* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Acute inflammation - immunology.unideb.hu
Periodontal disease wikipedia , lookup
Molecular mimicry wikipedia , lookup
Polyclonal B cell response wikipedia , lookup
Atherosclerosis wikipedia , lookup
Rheumatic fever wikipedia , lookup
Lymphopoiesis wikipedia , lookup
Hygiene hypothesis wikipedia , lookup
Adaptive immune system wikipedia , lookup
Immune system wikipedia , lookup
Acute pancreatitis wikipedia , lookup
Cancer immunotherapy wikipedia , lookup
Complement system wikipedia , lookup
Pathophysiology of multiple sclerosis wikipedia , lookup
Adoptive cell transfer wikipedia , lookup
Sjögren syndrome wikipedia , lookup
Rheumatoid arthritis wikipedia , lookup
Psychoneuroimmunology wikipedia , lookup
Immunosuppressive drug wikipedia , lookup
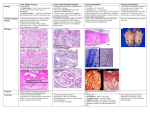
THE ACUTE INFLAMMATION AND ACUTE-PHASE RESPONSE Acute inflammation Acute inflammation is a protective response that is intended to eliminate the initial cause of cell injury, as well as the necrotic cells and damaged tissues resulting from the original insult, and to initiate the process of repair. The cells and molecules of host defense, including leukocytes and plasma proteins, normally circulate in the blood, and the goal of the inflammatory reaction is to bring them to the site of infection or tissue damage Triggers of acute inflammation • Infections (viral, bacterial, fungal, parasitic) & microbial toxins • Trauma, physical or chemical injury (e.g., thermal injury; irradiation; some environmental chemicals) • Tissue necrosis (e.g. ischemia) • Foreign bodies (splinters, dirt, sutures, crystal deposits) • Immune reactions (hypersensitivity and autoimmune reactions, which tend to persist, with features of chronic inflammation) Major components of inflammation – Vascular changes • Vasodilation • Increased vascular permeability • Increased adhesion of white blood cells – Cellular events • Recruitment and activation of neutrophils (polymorphonuclear leukocytes) and monocytes Classical signs of acute inflammation • • • • • Redness (rubor) Swelling (tumor) Heat (calor) Pain (dolor) Loss of function (functio laesa) Recognition of microbes and necrotic or damaged cells Macrophages and dendritic cells express different classes of pattern-recognition receptors that sense the presence of microbes and molecules from damaged or dead cells Robbins Basic Pathology (9th Edition) Activated macrophages secrete inflammatory cytokines Mast cells are also able to sense „danger”- and „stress”-signals ! ! http://dx.doi.org/10.3389/fimmu.2015.00238 Physical or thermal injury also activates mast cells Vascular changes Formation of oedema Robbins Basic Pathology (9th Edition) Vasodilation: histamine, prostaglandins, NO Increased vascular permeability: histamine, leukotrienes, bradykinin (15-30 min) TNF, IL-1 (hours) Activation of the complement pathways Cellular and Molecular Immunology, 8th ed., 2015 Elservier Mediator systems triggered by activation of factor XII Leukocyte recruitment and activation Mechanisms of neutrophil migration through blood vessels Margination and rolling E-selektin and P-selektin on endothelial cells /histamine, trombin, TNF, IL-1/ Adhesion • chemokines trigger conformational changes of integrins on the surface of neutrophils • Ligands for integrins on endothelial cells /TNF, IL-1/ Transmigration driven by chemokines /e.g. IL-8/ Chemotaxis Move toward sites of infection along a chemical gradient Chemotaxis of neutrophils • chemokines (e.g. IL-8) • leukotriene B4 • C3a, C5a • Bacterial products /N-formyl-metionin polipeptides/ • Products of collagen cleveage MMP: matrix metalloproteinase acPGP: N-acetyl Proline-Glycine-Proline – neutrophil chemoattractant Activation of neutrophils Robbins Basic Pathology (9th Edition) Neutrophils have the most efficient killing mechanisms among phagocytes Killing mechanisms of neutrophils (neutrophil extracellular traps) cathepsins, defensins, lactoferrin, lysozyme, NADPH oxidase, iNOS myeloperoxidase, elastase DNA, chatepsins, lactoferrin, myeloperoxidase, elastase Leukocytes are secreting harmful substances such as enzymes and ROS; therefore, they are important causes of injury to normal cells and tissues during inflammation! Large reserves of neutrophils are stored in the bone marrow and move in large numbers to sites of infection, where they act and then die Morphologic pattern of acute inflammation • serous • fibrinous • haemorrhagic • gangrenous • ulcerative • suppurative (purulent) The purulent exudate (pus) consists of creamy protein-rich fluid (liquor puris), neutrophils, debris of dead pathogens and necrotic cells. Certain organisms (e.g., staphylococci) are more likely to induce such localized suppuration and are therefore referred to as pyogenic (pus-forming). Abscesses are focal collections of pus. Kinetics of vascular and cellular events during acute inflammation Role of macrophages in acute inflammation Classical and alternative macrophage activation Cellular and Molecular Immunology, 8th ed., 2015 Elservier Role of matrix metalloproteinases (MMP) in inflammation They have role in: • chemotaxis • migration • antimicrobial activity (neutrophil elastase) • TNF release doi:10.1038/nri1418 Chemical mediators of acute inflammation Local and systemic actions of cytokines in inflammation Robbins Basic Pathology (9th Edition) IL-6 (IL-1) Acute-phase reaction Máj α1 antitrypsin, α1 antichymotrypsin protease inhibitors Acute-phase reaction Pentraxin family: CRP – opsonization, complement activation SAP – opsonization, complement activation, binding of mannose/galactose Collectin family: MBL – part of the complement system (SP-A/D – collectins of lungs) Complement proteins (C1-C9) Fibrinogen blood clotting The kinetics of acute-phase protein production in the blood The principal cell-derived and plasma protein mediators in acute inflammation Robbins Basic Pathology (9th Edition) EC: endothelsejtek Role of mediators in different reactions of inflammation Vasodilation – Histamine, prostaglandins, nitric oxide (NO) Increased vascular permeability – Vasoactive amines (histamine, serotonin), C3a and C5a (complement system), bradykinin, leukotrienes (LT), PAF Chemotactic leukocyte activation – Chemokines (e.g. IL-8), C3a, C5a, LTB4, TNF α, IL-1 Fever • IL-1, IL-6, TNFα, prostaglandins Pain • Prostaglandins, bradykinin Tissue damage • Neutrophil and Macrophage products – lysosomal enzymes – Reactive oxygen species (ROS) – NO Production of arachidonic acid metabolites and their roles in inflammation ! ! Robbins Basic Pathology (9th Edition) Outcomes of acute inflammation Outcomes of acute inflammation Features of chronic inflammation • Prolonged host response to persistent stimulus • Caused by microbes that resist elimination, immune responses against self and environmental antigens, and some toxic substances (e.g., silica) • Characterized by persistent inflammation, tissue injury, attempted repair by scarring • Cellular infiltrate consisting of activated macrophages, lymphocytes, and plasma cells, often with prominent fibrosis • Mediated by cytokines produced by macrophages and lymphocytes (notably T lymphocytes), with a tendency to an amplified and prolonged inflammatory response owing to bidirectional interactions between these cells