* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download 9/5/08 Transcript I
Photosynthesis wikipedia , lookup
Peptide synthesis wikipedia , lookup
Fatty acid synthesis wikipedia , lookup
Butyric acid wikipedia , lookup
Evolution of metal ions in biological systems wikipedia , lookup
Nitrogen cycle wikipedia , lookup
Genetic code wikipedia , lookup
Microbial metabolism wikipedia , lookup
Catalytic triad wikipedia , lookup
Metalloprotein wikipedia , lookup
Citric acid cycle wikipedia , lookup
Biochemistry wikipedia , lookup
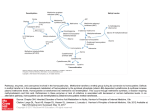
Dr. Baggott 9-5-08 10-11 am Note: I highlighted the parts I believe are relevant to the email Whikehart sent out regarding Monday’s test. Please know that other parts may be important, but these were the obvious ones. Last time we left of with Maple Syrup urine disease which is a favorite question for the people who make up boards to ask. If you have a block in this metabolism you build up keto acids of the branch chain amino acids and they then smell like maple syrup. That is the way this is diagnosed. Begins at page 9 of “Overview of Amino Acid Metabolism” packet. (Page has a 5 in top right corner) G. Phy → Tyr (Phenylketonuria) Let’s look at the catabolism of Phenylalanine. Phe goes to Tyrosine this is Catalyzed by Phenylalanine hydroxylase. One of the cofactors in Phenylalanine hydroxylase is Tetrahydrobiopter. If you have a block here, if your enzyme is no good here, you’ll have PKU (Phenylketonuria) also one of the things that the board people will pick on Pku is diagnosed early in life (Alabama will automatically do a test for PKU) because the treatment for PKU is simply a low phenylalanine diet. Turns out that ketoanalogs of phenylalanine are fairly toxic if you keep the diet low in phenylalanine the child will grow up normally and have normal mental and physical attributes. Most of PKU is due to the block in enzyme 1 which is the phenylalanine hydroxylase. There is a dihydrobiopterin reductase that can be also blocked in about 1-2% of PKU patients and if you have a block here you treat this patient with Biopterin. Conceptual Question often seen on boards: If you have a patient with PKU: What amino acid that is not essential for us now becomes essential? (they can’t do this metabolism) ANS- Tyrosine. G. Tyr →→→ acetoacetyl-CoA + furnarate Tyrosine’s catabolism is uninteresting. It goes to this intermediate in fatty acid metabolism and furnarate. I never ask questions about these because they’re so uninteresting; I don’t like them. I only ask questions on stuff I like. H. Family belonging to one carbon metabolism Of course you know we’re going to start overlapping things here. Sorry! That is the way you can learn better, if you have overlapping amino acids in different groups. i. Ser ↔ Gly Serine and Glycine belong to the family of one-carbon metabolism because Serine can be converted to Glycine in a reaction which transfers one carbon from Serine to a carbon acceptor which is tetrahydrofolate to form methylene tetrahydrofolate. Serine has 3 carbons. Glycine has 2 carbons. 1 carbon was transferred. This is a major source of one-carbon fragments that sit on folic acid (or that folic acid has) This one-carbon fragment will be used to synthesize purines and pyrimadines…and do other things also. So we’ll see that this is a major source: this beta carbon of serine is a major source of one-carbon fragments. We’ll see later that we can oxidize or reduce this 1-carbon fragment from the methylene state, we can oxidize it to the formal state of can reduce it to the methyl state. Reaction reversible but in our bodies it goes forward because we need these 1-carbon fragments. But theoretically, it is reversible. ii. Glysine cleaving enzyme utilizes glycine to put a methylene group on tetrahydrofolate. This is irreversible and only occurs in mitochondria. This reaction does not go backwards mainly because you have CO2 and ammonia formed. But this is an active enzyme in the mitochondria of liver and kidney and certain other organs. So, we can also get a 1-carbon fragment from glycine. Page 8 of “Overview of Amino Acid Metabolism” packet. (Page has a 6 in top right corner.) iii. His Histidine we’ve already discussed. Histidine is metabolized to formiminoglutamic acid and formimino group is then transferred to tetrahydrofolate (also a source of 1-carbon fragments) The formimino group then can also be reduced to other forms of 1-carbon fragments. iv. Met Methionine is a complicated one and they pick on this on boards a lot because it is so complicated. A major metabolic pathway for methionine is to convert it to S-Adenosyl-Methionine. You condense it with ATP and produce S-Adenosyl-Methionine. This is an irreversible reaction since you are creating pyrophosphate and phosphate here. What we do with methyl group on S-Adenosyl-Methionine? Here is the group that is important. (points the methyl group to the right of the box labeled “L-Methionine Adenosyltransferase) We are going to use that for methylation reactions. You will see more about this later. We will go over this again and again and again… Methionine becomes S-Adenosyl-Methionine. You take off a methyl group and it becomes S-Adenosyl-Homocysteine. S-Adenosyl-Homocysteine is simply S-AdenosylMethionine without the methyl group. What are the methyl acceptors? Oh-about 100 of them! That is not all that important. What I want you to get is that there is a lot of acceptors of the methyl group. That is why they have acceptors here, not just specific compounds. S-Adenosyl-Homocysteine is hydrolyzed to Adenosine and Homocysteine. Now we have to do something with this homocysteine. How many of you have heard that homocystinuria or homocystinemia (high homocysteine in the blood) is a risk factor for cardiovascular disease? (pause…and nobody answers) They are marketing all kinds of vitamin preparations to lower blood homocysteine levels. In normal metabolism if you don’t have a block in this enzyme, you will condense homocysteine with serine to form cystathionine. That will be hydrolyzed to cysteine and alpha-ketobutyrate which will be metabolized to propionate and on we go. Important thing to remember in this metabolic pathway is (will be on boards) is that homocysteine donates no carbons in the synthesis of cysteine. It donates what atom? Sulfur. If you have this pathway operating, you have no requirement for cysteine. You can make cysteine from methionine. Methionine yields homocysteine, homocysteine donates it’s sulfur to serine to form cysteine. Serine and cysteine have the same number of carbons. So did we learn about the catabolism of methionine, or the production (anabolism) of cysteine, or both? The answer is both. This is both the catabolism of methionine and the anabolism of cysteine. If you have a block at this synthase enzyme, then you have Homocystinuria and they also test for that in Alabama for kids because it leads to skeletal malformations (…and stuff like that) I. Family leading to acetoacetyl CoA: Lys, Trp Tryptophan and Lysine are so uninteresting, you can just white these out! They’re metabolized to compounds that are in the fatty acid oxidation pathway. They are so uninteresting, I can’t stand them. So, I never ask questions about them. i. Trp →→→→ acetoacetyl CoA niacin formation is a minor pathway ii. Lys →→→→ acetoacetyl-CoA J. Thr → Gly + acetaldehyde Threonine is odd-man-out. Threonine is a 4-carbon amino acid and it is cleaved to 2 2-carbon fragments. Threonine aldolase is just a term for the same enzyme called serine hydroxymethyl-transferase. (this was the enzyme that converted serine to glycine). It has other activites. It has about 20 other activities. It is in huge concentration in your liver. It is a major major enzyme in your liver and it also does this reaction. They just call it Threonine aldolase to distinguish which reaction it is catalyzing. So, threonine is odd-man-out as far as putting into any family. Page 11 of “Overview of Amino Acid Metabolism” packet. (Page has a 7 in top right corner.) IV. Biosynthesis of non-essential amino acids Synthesis of non-essential amino acids. Why aren’t we going over synthesis of the essential amino acids? Because if you could make them, would they be essential? No. So, we’re not going to do that. If you are really interested in how they’re made, go to your book and do that. I’m not interested in how they’re made. Ok, the non-essential ones are: o Alanine o Arginine o Asparagine o Aspartate o Cysteine o Glutamic o Glutamine o Glycine o Proline o Serine o Tyrosine We’re going to go over these pretty fast because you already know how they’re made. (with a few exceptions) Page 10 of “Overview of Amino Acid Metabolism” packet. (Page has a 8 in top right corner.) We can make glutamic acid in two different ways. o Transaminate alpha-ketoglutarate. o Reversible reaction called glutamate dehydrogenase. (dehydrogenases require the nicotinamide coenzymes. That is why they’re called dehydrogenases.) This enzyme catalyzes the removal of ammonia from glutamic acid if we want to make ammonia. If is reversible so it catalyzes this fixation of ammonia if you want to make glutamic acid. So, we can make glutamic acid through transamination or this glutamic acid dehydrogenase. We’ll see when we make urea, we can generate ammonia by running the reaction in the reverse direction. It is reversible. How do we make glutamine from glutamic acid? We need a glutamine synthetase, that’s obvious. Synthetase reactions require ATP. You put an amide group on the side-chain acid of glutamine. Glutamine synthetase. How do we make Alanine, Alpha-ketoglutarate or oxaloacetate? How do you make alanine, glutamine, aspartate? Transamination reactions. 1 step. Alpha-ketoglutarate goes to glutamic acid. Oxaloacetate goes to aspartic acid. Run it the other way and: pyruvate goes to alanine. Alanine goes to pyruvate. How do you make asparagines? Well, we had a glutamine synthetase. I’ll bet you mother nature makes asparigine with an asparagine synthetase. Same mechanism-the ATP ammonia here, converte aspartic acid to asparigine, add an amide nitrogen to the side chain of carboxylic acid. Glycine and Serine? We can get glycine from serine and we can also get serine from glycine theoretically. This pathway in the reverse is probably not that important. How do we get serine from the important pathway? This is an intermediate in glycolysis. That’s all I want you to know. This intermediate in glycolysis contains 3 carbons. Serine contains 3 carbons. We’re going to metabolize it right to serine. I don’t care about the intermediates. Just know it is an intermediate in glycolysis. (and now, the quote of the day) “Mother nature is usually very thrifty.” If you’ve got a 3 carbon intermediate in glycolysis and you need a 3 carbon amino acid, it is going to use that because it doesn’t want to waste time and energy using other things. Page 13 of “Overview of Amino Acid Metabolism” packet. (Page has a 9 in top right corner.) Cystine: we already saw that the catabolism of methionine and the biosynthesis of cysteine are one in the same. Homocysteine and Serine condense to form Cystathionine compound which is hydrolyzed. Homocysteine transfers it’s sulfur from serine to cysteine. Cysteine is just serine with the OH on the side chain replaced by sulfur. Phenylalanine: We’ve already seen how tyrosine is synthesized. Proline. You’ve been told that the catabolism of something is probably not the way you make something. So, catabolism and anabolism are not the same pathway. In the case of proline, it is. Proline comes from glutamic acid. We can make proline. If we need glutamic acid, we run the reaction here. If we need proline, we run the reaction this way. All these steps are reversible. Page 4 of “Biosynthesis of Urea” packet. (Page has a 113 in top right corner) Fig. 25.15 The allosteric regulation of glutamine synthetase activity by feedback inhibition. Glutamine synthetase is a very important reaction. That is why I devoted one special slide to it. We take glutamic acid in the presence of ammonia ATP and we make glutamate. Notice this captures ammonia and we will deal with that real soon when we discuss urea biosynthesis. We are going to use that amide nitrogen (not the amino nitrogen) on side chain to make purines, (which will go into purine skeleton) will use that to make pyrimadines (on side chain nitrogen in pyrimadines) and also the amide nitrogen is used to make amino sugars. So, glutamine uses that amide nitrogen for many different biosynthetic pathways. (that is just to introduce you to that because I’m going to tell you how it works for purines and pyrimadines. Page 12 of “Overview of Amino Acid Metabolism” packet. (Page has a 16 in top right corner.) Some Human Genetic Disorders Affecting Amino Acid Catabolism Inborn errors of metabolism almost always asked on boards. PKU. We’ve already discussed that the phenylalanine hydroxylase is mutated. Methylmalonic academia. Methylmalonyl-CoA mutase is the enzyme which requires B12. That is mutated. It’s not very prevalent. MSUD (Maple Syrup Urine Disease) Branched-chain ketoacid dehydrogenase complex is mutated. Homocystinuria Cystathionine beta-synthase is mutated. These 3 are enzymes in the urea cycle. All of them are almost always lethal. A kid never lives for more than 2-3 years because ammonia builds up. That is the thing that’s wrong with them. Ammonia builds up because the urea cycle is blocked. That is the hallmark of all these inborn errors involving urea cycle enzymes. Page 1 of “Biosynthesis of Urea” packet. (Page has a 10 in top right corner) Biosynthesis of Urea. B. The problem is most people get distracted by the intermediates of the urea cycle and they get all mad. Many of the intermediates and the enzymes in the urea cycle I’m not even going to talk about, I’ll just point at and say that these are things. Urea is a symmetrical molecule. It is going to be biosynthesized from ammonia, carbon dioxide and the amino nitrogen of aspartate. That is the origin of urea. C. (draws on board) NH4 O Asp C H2N NH2 I’ve got aspartate. First thing I have to do is generate ammonia. (one will come from ammonia and one will come from the amino nitrogen of aspartate) I have plenty of bicarbonate and CO2. How will I get my ammonia? Probably 2 reactions. o Glutamate dehydrogenase reaction run in this direction to create ammonia. o Glutaminase which hydrolyzes the amide nitrogen of glutamine to produce ammonia. If you look at glutaminase and glutamine synthetase (these are very active in the liver where urea biosynthesis occur) they form a buffering system for ammonia. If you want more ammonia 1 enzyme is activated. If you want less ammonia this enzyme is activated. So, you can meter out the amount of ammonia you need for urea biosynthesis. Ammonia is very toxic so you need a buffering system. You can’t just run a glutaminase or glutamate dehydrogenase in one reaction…in one way to create ammonia without having another way that can capture it. That enzyme is glutamine synthetase. How do we fix our ammonia? We use carbamoyl-phosphate synthetase. Which takes a CO2 and ammonia group in the presence of ATP and produces carbamoyl-phosphate. Page 2 of “Biosynthesis of Urea” packet. (Page has an 11 in top right corner) Here is our ammonia, here is our CO2. This is carbamoyl-phosphate synthetase. This will be then the carbon and one of the nitrogens of urea. So we’ve got 1 carbon and one Nitrogen of urea from CO2 and ammonia. The purpose of the urea cycle is to put one more nitrogen onto the urea molecule. This is the way it’s done. We’re going to transfer carbamoyl phosphate to ornithine and then we’re going to go through all this mess and we’re going to create an intermediate with spartate’s amino group on an intermediate. Finally we’re going to get arginine, we’re going to hydrolyze urea off arginine and regenerate ornithine. That’s all I want you to know. I don’t carea bout these intermediates. The global take-home message is that the only purpose of the urea cycle is to put final nitrogen on urea. Another conceptual thing students have problem with: I’m using the amino group of aspartate. What about all the other amino groups? You do all your transamination reactions. You want to generate that one? Use oxaloacetate, use glutamic acid get alphaketoglut. Transamination reactions allow this amino acid group on aspartate to come from almost all amino groups on other amino acids. So, it’s not just aspartate, it’s the last donor to the urea cycle but it’s not the only donor. Colorized version: Carbomoyl-phosphate condenses with ornithine then we have to add aspartate here, use the nitrogen from aspartate, make arginine, hydrolyze, get urea, regenerate ornithine. That’s all I want you to know about that. Page 1 of “One Carbon Metabolism” packet. (Page has an 11 in the top right corner.) Now for something that becomes a little more conceptually difficult. One-carbon metabolism. Especially folate 1-carbon metabolism. Tertrahydrofolate is a coenzyme that carries 1-carbon fragments. Also a coenzyme which allows one carbon to be oxidized or reduced. Tertrahydrofolate is composed of a pteridine ring, a paraaminobenzoic acid and a glutamic acid residue. In vivo there will be polyglutamates of this coenzyme. Poly-gamma-glutamates. In other words, the gamma carboxylic acid will be linked to the alpha-amino group of glutamic acid. What is the important place on this molecule? The 1 carbon fragment resides either on the 5-position, the 10-position, or as a bridge head on the 5 & 10 position. It carries a 1 carbon fragment. Page 2 of “One Carbon Metabolism” packet. (Page has a 1A in the top right corner.) Now it gets conceptually difficult because you have the 1 carbon fragments at various oxidation states. The 1 carbon fragment can be at the methyl, (which is the lowest oxidation state) methylene (intermediate or formal oxidation state). So let’s look at what these oxidation states do. What are we going to use the 1-carbon fragment carried by the tetrahydrofolate coenzyme for? Draws table 28-2 on board. “One-carbon groups carried by tetrahydrofolate” Methyl oxidation state has one “use” and one use only. We’re going to convert homocysteine (which is methionine without it’s methyl group) to methionine. Methylene oxidation state exists as a bridge-head between the 5 & 10. This is produced when we metabolize serine to glycine or when we cleave glycine to CO2 + ammonia. It wil also be used to convert deoxyUMP (dUMP; deoxyuridinemonophosphate) to deoxyTMP (deoxythymadinemonophosphate) Formyl group can be 5-formal, 10-formal, 5-10-methanyl, it can be formimino. (Methenyl, formimino, formyl are all the same oxidation states) We saw that when histidine is catabolized we created the 5-formimino. o The most important use of formal groups is the biosynthesis of purines. Here is where the conceptually difficult problem comes in: All of these forms are interconvertible except for one reaction. So I can go back and forth from any of these forms in here. All of these reactions are reversible. (So, I can take a methenyl and make it a methylene, can take a formyl and make a methylene, can take a methylene and make it a formyl, can take a formimino and go back and forth. Doesn’t have to be strictly reversible but can use pathways to get from one to the other. What we can’t do: is once this 1 carbon has been reduced from the methylene to the methyl state, this is irreversible. So you’ve got 5-methyl-THF. How do you get tetrahydrofolate back again? What reaction must you go through to get tetrahydrofolate back? You must take this and use it in methionine synthase to make methionine in order to regenerate tetrahydrofolate. In our body where does the equilibrium for all these reactions lie? Where is all of our folate pulled towards? Where is the predominate tetrahydrofolate in our body? 5-methylTHF. The equilibrium pulls everything in that general direction. That is the bottom line. Page 3 of “One Carbon Metabolism” packet. (Page has a 13 in the top right corner.) If you don’t like the previous bottom line…then study this page. Page 4 of “One Carbon Metabolism” packet. (Page has a 2A in the bottom left corner.) This actually tells you something. Notice the reversible arrows are a way to get from one to the other, except for one reaction: methylene being reduce to the methyl. Not a double headed arrow, just goes in one direction. Notice also we have serine going to glycine providing us with the major source of these 1 carbon fragments. Page 6 of “One Carbon Metabolism” packet. (Page has a 14 in the top right corner.) 2. i Now we’ve got to get that methyl group off of 5-methyltetrahydrofolate. The only way to do that is to convert homocysteine to methionine. 5-methylTHF comes in here and THF is spit out but we have a monkey wrench up here in this reaction. This reaction is tetrahydrofolate and B12 dependant reaction. You have to have methyl-cobalamine to run this reaction. Without vitamin B12 or methylcobalamine the reaction doesn’t go. If the reaction doesn’t go where will all the folates be trapped as? 5-methyl. This is like a sink, the equilibrium goes down to 5-methyl. I’m going to get all my folates trapped as a 5-methyl. This is the methyl trap hypothesis/theory of B12 deficiency. Without this, the reaction doesn’t go. The reaction doesn’t go and all the folates end up as 5-methyl. Can you use this (5-ch3-thf) to make dTMP? Does this make deoxyTMP? No. Does it make purines? No. I’ve got all my folates in a form that is useless for the biosynthesis of purines or deoxyTMP. That is why when I showed the bone marrow smears and the peripheral blood, that’s why B12 deficiency looks exactly the same as folate deficiency. It is a lack of purines and thymidilate. You technically do not have a deficiency of folate, you have a deficiency of folate in the form that is useful for biosynthesis of purines and thymidilate. So, your bone marrow and your peripheral blood look exactly like folate deficiency. So B12 and folate deficiency look the same because of this methyl trap hypothesis/theory. To treat B12 deficiency use cyanocobalamine, (which is a stable form of B12 that contains a cyano group and doesn’t contain a methyl group) you use such a small amount that we don’t worry about the toxicity of cyanide (and it will be injected). It is very difficult to treat people with malabsorption of B12 by feeding them B12 so almost always they will give an intramuscular injection. Page 5 of “One Carbon Metabolism” packet. (Page has a 3A in the top left corner.) This is the kind of stuff that will be on the test: Remember this cycle for creating homocysteine. We make S-Adenosylmethionine. SAdenosylmethionine then donates it’s methyl group to an acceptor. SAdenosylhomocysteine is then created, then we make homocysteine. In order to keep this cycle going we have to re-methylate homocysteine to methionine back here and around and around the cycle goes. Shown on bottom of page: S-Adenosylmethionine donates a methyl group, come back to homocysteine, remethylate, and around and around we go. Actually they determined how many times methionine is actually thrown around the cycle (realized homocysteine can be someplace else, it can be condensed with serine and produce cysteine and alphaketobutarate.) But, the methionine cycle and the S-Adenosylmethionine cycle, methionine used about 5-6 times before it is eventually catabolized. So, methionine is remethylated about 5-6 times in the cycle before carbon is metabolized. That completes the discussion of 1-carbon metabolism…