* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Chronic Inflammation
Atherosclerosis wikipedia , lookup
Molecular mimicry wikipedia , lookup
Rheumatic fever wikipedia , lookup
Periodontal disease wikipedia , lookup
Lymphopoiesis wikipedia , lookup
Polyclonal B cell response wikipedia , lookup
Immune system wikipedia , lookup
Adaptive immune system wikipedia , lookup
Cancer immunotherapy wikipedia , lookup
Sjögren syndrome wikipedia , lookup
Rheumatoid arthritis wikipedia , lookup
Adoptive cell transfer wikipedia , lookup
Hygiene hypothesis wikipedia , lookup
Immunosuppressive drug wikipedia , lookup
Innate immune system wikipedia , lookup
Today’s Quranic verse
God has revealed (from time to time) the
most beautiful Message in the form of a
Book, consistent with itself, (yet) repeating
(its teaching in various aspects): the skins of
those who fear their Lord tremble thereat;
then their skins and their hearts do soften to
the celebration of God's praises. Such is the
guidance of God: He guides therewith whom
He pleases, but such as God leaves to stray,
can have none to guide. [039:023]
1
“Every job is a self portrait of the person
who does it”
Autograph your work with excellence…!
2
CHRONIC INFLAMMATION
May 13, 2017
3
CHRONIC INFLAMMATION
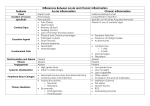
Specific Objectives:
1.
2.
3.
4.
5.
6.
7.
8.
9.
Describe the pathogenetic pathways leading to chronic inflammation.
List the principal cells of acute and chronic inflammation.
List the general features of chronic inflammation.
Outline the Classification of chronic inflammation.
Describe a granuloma and explain how it is formed.
Discuss the varying patterns of granulomatous reactions.
Discuss the Mononuclear Phagocyte System
Explain the functions of macrophages
Define the following macroscopic patterns of inflammation: serous inflammation,
fibrinous inflammation, purulent inflammation, hemorrhagic inflammation,
catarrhal inflammation, membranous & pseudomembranous inflammation,
abscess, ulcer, wound, scar, and keloid.
10. Describe the typical local and systemic signs and symptoms of inflammation.
11. Explain the pathogenesis of fever.
4
CHRONIC INFLAMMATION
It is defined as prolonged process in which destruction
and inflammation are proceeding at the same time as
attempt at healing.
Conditions favouring chronic inflammation
•Persistent infection by certain microorganisms
•Prolonged exposure to potentially toxic agent (exogenous /
endogenous)
•Local or general conditions impairing the body defence
•Autoimmune diseases
5
Chronic inflammation may develop in the following ways:
As a progression from acute inflammation if the original stimulus
persists,
After repeated episodes of acute inflammation,
De novo if the causative agent produces only a mild acute response.
6
GENERAL FEATURES OF CHRONIC INFLAMMATION
Acute inflammation
Demolition phase
Healing-repair & regeneration
Immune response
The hallmark of chronic inflammation
Presence of mononuclear inflammatory cells ("mononuclear cells",
"round cells", i.e., monocytes, lymphocytes, and/or plasma cells).
Some evidence of healing (scarring, fibroblast proliferation, angioblast
proliferation).
7
Acute inflammation
Exudation & pus formation in chronic suppurative conditions like
chronic brain abscess, osteomyelitis, empyema, pyosalpinx and
pyonephrosis
Fibrin presence in chronic empyema thoracis
Fluid exudation in chronic inflammations of serous sacs like
tuberculous peritonitis & spider web clot in CSF of tuberculous
meningitis
Usually however overt acute inflammation is not an outstanding
feature of chronic inflammation.
8
Demolition phase
Presence of macrophages commonly derived from emigrating
monocytes of bone marrow origin.
Healing
Repair
Presence of granulation tissue leads to repeated hemorrhage in peptic
ulcer and bronchiectasis resulting in hematemesis & hemoptysis
respectively.
9
Healing ( Repair)
Fibrosis seen in fibroproliferative tuberculosis, chronic peptic ulcer,
chronic cholecystitis and in the walls of chronic abscesses.
Cicatrisation leads to valvular stenosis and regurgitation in chronic
rheumatic valvulitis, pyloric stenosis in chronic gastric ulcers &
fibrous ankylosis in rheumatoid arthritis
Endarteritis obliterance in bed of chronic peptic ulcer, following
radiation damage & around gumma
10
Regeneration
In gall bladder cholecystitis glandularis proliferans
Regeneration of epithelium in ulcerative colitis leads to polypoidal
overgrowth & malignancy
Tumorlets in the lung in bronchiectasis
11
Immune response
B & T lymphocytes & plasma cells in granulation tissue
Extensive lymphoid infiltrate in Hoshimoto’s thyroiditis and
occasionally skin reaction to arthropod bite
Heavy plasma infiltrate in chronic inflammatory lesions of
juxtacutaneous mucous membrane
12
Note that the
activated
macrophage
releases products
that are similar
to those released
by PMN’s
13
CHRONIC
NON-SPECIFIC
INFLAMMATION
(NON-GRANULOMATOUS)
It is the continuation of a partially successful acute inflammation &
mostly reaction to persistent extracellular bacteria
Histologically characterized by structureless unorganized diffuse
infiltration of tissues by PMN’s and Round cells
Dominated by B cell immune response, with local amplification by B
cell-derived plasma cells secreting specific antibodies to enhance
bacterial phagocytosis and killing by WBC
Local tissue damage is caused directly by persistence of toxin
producing bacteria and indirectly by release of lysosomal enzymes
14
from host phagocytes, especially dead PMNs
15
16
17
18
19
20
21
22
23
24
CHRONIC GRANULOMATOUS INFLAMMATION
It is a special form of chronic inflammatory reaction which is
histologically characterized by presence of structured response with
recognizable single or coalescent units called granulomas .
It is dominated by cell mediated immune response (Type IV) when
microorganisms are present and generally show presence of T cells
and macrophages which transform locally into epithelioid cells and
giant cells.
It bypasses acute inflammation and is chronic from start .
Mostly it is reaction to facultative intracellular pathogens (TB bacilli,
fungi) or to inert indigestible foreign material (sutures, prostheses,
etc.) that do not cause direct cell injury and do not release
25
substances initiating acute inflammation.
GRANULOMA
An imprecise term applied to any small nodular delimited
aggregation of mononuclear inflammatory cells, or such a
collection of modified macrophages resembling epithelial
cells (epitheloid cells) usually surrounded by a rim of
lymphocytes, often with multinucleated giant cells. Some
granulomas contain eosinophils and plasma cells, and
fibrosis is commonly seen around the lesion.
While mostly granulomas are discrete & nodular, it does not usually have to be.
The process can be more diffuse, without the formation of actual granulomas.
This diffuse form of granulomatous inflammation is most often seen when an
individual's immune system is either innately hyporesponsive to a pathogen
(lepromatous leprosy) or compromised to the extent that it is difficult for the
inflammatory process to form discrete granulomas (tuberculosis seen in
persons with AIDS).
26
In its most classical form, a granuloma consists of
concentric layers of cells that, together, form the distinctive
lesion.
•This central focus is surrounded by a layer of specialized
macrophages, called epithelioid cells, and multinucleated giant cells.
The latter form as the result of cytoplasmic fusion of macrophages, due
to stimulation by a cytokine.
•The next layer is predominantly lymphocytes, and the outer layer is
most often fibroblasts, which are attempting to wall off the inciting
stimulus with fibrous connective tissue.
•Granulocytes, plasma cells, and other cells types may also be present.
27
*Macrophages are almost all recruited directly from the bloodstream
monocytes.
*Epithelioid cells have abundant pink cytoplasm, indistinct borders,
and elongated, euchromatin-rich, reticulated nuclei oriented helterskelter
*The giant cells of granulomas occasionally contain altered
cytoskeletal components in the shapes of stars, or asteroid bodies or
they may show presence of laminated calcified nuggets, called
Schaumann bodies ( "conchoid bodies").
*Plasma cells produce antibodies against the persistent antigen or the
altered tissue components.
*Lymphocytes are likely to be present even where there is no
involvement of the immune system.
28
If the agent is an inert foreign body, the granuloma will be of the non immune type.
However, if the inciting agent is antigenic, the lesion will be an immune
type of granuloma, in which the antigen-stimulated lymphocytes are
producing cytokines, such as interferon-gamma, to activate the
macrophages and their specialized forms (epithelioid and
multinucleated giant cells to heightened levels of microbicidal activity.
Classic granulomatous disease
Tuberculosis, leprosy, foreign body reactions (sutures,
schistosome eggs), the deep fungal infections, berylliosis, and
"sarcoidosis".
In syphilis (the granuloms, if any, are small and loose) and silicosis (the
granulomas, if any, are very fibrous).
29
30
31
32
33
34
TYPES OF GRANULOMATOUS REACTION
Granulomas with suppuration
(i.e., with pus in their centers; "stellate microabscesses") are typical of
those bacterial diseases with a propensity to involve lymph nodes.
These are lymphogranuloma venereum, cat scratch fever, brucellosis,
plague, tularemia, glanders-melioidosis, listeria, and yersinia infection
and blastomycosis.
Granulomas with caseation
are typical of certain fungal infections (histoplasmosis, blastomycosis,
and coccidioidomycosis ) and of mycobacterial (fungus-like bacteria)
infections (basically TB; also BCG bacillus and atypical mycobacteria)
35
Granulomas with foreign bodies
aspirated food, schistosome eggs, toxocara, silicone injections,
splinters, sutures, windshield fragments, chalazion, ruptured
epidermoid cysts, sea urchin spines, amyloidomas, dead aspergillus
fungi, dead filaria, ingrown hairs, talc in the lungs, metastatic
calcification bits, uric acid crystals (in longstanding gout,"tophi"),
sclerosing lipogranuloma of the penis, insect bites, * "actinic
elastolytic granuloma of Mieschler" (a foreign body reaction to your
own elastic fibers), etc.
36
Other solid granulomas are classified as immunologic
diseases:
Straightforward immune problems:
The organic pneumoconioses, berylliosis, zirconium disease (the
infamous "armpit sarcoidosis", from zirconium-based deodorants),
positive skin tests
More arcane immune problems:
Wegener's granulomatosis(and its variants Churg-Strauss and lethal
midline granuloma)
Immunologic reactions to tumors:
Lennert's lymphoma, seminoma (both are often rich in granulomas);
37
lymph nodes draining other cancers
Idiopathic (? immune) problems:
Sarcoidosis, Crohn's disease, primary biliary cirrhosis, bronchocentric
granulomatosis
Neutrophil deficiency syndromes:
“Chronic granulomatous disease“
Miscelleneous
Toxoplasmosis and Q-fever (curious little granulomas) and cutaneous
leishmaniasis ("foamy granulomas", present if immune response is
good).
HIV encephalitis presents groups of giant cells, the result of
macrophages recognizing HIV protein on each others' surfaces
38
39
40
41
42
43
44
45
46
47
48
MONONUCLEAR PHAGOCYTE SYSTEM
(Reticuloendothelial system-RES)
Consists of closely related cells of bone marrow origin including blood
monocytes and tissue macrophages, the latter are diffusely scattered
in connective tissue or clustered in organs (Kupffer cells in liver, sinus
histiocytes in lymph nodes, alveolar macrophages in lung &
Langerhan’s cells in skin)
Monocytes from blood migrate into various tissues and transform into
macrophages
Macrophage is a central figure in chronic inflammation. It can produce
wide range of biological substances active against both unwanted
invaders and the tissue
Macrophages can release Enzymes (neutral proteases & acid
hydrolases), Plasma proteins (complement components & coagulating
factors), Reactive metabolites of oxygen, Eicosanoids, Cytokines,
Growth factors and Nitric oxide.
49
Mononuclear Phagocyte System
•Circulating blood monocytes
•Tissue macrophages
Kupfer cells (liver)
Sinus Histiocytes (spleen)
Microglia (CNS)
Alveolar Macrophages (lung)
50
51
Differences between Acute & Chronic inflammation
ACUTE
Vascular Changes
Cellular Infiltrates
CHRONIC
Vasodilation
Minimal
Increased permeability
Minimal
Primarily neutrophils
Mononuclear
leukocytes,
macrophages
Stromal Changes
Minimal
Fibrosis, cellular
Edema and
proliferation
separation of layers
scarring.
52
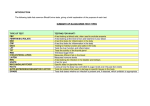
Comparison of Acute and Chronic Inflammation
Process
Acute Inflammation
Chronic Inflammation
Initiators
Microbial surfaces & fragments
Injured tissue & tissue fragments
Mediators
Mast cell products (histamine)
Bradykinin
Lysosomal components
Complement, lipid mediators
Non-digestable organisms
Non-degradable foreign matter
Auto-immune reactions
T-lymophocytes& macrophage
products- cytokines and GF’s
Proteases and reactive oxygen
Complement, lipid mediators
Vascular changes Vasodilatation & inc, permeability
Minimal
Cell
Populations
Neutrophils
Tissue macrophages
Monocytes/Macrophages
Plasma cells, Fibroblasts
Time course
years
Acute onset, minutes days
Insidious onset, weeks
Outcome
Resolution, Abscess formation
Chronic inflammation
Resolution, Tissue destruction,
53
fibrosis
54