* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Lecture 15 – Effector Functions of Humoral Immunity:
Complement system wikipedia , lookup
Major histocompatibility complex wikipedia , lookup
Monoclonal antibody wikipedia , lookup
Lymphopoiesis wikipedia , lookup
DNA vaccination wikipedia , lookup
Immune system wikipedia , lookup
Molecular mimicry wikipedia , lookup
Cancer immunotherapy wikipedia , lookup
Psychoneuroimmunology wikipedia , lookup
Adaptive immune system wikipedia , lookup
Polyclonal B cell response wikipedia , lookup
Innate immune system wikipedia , lookup
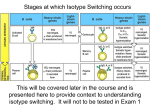
IMMUNOLOGY NOTES Lecture 2 – Intro to Immunology Angiten: chemical substances that elicit a specific immune response Innate Sys: phagocytes, NK cells, serum proteins (complement, CRP, MBP) Innate System recognizes well-conserved structures s/a LPS, PepG, dsRNA, etc Adaptive Sys: made up of T cells and B cells. These cells express “clonally restricted, antigen-specific cell surface receptors”. (TcR and BcR). These receptors recognize antigen and activate their respective cells. While both B and T lymphocytes have Ag receptors, the mechanism by which they recognize Ag differs. BcR is similar in structure to antibody (Ig) and can recognize any chemical structure that is floating around. TcR requires Ag to be presented by MHC located on APCs. “Naïve” Lymphocyte: lymphocyte which has never seen Ag. (As opposed to memory lymphocyte) Cardinal features of adaptive response: specificity, diversity, memory. Memory = the 2nd time a T/B sees Ag, its response is both faster and stronger. Due to 1: clonal expansion during initial Ag exposure & 2)differences in functional responses between naïve lymphocytes and memory lymphocytes. Adaptive System is divided into humoral and cell-mediated immunity. Humoral: mediated by antibody (the secreted product of B cells). Largely directed against extracellular pathogens (eg bact, parasites) Cell-Mediated: mediated by T cells either directly or through action of secreted cytokines. Largely directed against intracellular pathogens (some bact, viruses). There are 2 types of T cells: helper T cells (TH, CD4+) and cytotoxic T cells (CTLs, CD8+). In response to antigen, CD4s secrete cytokines, while CD8s kill the cells directly. Primary Lymphoid Organs: where leukocytes develop and mature. For all leukocytes except T cells, this is the bone marrow. The T cells it is the thymus. FC: What are the secondary lymphoid organs? Ans: Lymph nodes, spleen, mucosal immune system, cutaneous immune system. It is to these secondary lymphoid organs that the naïve B and T lymphocytes home once they have matured. It is in these secondary lymphoid organs that the B and T initially encounter Ag and where the immune responses are generated. All secondary lymphoid organs are highly organized into specialized B and T areas. B areas are called follicles while T areas are known as interfollicular zones. T cells traffic through the secondary lymphoid organs using the blood and lymphatic system. Adjuvant: a substance which causes local inflammation. Generally speaking, adjuvants activate macrophages and dendritic cells in the tissues activating them to present Ag to T cells in the secondary lymphoid organs. Most microbes contains one or more natural adjuvants. Lymphocyte Recirculation: Lymphocytes, particularly naïve Ts, constantly recirculate through the secondary lymphoid organs. Naïve lymphocytes leave the blood through HEV and enter the T cell area. (B cells migrate to the follicle). If the lymphocytes don’t encounter Ag, they leave through the efferent lymphatics. They then either go to other lymph nodes via afferent lymphatics, or reenter circulation via the thoracic duct. Each T cell hits one lymph node each day (estimate). Ie: A given specific T cell does not remain in its one lymph node forever. It moves around to other lymph nodes too. Lecture 3 – Antibody and TcR Assembly of Antibody: The variable region of IgH is made up of V,D,J gene segments. Once the VDJ region is formed, it is spliced together to the constant region to form a mature IgH. A similar process takes place with IgL, but there are only V and J (no D) gene segments. Antibody molecules are assembled from a large number of individual gene segments. This process is known as somatic gene rearrangement. It occurs during B development in the bone marrow. Gene segments are known as V, D, J. During the course of an immune response (c/o!!) antibody molecules undergo changes in their variable regions to increase affinity, and in their constant regions to change effector functions. TcR: Similar to antibody. chain is analogous to IgL ( looks like L) while chain is analogous to IgH ( looks like ‘H’). Like Ig molecules, the TcR is assembled from numerous gene segments by somatic gene rearrangement. chain has V,D,J while chain has only V and J. CDR1 and CDR2 are primarily responsible for interacting with MHC while CDR3 is responsible for interacting with peptide antigen. Unlike Ig, TcR does not undergo structural changes during the immune response. Somatic Gene Recombination is controlled by lymphocyte specific proteins known as RAG-1 (recombinase activating gene) and RAG-2. Defects in RAG genes prevent recombination which means that no mature B or T cells can be formed. D and J are joined first. Then V. The variable region is then spliced to the constant region (which is also variable—determines which Ig in B cells. Not as important in T cells). If for any reason rearrangement is unable to generate a functional BcR or TcR, the cell dies. (see previous bullet). Once a mature receptor has been generated, they still must go through some final checkpoints to eliminate those B and T that do things like recognize self-antigen (negative selection). TcR undergo additional selection to ensure that only those receptors that require MHCs can go on. Mecanisms of Generating Diversity: 1)Combinatorial association of VDJ regions. 2)Pairing of the two different receptor chains (, ). 3)P-region addition 4)Nregion diversification. - P-region addition: imprecise cleavage/splicing of the VDJ regions with addition or deletionof nucleotides - N-region diversification: addition of nucleotide sequences between gene segments by the enzyme terminal transferase. - In all cases, the major location for diversity is at the junctions. It is the hypervariability of these junctional regions that gives rise to the CDR3 regions (principally responsible for Ag recognition). Allelic Exclusion: Receptors can only be expressed at the cell surface in dimer form. So the heavy chains are expressed along with pre-B or pre-TcR. Cell surface expression of a functional heavy chain with a pre-receptor chain means that successful rearrangement has occurred. A signal is sent down to the cell to inform it to cease further rearrangement. This ensures that only a single receptor is expressed. At this point the immature B and T cells (now expressing functional TcR/BcR) can undergo positive and negative selection. Negative Selection: those cells that recognize self-MHC with high affinity and therefore are potentially autoreactive are induced to die by apoptosis. Ig but not TcR undergo further molecular changes: - Isotype switching: delete the intervening DNA between the VDJ and the new isotype C region. - Somatic hypermutation: Random mutations in the V regions. Those that lead to lower affinity cells are induced to die. - Switch to secreted Ab: Splice the Ig mRNA coding for the transmembrane exon protein. 6 – MHC and Antigen Presentation The principal function of MHC is presentation of protein antigen to TcR. MHC-I is present on nearly all cells (except RBCs). – antiviral immunity MHC-II is present only on pro-APCs (Bs, dendritic cells, Macrophages).DTH/humoral immunity They are also responsible for self/non-self discrimination. (the principal cause of graft rejection) Awos: MHC alleles control immune responsiveness and graft rejection. MHC Restriction: T cells can only recognize antigen when presneted in combination with self-MHCs. Only MHC I (2 microglobulin) chain is not polymorphic. I, II and II are all polymorphic. (Ie: The 2 chain on MHC-I is identical for all MHC-Is). - Each variant MHC-I allele is encoded by a single chain. - Each variant MHC-II allele is encoded by both an and a chain. - This means that you have 6 different MHC-I molecules (genes) in your halotype. Because MHC-II has two chains, you have 12 different possible molecules for that one. Certain polymorphic MHC alleles are linked to resistance for disease (eg HLAB*5301 for malaria) as well as for autoimmunity (HLA-B27 – ankylosing spondylitis) In order for MHC-Ag to be presented, the Ag must first be “presented” to a T by an APC. ?? Dendritic cells tend to capture antigen at initial site of infection. They then run off to a lymph node so they can present it to a naïve T cell. FC: What is the purpose (other than ID!) of CD4/8? The CD4/CD8 co-receptor MHCI presents to CD8+ and MHCII presents to CD4+. interacts with the non-polymorphic chains during activation. Ie: CD8 interacts with 3 domain of MHCI and CD4 interacts with II chain of MHC-II. Each MHC molecule (I and II) are coded for by three different gene loci. MHC-I is coded for by HLA-A, HLA-B, HLA-C on chromosome 6. Each of those loci has many different possible alleles. Similarly, MHC-II is coded for by HLA-DP, HLADQ, HLA-DR also on chromosome 6. Each person has a specific HLA-A allele, HLA-B allele, HLA-C allele. If there were 5 different alleles of each, each halotype has a 1/125 chance of being identical. However, recall that there are 2 chromosomes… (MHC genes are expressed codominantly). Halotype: the entire set of MHC genes on each chromosome. Anchor Residues vs TcR Contact Residues: the part of the peptide that binds to the MHC is called the anchor residue. The part that binds to the TcR is called the contact residue. Only MHCs bound to peptide are stably expressed at the cell surface. (If inside the ER a peptide does not get bound, the MHC will be destroyed). MHCs are unable to discriminate between self and foreign peptides. IFN (eg by NK, CD4) increases MHC expression and Ag presentation.(in addition to activating macrophages, etc) MHC Class I Pathway (cytosolic proteins): 1. cytosolic proteins are degraded by the proteosome 2. residues are transported into ER by TAP 3. protein is bound to MHC and sent off to the surface - if a person is deficient in TAP, they are susceptible to viral infections MHC Class II Pathway (proteins in endosomes/phagosomes) 1. phago/endosome fuses with lysosome to form phagolysosome which degrades peptides and transported into the ER. 2. Meanwhile, inside the ER, class II MHCs are bound to invariant chain protein (occludes the peptide groove) 3. MHCII-Ii and peptide are transported into a vesicle called ‘MHC class II compartment’ (MIIC) where Ii is attacked by proteases leaving only a peptide called CLIP. Another protein called HLA-DM catalyzes removal of CLIP allowing the peptide to bind to the MHC. - Question: what keeps these peptides from binding to MHC-I? - “II = Ii” 7 – T Lymphocyte Activation TcR/CD3 Complex: The TcR dimer is expressed along with other molecules, most importantly, the CD3 complex. Because the TcR cytoplasmic tails are so short, the T cell needs the CD3 to delve into the cytoplasm to deliver the message. Signal Transduction in T activation: The CD3 complex has ITAM(s) attached to each chain. Phosphorylation of ITAM allows molecules containing SH-2 domains to bind. The most important of these molecules in T activation is ZAP70. When a T cell encounters Ag (with MHC, of course!), TcR and CD3 are recruited to the site of interaction. CD4/8 is recruited as well. On the cytoplasmic tail of CD4/8 is a tyrosine kinase called p561ck or Lck. It is Lck that phosphorylates the ITAMs on the CD3 which then allows ZAP70 to bind. Activated ZAP70 triggers a variety of events such as: Ca; activation of MAPK pathway; activation of calcineurin; Also transcription factors that promote cytokine gene expression. Eg: NFAT, AP-1, etc IOW: 1)T/Ag interact. 2)Recruit CD3, CD4/8. 3)Lck on CD4/8 phosphorylates ITAMs on CD3. 4)ZAP70 binds and is activated by ITAMs. 5)ZAP70 exerts effects by phosphorylating multiple substrates (eg RasMAPK). CD4/CD8 Coreceptors: see above… Adhesion Molecules: Provide adhesion of the TcR to the APC. (Requires > 4-6 hours for full activation). Eg The integrin LFA-1 (ICAM-1); CD2 (LFA-3). Adhesion molecules do not “work” unless the TcR is bound to an antigen. Costimulatory Molecules: Eg: CD28, CD40L. Also known as the second signal. Essential for proper activation of T cells. Without 2nd signal anergy. CD28 is present on essentially all T cells and binds to B7 found on APCs. CD40L (reg of B7; Induce IL-12; isotype switching) is upregulated on activated Ts. Interacts with CD40 found on a variety of APC. CD40 activation on macrophages causes upregulation of costimulatory B7s, activates macorphages, induces IL-12, etc. CD40 activation on B cells upregulates B7 co-stimulation and induces B cells to undergo isotype switching. Note how CD40 signalling is important for both CMI and humoral immunity. Patients with deficiencies in CD40L (hyper-IgM) exhibit profound defects in both cell-mediated and humoral immunity. A “resting” APC is co-stimulator deficient. Initially, the APCs (eg macrophage) do NOT have B7, CD40, etc. However, if they are activated (eg by innate immune system), they will upregulate their co-stimulator molecules. FC: How is CD40 induced? Ans: By TcR signalling (following activation from an antigen). Role of IL-2: IL-2 causes clonal expansion of T cells When a T cell becomes fully activated it upregulates expression of IL-2 (“T cell growth factor”). It also upregulates expression of the high-affinity IL-2 receptor. (Ie: Autocrine action). ITAMs: found in a wide variety of cell-surface signalling molecules involved in signal transduction in the immune system. FC: Phases of the T cell immune response (from naïve T): Ans: 1)Ag is presented to naïve T by APC. 2)T (CD4 or CD8) is activated and secretes IL-2 and upregulates IL-2R. This causes proliferation 3) IL-2 also causes differentiation: CD4 into CD4 effectors and CD4 memory cells. Same thing with CD8. 4)CD4 effectors activate Bs/Ts; activate macrophages; inflammation. CD8 effectors lyse target cells and activate macrophages. Signal 1 vs Signal 2: The TcR provides signal 1. The costimulatory molecules are known as signal 2. Signal 2 is essential to achieve full activation. In fact, without signal 2, you get anergy. Turning off T immune response: (3 mechanisms illustrated here) 1. No Antigen: As antigen is reduced, TcR stimulation is decreased, and so therefore is IL-2. Absent IL-2, T cells will die by apoptosis. 2. Too Much Antigen: In the presence of very high concentration of antigens, T cells can be induced to undergo apoptosis via Fas/FasL pathway. 3. Time: >96 hours after stimulation, T cells upregulate CTLA-4. CTLA-4 binds B7 with twenty-fold higher affinity (removes costimulation). Also, CTLA-4 dephosphorylates the ITAMs and ZAP70. APPON: Classes of Lymphocytes: 1. B Lymphocytes secretion of antibodies 2. CD4 Lymphocytes secretion of cytokines activation and proliferation of B (into plasma cells) and CD8 lymphocytes (into cytotoxic effectors) ; Activation of macrophages; Inflammation 3. CTL target cell lysis 4. NK target cell lysis Lecture 15 – Effector Functions of Humoral Immunity: Methods by which Ab enhance immune response: 1. Neutralize a toxin/pathogen by binding/blocking imp site 2. Opsonize (make phag more efficient; the Ag/path with bound Ab is gulped down by phags expressing receptors for Fc portion of the Ab attached to the Ag. ) 3. ADCC (target pathogen for direct killing) 4. Activate complement ( opsonization; inflammation; lysis via MAC) Effector functions of the different Ig isotypes: IgM: BcR on naïve B cells; When secreted can be fixed by complement; affinity since no affinity maturation has occurred; pentamer ( avidy for Ag) IgD: BcR on naïve cells but no secreted form IgG: most important Ig for infections; opsonization; activates classical pway of complement; ADCC; neonatal immunity; feedback inhibition of B response IgA: 10- B Lymphocyte Activation 1. 2. 3. 4. 5. 6. 7. 8. Humoral Response (general features) BcR and signal transduction Role of complement in augmenting B specific antigen responses Early signals following BcR Role of T cells and CD40L in humoral responses Role of cytokines in isotype switching (Eg: IFN-gamma IgG) Germinal Center reaction and affinity maturation Role of Ig in feedback inhibition of humoral response Plasma Cells: Some antibody-secreting cells end up in bone marrow where they differentiate into plasma cells. Plasma cells produce low, basal levels of antibody giving continuous protection. Another few B cells will become memory cells. Germinal Center Reaction: affinity maturation, isotype switching and generation of memory B cells Once activated Bs differentiate into antibody-secreting cells, they typically still remain in the peripheral lymphoid organ (in which they were activated). Their antibodies enter the circulation. Question: Why is it that the secondary response can only be induced by protein antigens? FC: What is meant by “Thymus-dependent humoral response”? Ans: Humoral response to protein antigen requires Ts in addition Bs. These are referred to as “Thymus-dependent humoral responses” (TD). The T cells are needed to help by secreting cytokines and expressing CD40L which together help with isotype switching and affinity maturation. Humoral response to non-protein antigens does not require T cells and are referred to as “Thymus-independent humoral responses” (TI). Ie: Thymus dependent vs independent refers to the requirement of T cells. Question: Exactly which processes take place in the germinal centers? FC: What are some of the functions carried out by antibodies? Ans: neutralization, opsonization, A?, complement activation FC: What is important about CD40 on B cells? BcR and initiation of Signalling: The BcR of naïve B cells is IgM. (Of course, this can/will change if isotype switching occurs later). IgM is associated with two other chains called Ig-alpha and Ig-beta (analogous to CD3 complex in T cells). These two chains contain the ITAM motifs which, when phosphorylated, attract Syk (analogous to ZAP70). Note: If the antigen is also attached to complement product C3d, this will complex with CD21 on the B cell and enhance activation about 1000 times! Role of CD40: CD40, located on B cells needs to interact with CD40L found on T cells. Engagement of the B cell’s CD40 allows: isotype switching, affinity maturation, secretion, generation of B memory cells. Also upregulation of B7. FC: Describe the process for B Activation beginning with a naïve B cell in a peripheral lymphoid organ. List the main effectors. Activation usually occurs in the lymph node. A filtered antigen binds the BcR. Activation leads to changes that are essential for effective interaction with CD4s. These include: processing of antigen and subsequent presentation along with MHCII. Upregulation of B7 and other costimulatory molecules. Upregulation of cytokine receptors (in preparation for the Cyk’s to be obtained from the T cells). AWOS: Upregulation of B7 and Cyk receptors. Migration into T-cell rich area. - Antigen activated B cells then enter the T region to present their antigens. The Ts have recently been activated by the same antigen presented by dendritic cells. Both the B and T cells receive stimuli from each other. The T gets Ag/MHC and costimulation. The B gets cytokines for growth and differentiation and CD40L for germinal center reactions. - FC: Describe the process of B/T bidirectional interaction from the point that the B first presents antigen to the T: The B cell presents antigen to the T. The T responds by expressing CD40L and secreting cytokines. The B cell is now induced to proliferate and differentiate. Isotype Switching: changing the IgH from one Ig type to another. Because the switch is always “downstream” (i.e. via deletion of intervening DNA), they can never revert to IgM. Similarly, they can never go from a downstream type to an upstream one. Isotype switching is defective in certain types of immunity. Isotope switching requires T cells. For cytokines and CD40 engagement.(IFN-gamma for IgG; IL-4 for IgE; TGF-beta for IgA. No signal, of course, will result in remaining IgM). Affinity Maturation: During the course of an immune response, the average affinity of an antibody for an antigen changes. This is due to point mutations taking place in the CDRs of V regions of both light and heavy chains. Because activated B cells need continual feedback from BcR to survive, those receptors with higher affinity will bind antigen and survive, while those that have low affinity will not. Again, be aware that affinity maturation requires CD40L. Therefore, this is limited to thymicdependent antigens. Thymic In/Dependent: Affinity maturation only occurs for hymic-dependent agents” (ie proteins, AA?) because in thymic-independent antigens, no CD40 or Cytokine are produced. Thymic independent produce only low affinity IgM. Switch to Secretion: occurs by splicing out part of the Ig mRNA coding for transmembrane and cytoplasmic regions. Generation of Memory Cells: Even once the response is over, a small fraction of antibodies will be found to have gone on to become memory cells. The mechanism is not known. However, CD40 is essential. Another few will become plasma cells. Germinal Center: All of the reactions take place in the germinal center, aka secondary follicle. This is a specialized region that forms in the primary follicles in an absolutely T-cell dependent way. Germinal center formation fades after the Ag stimulus is removed. FC: How is B activation ended? Late during the humoral response, antigen-ab complexes crosslink the BcR with Fc receptors on B cells. This inhibits further B activation. 11 – Cytokines and Cytokine Receptors 1. General properties of cytokines 2. Function of cytokines during the innate immune response 3. Role of TNF, IL1, chemokines in regulation of inflammation and leukocyte recruitment. 4. Cytokines produced in response to viral infection 5. Function of cytokines during the adaptive response 6. Differentiation and function of Th1 vs Th2 think…. IFN-γ: think macrophage activation TNF: think inflammation Helper T cells: think production of cytokines Cytokines: think “the means by which cells of the immune system communicate. Function of TNF, IL-1: think inflammation via recruitment of luekocytes (via upregulation of endothelial adhesion molecules and chemokines). IL-12: think potent activator of Th1 pathway Type I Interferon: think anti-viral Flashcards: FC: Give 2 examples by which prolonged cytokine production can be deleterious: TNF-alpha sepsis; IFN-gamma loss of tolerance/autoimmunity FC: Give an example of pleitropy and redundancy in cytokines: Pleiotropy: IL-4 IgE antibody production, Th2 differentiation; inhibition of macrophages. Redundancy: IL-2, IL-4, IL-5 all stimulate B proliferation. FC: Main cytokines produced during innate response. Who secretes them. Primary Function. TNF-α, IL-1, IL-12, Chemokines. Secreted by macrophages and NK cells. Modulation of innate immunity; Inflammation; Leukocyte recruitment; Induction of adaptive response. FC: Main cytokines produced during adaptive response. Who secretes them. Primary Function. IL-2, IL-4, IL-5, IFN-γ. Secreted by T cells. Regulation of adaptive response; Regulate lymphocyte growth/differentiation; Activation of effector cells. FC: Main functions of IL-12: 1. Potent activator of Th1 pathway (IL-4 is activator of Th2); 2. Enhancement of cytolytic activity of CTL and NK cells. FC: IFN-α and IFN-γ: aka type I interferons. Important in anti-viral immunity. Inhibits viral replication. Increases the number of MHC molecules on infected and neighboring cells (thereby enhancing presentation of viral peptides). Notes Cytokines work by altering the pattern of gene expression on the target cell. All cells produce and respond to cytokines Expression of cytokine receptors is also tightly regulated. Unlike hormones, cytokines do not usually act at a distance. Rather they are shortacting, often on the cell with which the secreting cell is interacting. Some functions of cytokines: Proliferation of activated lymphocytes; Isotype switching; Plasma cell development; Lineage commitment of CD4s to Th1/2; Macrophage activation; Hematopoiesis aspects SEE SLIDE 6… INNATE VS ADAPTIVE CYTOKINES… Cytokines of innate: TNF-α, IL-1, IL-12, IFN-α, IFN-β. FC: What is the principal function of TNF and IL1? Activate endothelial cells causing them to upregulate adhesion molecules and chemokines in order to recruit leukocytes. Ie; Promotion of the inflammatory response. (TNF/IL1/IL6 also act on the liver to secrete acute phase proteins for anti-microbial affinity). TNF/IL1/IL6 act on the liver to induce the acute phase response which greatly enhances anti-microbial immunity. Acute phase proteins bind specifically to bacteria and opsonize them. FC: Give an overview of the innate response to bacterial infection: Nearby macrophage responds to the LPS on the bacterial wall by quickly secreting TNF and IL1 and IL-12. (Note: we have not yet activated the macrophage). This causes recruitment of leukocytes to the site of infection. A little while after, the IL-12 kicks in and causes CD4 to differentiate into Th1 which secretes IFN-γ. The IL-12 also activates NK cells which also secrete IFN-γ. The IFN-γ now activates the macrophages so that they have phagocytic activity. TNF in septic shock: systemic release of TNF results in systemic inflammation (edema, etc) Cytokines in the adaptive response: Once a T cell (both CD4 and CD8) has been presented with antigen, it begins to secrete IL-2. It also upregulates IL-2R. IL-2 is the principal growth factor for T cells. This autocrine loop drives T proliferation and activation. Now that activated T cell can begin secreting its other cytokines. Question: what are other functions of IL-2? [proliferation of Ts, Bs, and NKs??—I think so…] Phases of CD4 activation: Recognition: The CD4 responds to an APC. Activation: It responds by secreting IL-2 which causes expansion into many CD4s. Effector: The various CD4s secrete their various cytokines… FC: List the cytokines secreted by the Th1 and Th2 pathways: Th1: IFN-γ, IL2. Th2: IL-4, IL-5, IL-10, IL-13. FC: Which of the Th pathways are concerned with humoral immunity? Broadly speaking, Th1 cytokines regulate cell-mediated immunity. Th2 cytokines regulate humoral immunity. FC: Give the innate cytokines that influence the choice of CD4 pathway. List which cells typically stimulate production of those cytokines. IL-12 produced by the innate response to bacteria induces Th1. IL-4 produced by the innate response to parasites/nematodes, induces Th2. Question: the innate response produces IL-4??? FC: Actions of IFN-γ: macrophage activation; isotype switching to opsonizing bodies (IgG); development of Th1; increased MHC expression/presentation. FC: Actions of IL-4: induction of Th2; isotype switching to IgE; inhibition of macrophage activation. Overview of cytokine receptors: Most are heterodimers with an α chain and an β (or γ) chain. The α chain is the binding while the β (or γ) is the signalling unit. Remember that these chains are shared (which explains both pleitropy and redundancy). FC: Mechanism for cytokine receptor signalling: The mechanism is phosphorylation of the cytosolic part of JAK kinases (analogous to ITAMs) which allows STAT (SH-2 protein—analogous to Syk and ZAP70) to bind. Phosphorylation of STAT causes gene transcription. NOTE: This is only for type I and type II cytokine receptors. Things like TNF and IL-1 each have different receptors. (Eg: TNF has a cell death pathway via caspases). X-Linked SCID: IL2, 4, 7, 13, 15 all share a common γ chain which is defective in this disease. This means lots of problems in generation and regulation of immune response. “Bubble Boy Syndrome”. Question: What about ADA deficiency??? VIROLOGY NOTES INTRODUCTION TO VIRUSES MORPHOLOGY Energy-less: they float around until they come in contact with an appropriate cell Composed of nucleic acid and a protein coat (capsid). Some have lipid envelopes (from membranes). Contain all the genetic information to build replicas—but not the enzymes. Nucleic Acid: single vs double stranded; linear vs loop; segmented vs nonsegmented; one simple message vs hundreds of proteins Capsids: two types: icosahedral vs helical Envelope: can get from cell membrane, golgi, nuclear membrane (as the viruse leaves the cell). RNA VIRUSES 3 types of RNA: single-stranded (most common), double-stranded (one), retrograde (one) + means just like mRNA and thus, can be translated right away by the host’s ribosomes - means it must be converted to + RNA prior to translation Retrovirus: must be converted to DNA which must then be transcribed to +RNA. To convert RNA to DNA (!) these viruses carry a unique enzyme called reverse transcriptase. RNA Dependent RNA Polymerase: Because a negative-stranded RNA needs to be transcribed into a + strand, -RNA viruses must carry in their capsid this enzyme. (Human cells do not have this enzyme). DNA VIRUSES: DNA must first be transcribed into mRNA (by using the + strand as a template). The – strand is simply ignored. CAPSIDS Two types: icosahedral (polypeptide chains capsomer triangle icosahedron). Helical: capsomers bound to DNA which coil. DNA VIRUSES: (HHAPPPy) Double stranded; Icosahedrals; Nuclear replication Herpes, Hepadna, Aeno, Papova, Parvo, Pox EXCEPTION: Parvo: single-stranded “PAR One” EXCEPTION: Pox: ‘Pox in a Box’ i.e. complicated DNA (hundreds of proteins), complicated capsid structure ENVELOPES: (Half—the middle 3) hhAPPpy) RNA VIRUSES (PC-CRaFT-FARBOP-Reo) Most: Single stranded; Cytoplasmic replication; Enveloped; Helical 4 Groups: +Naked; +Enveloped; -Enveloped; (no + env); ds naked Picorna, Calici; Corona, Retro, Flavi, Toga; Filo, Rhabdo, Adeno, Bunya, Orthomyxo, Paramyxo; Reo) picorna (small i.e. comes first); Flavius’s Toga; most are enveloped (middle 2 of the 4 groups) EXCEPTION: replicate in nucleus: Retro, Orthomyxo EXCPEPTION: Icosahedral: picorna, calici, flavi, toga, reo Transcription, Translation, Replication + RNA: Adsorption, Penetration, Uncoating sans probleme. +RNA (since it is identical to mRNA) is translated directly using cell ribosomes, proteins, enzymes. For replication, the +RNA must be transcribed into –RNA which is what is needed to have as a template for replication of new +RNA progeny. Finally you get assembly and release. - RNA: Adsorption, Penetration as normal. In the uncoating process, the RNA Dependent RNA Polymerase enzyme is released into the cytoplasm. Immediately, +RNA strands are generated using the RNA Dependent RNA Polymerase. Translation: Translation begins. Replication: The +RNAs can be used to make many –RNA progeny. DNA Viruses: transcription and replication typically occur in the nucleus; translation occurs in the cytoplasm. DNA Transcription is divided into three phases: Immediate early; Early; Late. Immediate early and Early is when 1)enzymes are encoded for replication and for 2)transcription of late mRNA. Late Transcription:Late is when capsids are made. Late mRNA is usually transcribed after DNA replication has begun. Late mRNA is transcribed from progeny mRNA. Late mRNA is used to make capsids. Assembly and Release and Host Outcome Naked Virions: released via lysis or exocytosis Enveloped: get their membranes by budding through nuclear membrane, golgi, cell membrane Host outcome either death (cell loses its functions when virus takes over); or transformation: Infection introduces or activates oncogenes.