* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download PowerPoint - New Page 1
Cardiovascular disease wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Electrocardiography wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Coronary artery disease wikipedia , lookup
Jatene procedure wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Heart failure wikipedia , lookup
Cardiac surgery wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
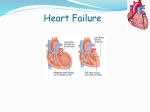
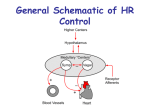
Pathophysiology of Brain & Body USSJJQ-20-3 Heart Failure Introduction Heart function… pump sufficient blood to organs to… furnish oxygen/substrates and remove metabolites… thereby maintaining ‘steady-state’ (homeostasis) Heart failure (HF) ventricular contraction compromised such that... heart cannot meet demand or… can only do so at raised ventricular pressure Increased workload & reduced cardiac reserve A symptom complex rather than a single disease Types Chronic - eg congestive heart failure (CHF) Acute - eg myocardial infarct not usually classed as heart failure (different ICD code to HF) CHF Incidence (USA) ~ 5.3 million people in the USA (2006) estimated that similar number have unsuspected HF Circa 2% of the population has HF 75-80% of these > 65 years of age Approx 660,000 new cases each year likely to develop symptoms in the next 1-5 years HF 3 million visits to the doctor 1 million hospitalisations per year (2009) CHF Burden (USA) Approx 57,000 deaths in 2009 A leading cause of hospitalisation for > 65 years old The risk of death is 5 - 10% per year (mild symptoms), 30-40% (severe symptoms) $25-40 billion on care of HF patients $8-15 billion on hospitalisations ~ $10,000 per admission (~1,000,000 admissions in 2005) rest in medications, home health care, etc does not include indirect costs (eg lost productivity) Incidence of heart failure, by sex and age, 1995/96, Hillingdon Cowie MR et al (1999) European Heart Journal 20: 421-428 Heart Failure Common, Deadly, Expensive, ‘Epidemic’ Risk Factors Coronary Artery Disease, previous MI Hypertension Obesity Diabetes, Dyslipidemia Valvular disease; eg aortic valve stenosis Drug/disease-induced myocardial dysfunction Smoking Congenital defects Cardiac Output (CO) and Cardiac Reserve CO is the volume pumped per ventricle per min CO = heart rate (HR) x stroke volume (SV) Cardiac reserve is the difference between resting and maximal CO (5 L/min vs 30 L/min) Eg CO (ml/min) = HR (75 beats/min) x SV (70 ml/beat) HR is the number of beats per minute SV is the volume of blood pumped out by a ventricle with each beat (SV = EDV – ESV) = 5250 ml/min or 5.25 L/min Low CO in HF essentially a problem with SV CO = HR x SV : Control of Stroke Volume Preload – amount ventricles are stretched prior to systole Contractility – cardiac cell contractile force due to factors other than EDV set by End Diastolic Volume Eg circulating epinephrine Afterload – back pressure exerted by blood in the large arteries leaving the heart Ie pressure against which ventricle is ‘pushing’ SV and Preload : Starling’s Law of the Heart The heart is a ‘demand pump’ It always attempts to pump what returns to it (Venous Return) Greater VR greater filling greater stretch greater force greater stroke vol greater CO Starling’s Law of the Heart SV and Preload: Starling’s Law of the Heart SV and Afterload Before it can actually pump blood, the ventricle must expend energy generating a pressure > arterial pressure ie > diastolic pressure Some of the work done by the heart muscle is ‘wasted’ by not pumping blood during isolvolumetric contraction SV and Contractility Contractility is a change in contractile strength independent of stretch/EDV ↑ contractility ↑ Stroke Volume ↑ in contractility comes from: ↑ sympathetic activity Hormones such as epinephrine ++ and some drugs Ca Law of Laplace: the physics of failure Wall tension in ventricle reflects the minimum work the muscle must perform to just shorten T = P x r / 2H T = tension P = pressure r = radius H = wall thickness Can rearrange P Raised preload = T x 2H r overfilling ventricles ↓ H, ↑ r so ↑ T needed to generate same P needed to eject blood Raised afterload ↑ P needed to eject blood So ↑ T needs to be produced, all other things equal Categories of Heart Failure Chronic (CHF) Acute (MI) High output Low output Systolic Diastolic Right-side Left-side High/Low Output High output Rare Excessive need for CO, even at rest Causes do not reflect inadequate heart Severe anaemia Hyperthyroidism Arteriovenous shunts (low resistance pathways) Low output Most common Impaired pumping ability Eg ischaemic heart disease Systolic Impaired ejection during systole ↓ in contractility & ejection fraction Typical causes… Ischaemic Heart Disease (2/3rds of Sys HF), cardiomyopathy Hypertension, valvular (eg aortic) stenosis Affect contractile activity Cause pressure overload in ventricle Results in ↓ ejection fraction Can be as low as 15% (normally 65%) Causes ↑ in EDV, dilation, pressure Law of Laplace means this is not good! Diastolic Impaired filling during diastole Leads to congestive symptoms Caused by… Myocardial hypertrophy (eg caused by hypertension) ↑ ventricular wall thickness Ischaemic Heart Disease Delayed ventricular relaxation Mitral valve stenosis ↓ O2 so ↓ ATP (needed to pump Ca++ and break actomyosin) Poor ventricular filling Features Ventricular hypertrophy abnormal remodelling ↓ chamber size ↓ventricular compliance ‘stiffer’ chambers more difficult to fill Right-sided Impaired pumping of blood to lungs Leads to… Damming of blood in systemic veins ↑ in systemic venous, r. atrial, r. vent. ED pressures Fluid movement to interstitial spaces Oedema, especially lower regions Backup in liver and portal vessels → Impaired liver function Impaired digestion Ascites Weight gain through fluid retention Left-sided Impaired pumping of blood to systemic circ. Leads to… Damming of blood in pulmonary vessels ↑ in pulmonary, L. atrial, L. vent. ED pressures Fluid movement to pulmonary interstitium Impaired gas exchange Cyanosis, shortness of breath Oedema Symptoms Due to ↑venous/capillary pressure ‘damming’ of blood and salt/water retention Nocturia Return of fluid from interstitial spaces in tissues to plasma when supine Dyspnea (shortness of breath): cardinal sign ↑ diffusion distance due to pulmonary oedema Worse when lying down (↑ VR pulm congestion) Especially at night (paroxsymal nocturnal dyspnea) Bronchospasm due to excess fluid (cardiac asthma) Above arise from altered microcirculation fluid dynamics Cyanosis Bluish mucosal membranes/skin ↓ oxygenation in lungs + ↑ extraction in tissues Physiological Response to HF Response to ↓ SV & ↓ CO ↑ Sympathetic tone and (nor)epinephrine ↑ heart rate and contractility NE/E can ↑ TPR and, therefore, afterload Na+ & H2O retention Via activation of RAS by ↓ RBF & ↓ BP ↑ SV by ↑ ventricular filling (Frank-Starling mechanism) Frank Starling mechanism CO can be normal at rest due to ↑ ED V & P Exercise-induced ↑ in CO at high ED V & P Can be counter-productive by ↑ ‘volume load’ on heart Can lead to pulmonary congestion/shortness of breath Myocardial hypertrophy Like skeletal muscle, cardiac response to exercise Can get abnormal remodelling of chamber → ↓ volume Compensated vs Decompensated If physiological responses restore CO Compensated If physiological responses fail to restore CO Decompensated ↑HR ↑TPR ↑ afterload Na+ & H2O retention ↓ diastolic filling time Over-stretching of ventricles Development of oedema Further responses exacerbate the situation Therapeutics Diuretics Beta-adrenergic blockers Vasodilators Captopril, Enalopril Angiotensin II receptor antagonists Nitrates (eg nitroglycerin) ACE inhibitors Carvedilol Losartan Positive inotropic drugs Cardiac glycosides Sympathomemetics Phosphodiesterase inhibitors Cardiac Contraction Only 10% of myocardial cell volume is cytoplasm Na + channels open for 1-2 msec Slow Ca++ channels open and conc ↑ Contractile protein activation occurs K+ channels open and K+ efflux restores RMP Ca++ channels close Ca++ conc returned to normal by Ca++ pumps May wish to bolster contraction short-term but ‘unload’ heart long-term – a therapeutic tightrope! Possible Interventions ↑ Na+ influx ↑ Ca++ loading of the SR Maintain Ca++ concentration Inhibit K+ channels Greater Ca++ release ↓ Ca+ extrusion Larger depolarisation Prolong depolarisation ↓ adrenergic stimulation ‘unload’ the heart recovery Digitalis Glycosides Extracted from the foxglove plant Effective range = 1.0 - 2.5 ng/ml But toxic range = 1.5 ng/ml and up ! ↑ cytoplasmic Na+ conc Inhibits Na+, K+-ATPase (sodium pump) arrhythmias ↓ gradient inhibits Na+ influx which is… coupled to Ca++ efflux so… increases Ca++ retention & loading in the SR Relieves symptoms, but does not ↑ survival Diuretics: reversing renal retention Drugs which ↑ Na+ & H2O excretion ↓ ECF volume, oedema ‘Unload’ ventricular filling Normally, < 1% filtered Na+ /H2O excreted Filtered load is circa 600 g/day & 180 L/day Topologically, filtrate is external to body + + Reabsorption of Na is active, via Na pump Reabsorption of H2O is passive, no H2O pump Relies on hydrostatic & osmotic forces + By heart & Na pump Common Diuretics Types Loop diuretics Thiazides eg acetazolamide Osmotic diuretics eg bendrofluazide Carbonic anhydrase inhibitors eg frusemide eg mannitol K+ sparing eg spironolactone Loop diuretics Eg: Frusemide/Furosemide Most powerful diuretics Affect up to 20% filtered Na+ load excreted Mode of Action Thick (ascending) segment of loop of Henle Inhibit Na/K/2Cl carrier via Cl-binding site Misc venodilator action seen clinically in the treatment of heart failure gives symptomatic relief occurring before the onset of diuretic action From Martinez-Maldonado, M, and Cordova, HR: Cellular and molecular aspects of the renal effects of diuretic agents. Kidney Int. 1990, 38:632-641. Loop Diuretics – unwanted effects ↑ Na+ conc reaching the distal tubule Results in ↑ loss of H+ and K+ Exchangers are driven more Hypokalaemia arrhythmias, convulsions Metabolic alkalosis Hypovolaemia low cardiac output