA synthesis POLYENE ANTIBIOTICS • Amphotericin B • Obtained from Streptomyces Nodosus • Amphoteric in nature • Polyene group- Multi lactone ring with conjugated double bond. • One end – Hydroxyl group (OH)–polar (Hydrophilc) MECHANISM OF ACTION Amphotericin B Binds ergosterol in fungal cell membrane Form pores in cell membrane • Other end – Hydrocarbon group-non polar (Lipophilic) Cell contents leak out Cell death MECHANISM OF ACTION ANTIFUNGAL SPECTRUM - Fungicidal at high & static at low conc. - Broadest spectrum of action • Aspergillus Blastomyces dermatitidis Candida albicans Cryptococcus neoformans Coccidioides immitis Histoplasma capsulatum Mucor spp. Also active against Leshmania RESISTANCE: • Replacement of ergosterol by other sterols in fungal plasma membrane. PHARMACOKINETICS • Poorly absorbed orally • Insoluble in water so colloidal suspension prepared with sodium deoxycholate (1:1 complex) • Plasma proteins bound 90% • Metabolized in liver • Slowly excreted in urine DI:• Flucytosine – synergetic action inc. permeability FC • Aminoglycoside inc. renal toxicity. ADVERSE EVENTS: – Acute reaction: – Chills, fever, headache, pain all over, nausea, vomiting, dyspnoea lasting 2-5 hrs because of release of IL & TNF – Long term toxicity: – Nephrotoxicity: Azotemia ( inability of the kidneys to excrete blood urea nitrogen) , Hypokalemia, acidosis, ↓ GFR – anemia – CNS toxicity : intrathecal administration, headache, vomiting, nerve palsies – Hepatotoxicity rarely USE:- Disadvantages of AMB • Useful drug in nearly all life threatening mycotic Nephrotoxicity infections • Treatment of invasive aspergillosis Acute infusion related reactions • Rapidly progressive Blastomycosis (Infection with a fungus called Hypopotassemia, anemia, hepatic Blastomyces dermatitidis) & dysfunction. Coccidiomycosis (caused by inhaling spores of the fungus Coccidioides immiti s) • Cryptococcus neoformans • Mucormycosis. • Disseminated rapidly progressing Histoplasmosis • Reserve drugs for resistant kala azar ( visceral leishmaniasis caused by L. tropica) • Topical uses: for oropharngeal candidiasis NYSTATIN:- Obtained from S.Noursei Similar to AMB In antifungal properties High systemic toxicity so used locally only Poorly absorbed from mucus membrane Available as ointment, cream , powder, tablet USES: In intestinal moniliasis (Yeast infection of the mouth and throat ) In vaginitis Prevention of oral candidiasis Can be used in oral, cutaneous, conjunctival candidiasis ADVERSE EVENTS: Gastrointestinal disturbances HAMYCIN:- S. Pimprina Hindustan antibiotics Pimpri More water soluble, fraction absorbed orally but unreliable in systemic infections Topical use in thrush (develops on the mucous membranes of the mouth ), cutaneous candidiasis, trichomonas & monilial vaginitis, otomycosis by aspergillus Natamycin: Similar to nystatin, broad spectrum Used topically 1%, 3% ointment For Fusarium solani keratitis (ocular infectious disease), trichomonas (sexually transmitted disease (STD) caused by a small organism called Trichomonas vaginalis.) & monilial vaginitis (Vaginal Yeast Infection) GRISEOFULVIN • Obtained from Penicillium griseofulvum • Fungistatic • Systemic drug for superficial fungal infections • Active against most dermatophytes • Narrow spectrum • Dermatophytes concentrate it actively hence selective toxicity • Resistance: • loss of drug concentrating ability • MECHANISM OF ACTION: • Griseofulvin interacts with polymerized microtubules and • Disrupts the mitotic spindles thus arresting fungal mitosis PHARMACOKINETICS: • Irregular absorption • Increased by fatty food • Gets conc in keratinized tissue ADVERSE EVENTS: • Headache most common • GIT disturbances • CNS symptoms: confusion, fatigue, vertigo • Peripheral neuritis • Rashes, photoallergy • Leukopenia, albuminuria (the presence of albumin in the urine). USES: • Systemically only for dermatophytosis, ineffective topically • In athletes foot (a fungal infection affecting mainly the skin between the toes) • Systemic azoles more effective and preferred. DI :• Induces warfarin metabolisrn • Reduces efficacy of oral contraceptives. • Phenobarbitone reduces the oral absorption and induces the metabolism of griseofulvin • failure of therapy may occur. :,f FLUCYTOSINE • Has useful activity against Candida and Cryptococcus. • Synthetic pyrimidine antimetabolite • Fungistatic MECHANISM OF ACTION • It is converted to antimetabolite 5-florouracil in a fungal but not human cell. • Inhibits thymidylate synthetase enzyme and • Thus DNA synthesis. • Should never be used alone, resistant may occur. Uses • Combination with itraconazole for treating chromoblastomycosis (chronic fungal infection of the skin and the subcutaneous tissue) • With amphotericin for treating cryptococcal meningitis in AIDS patients UNWANTED EFFECTS • Neutropenia • Thrombocytopenia • Bone marrow depression. • Nausea, vomiting ,diarrhea, • Severe enterocolitis (inflammation of both the small intestine and the colon.) • Hepatic enzyme elevation. 5-flucytosine permease 5-flucytosine (outside) (inside) Cytosine deaminase 5-fluorouracil 5dUMP (inhibits thymidylate synthase) RNA Phosphoribosyl transferase 5-FUMP Fdump(fluorodeoxyuridne monophosphate Mechanism of action of Flucytosine TERBINAFINE Orally & topically effective drug Against candida & dermatophytes Fungicidal : shorter courses of therapy required & low relapse rates Pharmacokinetics: Well absorbed orally 75% Highly keratophilic & lipophilic High protein bound , poor BBB permeability Negligible effect on CYP450 MECHANISM OF ACTION: • Acts as a noncompetitive inhibitor of ‘squalene epoxidase’, • an early step enzyme in ergosterol biosynthesis by fungi. • Accumulation of squalene within fungal cells appears to be responsible for the fungicidal action. • The mammalian enzyme is inhibited only by higher concentration of terbinafine. Acetyl CoA Squalene Allylamine Drugs (Terbinafine) Squalene epoxidase Squalene-2,3 oxide Lanosterol 14-α-demethylase (ergosterol) ADVERSE EVENTS: Nausea , vomiting , Diarrhoea Taste disturbances Rarely hepatic dysfunction Topical: erythema (superficial reddening of the skin) , itching, dryness , urticaria, rashes USES: • Topically as cream in tinea pedis (Infection that usually begins between the toes)/ cruris (fungal infection of the groin region) /corporis (superficial fungal infection of the arms and legs,) and Pityriasis versicolor (patches appear mainly on the chest and back) • Oral treatment reserved for onychomycosis (fungal infection of the nail.) , tinea capitis (a fungal infection of the scalp and hair shafts). • Efficacy in nail infection is ~80%. • Less effective against cutaneous and mucosal candidiasis. Mechanism of action of terbinafine ECHINOCANDINS Caspofungin, micafungin, anidulafungin • A new class of potent semisynthetic drugs • With large cyclic peptides linked to a long chain fatty acid • Have low toxicity compared to AMB. • Active mainly against Candida and Aspergillus. • Strains of candida that have become resistant to azoles are susceptible to caspofungin. MECHANISM OF ACTION • Inhibits the synthesis of β-1, 3glucan • which is a unique component of the fungal cell wall. • Cross linking between chitin and β1, 3-glucan gives toughness to the fungal cell wall. • Weakening of the cell wall leads to osmotic susceptibility of fungal cell, which then burst out. USE:• In deep and invasive candidiasis. • Esophageal candidiasis • In invasive aspergillosis. • Now increasingly used in neutropenic immunocompromised patients whose fever is not responding to antibacterial antibiotics. ADR:• An acute febrile reaction (reactions are fever, chills, pruritus, or urticaria,) • Phlebitis of the injected vein. • Rash, vomiting, dyspnoea, hypokalemia and joint pain may occur. TOPICAL AGENTS USED IN DERMATOPHYTE Tolnaftate: • An effective drug for tinea cruris and tinea corporis • Poor penetrability • Resistance does not occur. • Causes little irritation Ciclopirox olamine: • Penetrates superficial layers and reaches hair roots • Negligible Systemic absorption. • No irritation • Used in onychomycosis:Formulated as nail lacquer • Vaginal candidiasis :- as vaginal cream. • Effective in tinea infections, pityriasis versicolor and dermal candidiasis. • Undecyclenic acid: • Generally combined with zinc salt • Requires prolonged treatment has high relapse rate • Weaker antifungal action used in tinea cruris, tinea pedis and nappy rash (inflammation of a baby's skin caused by prolonged contact with a damp nappy) • Sodium thiosulfate: • A weak fungistatic, • Active against Malassezia furfur (a fungus species can cause tine a versicolor, folliculitis) • Effective in versicolor pitryasis BENZOIC ACID: • Fungi static-weaker than tolnaftate • Used in combination with salicylic acid • Whitfields ointment: ( benzoic acid 6% + salicyclic acid 3 %) • Salicyclic acid due to its keratolytic action helps to remove infected tissue & promotes penetration of benzoic acid in fungal infected lesion • Adverse events: irritation & burning sensation QUINIDIOCHLOR: • Luminal amoebicide • Weak antifungal & antibacterial • External application : Dermatophytosis , mycosis barbae (Ringworm of the beard) , pitryasis versicolor • Also used in vaginal creams for monilial and trichomonas vaginitis BUTENAFINE • A benzylamine congener of terbinafine • Same mechanism of action. Use:• Topically in dermatophytosis. • Efficacy in tinea cruris / corporis / pedis AZOLES • Synthetic anti fungals • Broad spectrum • Fungistatic / Fungicidal • Most commonly used • Classified as imidazoles & triazoles • Both these groups are • Structurally related compounds • Have same mechanism of action • Have similar antifungal spectrum • Imidazoles: • Two nitrogen in structure • Topical: • Econazole, Miconazole, Clotrimazole • Systemic : • ketoconazole (topically also) • Triazoles : • Three nitrogen in structure • Fluconazole, itraconazole, voriconazole, Terconazole • Fluconazole and itraconazole -----largely replaced ketoconazole for systemic mycosis • Because of greater efficacy, longer t½, as well as fewer side effects. • Some newer triazoles have been added. • Newer : Butaconazole, Oxiconazole, Sulconazole • Covering dermatophytes, Candida, other fungi involved in deep mycosis (except mucor), Nocardia and Leishmania THE MECHANISM OF ACTION • They inhibit the fungal cytochrome P450 enzyme ‘lanosterol 14demethylase’ • Thus impair ergosterol synthesis. • Leading to a cascade of membrane abnormalities in the fungus. • The lower host toxicity :- • Lower affinity for mammalian CYP450 enzymes • Lesser propensity to inhibit mammalian sterol synthesis. RESISTANCE:• Mutation of the gene • Encoding for fungal 14demethylase enzyme. • By enhanced removal from the fungal cell. Acetyl CoA Squalene Allylamine Drugs (Terbinafine) Squalene monooxygenase Squalene-2,3 oxide Lanosterol Azoles 14-α-demethylase (ergosterol) MICONAZOLE & CLOTRIMAZOLE KETOCONAZOLE • Topical use • First orally effective broad spectrum antifungal • Effective against • Cream, gel, spray, lotion, solution , pessary • Dermatophyte infections (pedis, cruris, corporis, versicolor) • Candida: oral pharyngeal, vaginal, cutaneous ADVERSE EVENTS: • Local irritation , itching or burning • Miconazole shows higher incidence of vaginal irritation & pelvic cramps • No systemic side effects • Dermatophytosis • Deep mycosis • Candidiasis PHARMACOKINETICS: • Requires environment absorption acidic for USE: • Restricted use, most serious mycoses • Dermatophytosis • Monilial vaginitis • Systemic mycosis: blastomycosis (Parasitic fungi affecting the skin or the internal organs), histoplasmosis (infection by a fungus confined to the lungs but can be fatal if spread throughout the body), Coccidioidomycosis (a serious fungal disease of the lungs and other tissues) • Less efficacious than AMB & produces slower response • Efficacy low in immunocompromized and meningitis • Lower toxicity than AMB higher than triazoles • So triazoles have replaced it in systemic mycosis • High dose used in cushings syndrome (a metabolic disorder caused by overproduction of corticosteroid hormones) • Topical: T.pedis, cruris, corporis, versicolor 38 DRUG INTERACTIONS: • Inhibits CYP450 enzyme ADVERSE EVENTS: • Nausea , vomiting , anorexia • ↑ Sr conc of cisapride, terfenadine, • Headache , paresthesia, alopecia • Reduces steroid, testosterone estrogen synthesis astemizole, quinidine & • Thus can cause gynaecomastia (enlargement of a man's breasts, usually due to hormone imbalance), • Oligospermia (deficiency of sperm cells in the semen), loss of libido (loss of sex drive) & impotence ( sexual dysfunction) in males. • Menstrual irregularities & amenorrhoea (an abnormal absence of menstruation) in females • Elevation of liver enzymes • Hypersensitivity reaction like skin rashes • Itraconazole or fluconazole, that have largely replaced it for systemic use. • Phenytoin toxicity • Sulfonylureas: hypoglycemia • Cyclosporine: nephrotoxicity • Warfarin: bleeding • Rifampicin, phenytoin ↑ metabolism of ketoconazole • Should not combine with AMB TRIAZOLE FLUCONAZOLE • Newer water soluble triazole • Oral, IV as well as topical • Broad spectrum antifungal activity • Candida, cryptococcosis, coccidioidomycosis • Dermatophytosis • Blastomycosis • Histoplasmosis • Sporotrichosis PHARMACOKINETICS: • 94% oral bioavailability • Not affected by food or gastric pH • Primarily excreted unchanged in urine • Poor protein binding (10-12%) • Widely distributed • Crosses BBB • T ½ -27-32hrs ADVERSE EVENTS: USES: • GIT upset • Headache, • Candida alopecia, skin rashes, hepatic necrosis • Teratogenic effect • CYP450 Enzyme inhibiting property less • No anti androgenic & other endocrine effects DRUG INTERACTIONS: • Effects hepatic drug metabolism to lesser extent than Ketoconazole • H2 blockers & PPI do not effect its absorption • Tinea infections candidiasis & • Disseminated cutaneous candidiasis, cryptococcal, coccidiodal meningitis & other systemic fungal infections • Candida UTI • Meningitis preferred drug • Eye drops for fungal keratitis (infection of the cornea) ITRACONAZOLE • Broadest spectrum of activity also against aspergillus • Fungistatic PHARMACOKINETICS: • 50-60% bioavailability • Absorption is variable, enhanced by food & gastric acidity • High protein binding 99 % • Well distributed accumulates in vaginal mucosa, skin, nails but CNS penetration is poor • Metabolized in liver CYP3A4 • Excreted in feces • T1/2= 30- 64hr ADVERSE EVENTS: • GI Intolerance • Dizziness, pruritis , hypokalemia, hypotension • Increase plasma transaminase • Rarely Hepatotoxicity headache, DRUG INTERACTIONS: • Oral absorption decreased by antacids, H2 blockers , and proton pump inhibitors • Rifampicin, phenobarbitone , phenytoin induce metabolism • Clarithromycin and HIV protease inhibitors reduce the metabolism of itraconazole and raise its blood levels. • Potentiates effect of hypnotic drugs • Inhibits CYP3A4 drug interaction profile similar to ketoconazole USES: • For paracoccidomycosis (a fungal infection caused by the fungus Paracoccidioides brasiliensis. )& chromoblastomycosis • For histoplasmosis, sporotrichosis (infection caused by a fungus called Sporothrix schenckii )& blastomycosis in AIDS patients • Esophageal, oropharyngeal, vaginal candidiasis • Dermatophytosis: less effective than fluconazole • Onychomycosis • Aspergillosis 43 VORICONAZOLE ADVERSE EVENTS: • Second generation triazole • Transient • High oral bioavailability, • Low protein binding visual • Good CSF penetration changes • Metabolized by CYP2C19 vision , altered color • Doesn’t require gastric acidity absorption for • T1/2-6 hrs USES: • DOC for invasive aspergillosis • Most useful for esophageal candidiasis • First line for moulds like fusarium (infestation with any of the fusaria or related moulds.) • Useful in resistant candidal infections like blurred perception & photophobia • Rashes in 5 -6 % • Elevated hepatic enzymes • Prolongation of QT THANK YOU -PHARMA STREET