* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Thyroid Nodules
Survey
Document related concepts
Transcript
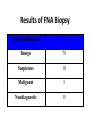
In The Name Of God Thyroid Nodules (Epidemiology;Etiology &Pathogenesis) Nodule definition A discrete lesion within the thyroid gland that is due to an abnormal focal growth of thyroid cells. -Benign -Malignant (Hyper;Hypo Or Normo- function) Factors associated with thyroid nodules • Iodine deficiency • Genetics: -Family clustering -Monozygotes -Sex differences(F>M) -Mutations(Tg;NIS;Tpo;TSH-R;Pendrin) -Chromosoms(14q;Xp22;3q26) • Environmental: -Cigarette smoking -Infections -Drugs -Goiterogens Thyroid Nodules: Differential Diagnosis • Subacute Thyroiditis •Metastasis • Prior thyroid surgery •Lymphadenopathy • Thyroid hemiagenesis • Cystic hygroma • Aneurysm • Bronchocele • Laryngocele •Thyroglossal duct cyst •Parathyroid cyst/adenoma ((History;Physical Exam ;US&….)) Clinical findings in favor of malignancy • Historical features: -Age:<20 or >60 -Male sex -Neck irradiation(childhood) -Rapid growth -Change in speaking;swallowing or breathing -FH of thyroid malignancy or MEN-2 -The coexistence of any other malignancy, such as HL, non-Hodgkin’s lymphoma or any other cancer • Ph.E: -Firm & irregular consistency -Fixation -Vocal cord paralysis -Regional lymph adenopathy US findings in favor of malignancy -Hypoechoic lesion -Irregular margins -Calcification -Absence of halo -Internal or central blood flow *Low suspicion -Echo-Free (cystic) lesion -Homogeneous hyperechoic lesions Thyroid nodules in adults • palpation :3-7% of adults • More common in women than men(4 times) • Cysts are the most frequently encountered solitary palpable nodules.(one-third) • U/S: 20% of all women • U/S: 50% of women > 50 y. have nodules • US:>60% In healthy adults • In autopsy series:50% • Increase linearly with: -Age(0.1% annually) -Exposure to ionizing radiation(2% annually) -Iodine deficiency Thyroid nodules in adults-Cont. • The most important thing is to distinguish benign from malignant causes • the incidence of malignancy is greater in solitary nodules than multiples. • Multiple nodules does not imply the nodules are benign. • Most thyroid nodules are benign(95%) • Hyper- or hypothyroidism suggests benignity • But most patients with thyroid nodules have normal thyroid function tests. • Possibility of cancer regardless of nodule size is about 5% and its prevalence is 2-3 times more often in women. • Nodule size is not predictive of malignancy and cancer is not less frequent in small size nodules(<10mm) • Mortality rate is higher in men. Results of FNA Biopsy Cytologic Diagnosis % Benign 70 Suspicious 10 Malignant 5 Nondiagnostic 15 NONDIAGNOSTIC *Repeat Cyst > 4 cm Diagnostic Operate Follow *%15 of nondiagnostic aspirate may represent malignant nodules. %50 Benign LT4 ? Follow *Suspicious Malignant Surgery *%10 to %20 are malignant at operation. Cystic nodules • • • • • %15 to %25 of all nodules. 2% to 4% are malignant. False negative & Nondiagnostic(FNA) Treat surgically cysts > 4cm. Half of them disappear after one or more aspirations. • Suppressive therapy is ineffective. Benign thyroid nodule Observation for 1 year Thyroid ultrasound Size decreased Size unchanged Size incresed FNA Continue observation Benign nodule Malignant or suspicious LT4 suppression For 1 year Ridgway,Ann intern Med 1998 Surgery Thyroid ultrasound Size decreased or unchanged Continue LT4 therapy Ridgway,Ann intern Med 1998 Size increased Surgery Benign thyroid nodule Burch,1995 Trial of LT4 therapy TSH 0.1-0.5 mu/l for 6-12Mo. Obtain US at baseline and 6-12 Mo. Larger Smaller Unchanged Surgery Stop LT4 , observe Nodule growth Restart LT4 No change Follow ,off LT4 Benign thyroid nodule T4 for 12 Mo. To keep TSH less than 0.1mu/l Increase in size D/C T4,Rebiopsy or surgery No change in size D/C T4 Decrease in size D/C T4 and observe OR Decrease T4 to keep TSH At the low end of NL range Cooper,1995,JCEM Thyroid Cancers • Incidence : – (~9/100,000 per year) ;increases with age, plateauing after about age 50. – Twice as common in women as men. – male sex is associated with a worse prognosis. • Associated with: – Radiation: • predisposes to chromosomal breaks, leading to genetic rearrangements and loss of tumor-suppressor genes. • It increases the risk of benign and malignant thyroid nodules,associated with multicentric cancers, and shifts the incidence of thyroid cancer to an earlier age group • Children seem more predisposed to the effects of radiation than adults • radiation derived from 131I therapy appears to contribute little, if any, increased risk of thyroid cancer. Cont. – TSH and Growth Factors: • Many differentiated thyroid cancers express TSH receptors and, therefore, remain responsive to TSH. – Oncogenes and Tumor-Suppressor Genes: • cancers are monoclonal in origin(mutations that confer a growth advantage to a single cell.) • impaired apoptosis • Specific mutations for tumor phenotype. • nonspecific mutations. Specific cancers • PTC • FTC • MTC • ATC • Lymphoma Papillary Thyroid Cancer • Most common type (70 to 90% of well-differentiated thyroid malignancies) - Age: 20-30 • Microscopic PTC :25% of thyroid autopsies. • Pathogenesis : RET rearrangements -Activation of receptor tyrosine kinases (RET/PTC, TRK, MET) →Produce chimeric proteins with tyrosine kinase activity • BRAF V600E mutation in ~50% of cases(PCR of biopsy - more aggressive PTC) • Detection of RET rearrangements by PCR of thyroid biopsies or peripheral blood in 20 to 40% of PTCs on chromosome 10. (Chernobyl Nuclear Accident). • RET translocations cause some papillary cancers. • Thyroglobulin is an excellent tumor marker. • TSH dependent? • APC gene mutation for familial adenomatous polyposis and Gardner’s syndrome: higher incidence of PTC. MTC • • • • • • • • • • • • ~5% of thyroid cancers malignant tumor of calcitonin-secreting C cells 75% sporadic & 25% hereditary(AD) Genetical:As a part of either a MEN- 2A or MEN -2B Familial: MTC without other features of MEN Variable age (Sporadic/MEN):sixth and seventh decades in sporadic forms. more aggressive in MEN-2B than in MEN-2A familial MTC is more aggressive than sporadic MTC 5 to 10% of thyroid cancers RET mutations in some sporadic cancers. Calcitonin is an excellent tumor marker All patients with MTC should be tested for RET mutations. (point mutations that induce constitutive activity of the tyrosine kinase .) Follicular Thyroid Cancer • • • • • • • • • Less common than papillary Age 40-50 TSH dependent? Often caused by a chromosomal translocation fusing the genes encoding Pax8 (transcription factor) and PPARg (nuclear receptor of thiazolidinediones).. Thyroglobulin is an excellent tumor marker The incidence of FTC varies widely in different parts of the world. it is more common in iodine-deficient regions. RAS mutations are found in some FTCs. Loss of heterozygosity (LOH), consistent with deletions of tumorsuppressor genes, is particularly common in FTC, often involving chromosomes 3p or 11q. Anaplastic carcinoma • Predominantly in persons older than 70 years. • High mortality:most die < 1 year. • One third arise in preexisting differentiated cancers . • Mutations of the tumor suppressor gene, p53. Questions?